| Cardiology Research, ISSN 1923-2829 print, 1923-2837 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, Cardiol Res and Elmer Press Inc |
| Journal website https://www.cardiologyres.org |
Original Article
Volume 14, Number 5, October 2023, pages 342-350
Secondary Prevention of Cryptogenic Stroke and Outcomes Following Surgical Patent Foramen Ovale Closure Plus Medical Therapy vs. Medical Therapy Alone: An Umbrella Meta-Analysis of Eight Meta-Analyses Covering Seventeen Countries
Urvish Patela, p, q, Chetna Dengrib, p, David Pielykhc, Aakash Baskard, Muhammad Imtiaz Tare, Greshaben Patelf, Neel Patelg, Nishel Kotharih, Renui, Sri Abirami Selvamj, Amit Munshi Sharmak, Vikramaditya Samela Venkatal, Shamik Shahm, Syed Nazeer Mahmoodn, Appala Suman Peelao
aDepartment of Neurology and Public Health, Icahn School of Medicine at Mount Sinai, New York, NY 10029, USA
bDepartment of Neurology, Cleveland Clinic Florida, Weston, FL 33331, USA
cOdessa National Medical University, Valikhovskiy Lane 2, Odessa 65000, Ukraine
dK.A.P. Viswanatham Government Medical College, Musiri, Trichy, Tamilnadu 621006, India
eTouro University Nevada College of Osteopathic Medicine, Henderson, NV 89014, USA
fB.J. Medical College, Ahmedabad 380016, India
gDepartment of Public Health, Icahn School of Medicine at Mount Sinai, New York, NY 10029 USA
hDartmouth Hitchcock Medical Center, Lebanon, NH 03766, USA
iDepartment of Medicine, Sarojini Naidu Medical College, Agra, Uttar Pradesh 282003, India
jDepartment of Internal Medicine, St Mary Medical Center, Langhorne, PA 19047, USA
kDepartment of Medicine, Geisinger Commonwealth School of Medicine, Scranton, PA 18510, USA
lDepartment of Medicine, Cheshire Medical Center, Keene, NH 03431, USA
mDepartment of Neurology, Stormont Vail Health, Topeka, KS, USA
nDepartment of Medicine, Section of Pulmonary/Critical Care, MedStar Washington Hospital Center, Washington, DC 5333, USA
oDepartment of Family Medicine, UNC Health Southeastern, Lumberton, NC 28358, USA
pThese authors contributed equally to the article.
qCorresponding Author: Urvish Patel, Department of Neurology and Public Health, Icahn School of Medicine at Mount Sinai, New York, NY 10029, USA
Manuscript submitted June 19, 2023, accepted August 9, 2023, published online October 12, 2023
Short title: CS and Outcomes Following Therapy
doi: https://doi.org/10.14740/cr1526
| Abstract | ▴Top |
Background: Cryptogenic stroke (CS) is an exclusion diagnosis that accounts for 10-40% of all ischemic strokes. Patent foramen ovale (PFO) is found in 66% of patients with CS, while having a prevalence of 25-30% in the general population. The primary aim was to evaluate the risk of recurrent stroke following surgical PFO closure plus medical therapy vs. medical therapy alone amongst CS, an embolic stroke of undetermined source (ESUS), or transient ischemic attack (TIA). The secondary aim was to evaluate new-onset non-valvular atrial fibrillation, mortality, and major bleeding.
Methods: We conducted an umbrella meta-analysis using PRISMA guidelines on English studies comparing surgical PFO closure plus medical therapy versus medical therapy alone for managing CS. We extracted data on interventions and outcomes and used random-effects models with generic inverse variance to calculate relative risks (RRs) with 95% confidence intervals for outcome calculations.
Results: A comprehensive search yielded 54,729 articles on CS and 65,001 on surgical PFO closure, with 1,591 studies focusing on PFO closure and medical therapy for secondary CS, ESUS, or TIA prevention. After excluding non-meta-analyses, 52 eligible meta-analyses were identified, and eight studies were selected for outcome evaluation, excluding non-English, non-human, and studies before January 2019 as of August 31, 2021. Among a total of 41,880 patients, 14,942 received PFO closure + medical therapy, while 26,938 patients received medical therapy alone. Our umbrella meta-analysis showed that PFO closure plus medical therapy had a 64% lower risk of recurrent strokes than medical therapy alone (pooled RR: 0.36). PFO closure plus medical therapy was associated with 4.94 times higher risk of atrial fibrillation. There was no difference in the risk of death or bleeding between both groups.
Conclusion: In patients with CS, PFO closure, in addition to medical therapy, reduces the risk of recurrence. More research is needed to assess the efficacy of early closure as well as specific risk profiles that would benefit from early intervention to reduce the burden of stroke.
Keywords: PFO closure; Cryptogenic shock; TIA; Atrial fibrillation; Meta-analysis
| Introduction | ▴Top |
The incidence of strokes in the United States is approximately 795,000/year [1]. Stroke is the second leading cause of death worldwide, accounting for 11.8% of deaths, and is associated with significant mortality. Acute ischemic stroke (AIS) is the fifth leading cause of death in the United States. AIS is caused by cardiovascular embolism, large vessel atherosclerosis, and small vessel disease. Up to 10% to 40% of all symptomatic ischemic strokes lack a well-defined etiology, and this subgroup is referred to as cryptogenic stroke (CS) [2-5].
The diagnosis of CS is made when the stroke cannot be attributed to any known causes of AIS, including cardio-embolism, large vessel atherosclerosis or small artery disease, despite a comprehensive workup [6, 7]. CS is more common in younger patients (< 55 years of age) and may occur due to intracardiac shunts, occult atrial fibrillation (AF), and aortic atherosclerosis [8]. Among all these causes, patent foramen ovale (PFO) is very commonly seen in patients with CS [9]. The prevalence of PFO in the general population is nearly 25-30% but is much greater in CS patients (66%) [10, 11]. The proposed mechanism in PFO patients is a paradoxical embolism, in which the thrombus moves from venous to systemic circulation via the PFO.
Patients are at increased risk for recurrent strokes after the first episode of CS, and therefore secondary prevention is crucial. The common therapies for managing PFO are percutaneous device closure and medical therapy (antiplatelet and/or anticoagulant drugs). A long-standing debate about the best strategy to manage PFO patients after a CS comparing transcatheter PFO closure versus medical therapy showed conflicting results [12, 13]. In the Risk of Paradoxical Embolism (RoPE) study, an index scoring system was proposed to determine whether the PFO was caused by a stroke or an unexpected event [8]. The RoPE score was proposed in patients of all ages with a score ranging from 0 to 10; a higher score indicates a greater likelihood that the stroke is secondary to a PFO. Kotoor et al reported that PFO closure could be considered the primary treatment for people with PFO and those taking aspirin and an elevated RoPE score [8]. Studies also indicate that anticoagulant therapy could have a substantial advantage in managing a CS compared to antiplatelet treatment alone and that anticoagulant therapy could be nearly as efficient as the closure of PFO [14-19]. A significant complication with PFO closure is AF [8]. However, this procedure-induced AF has been reported as being brief and, therefore, would not be sufficient to cause cardio-embolism [8].
Several randomized controlled trials (RCTs) compared the effectiveness of PFO closure and medical therapy versus medical therapy alone to prevent secondary stroke, but the findings are conflicting [14, 15, 17]. Several meta-analyses have produced varying results, some demonstrating possible borderline advantages of PFO closure and others indicating no benefit depending on how the assessment should be carried out [20-23]. In an attempt to resolve uncertainty concerning the appropriate therapy of CS in the presence of PFO and to evaluate the variability between different PFO closing mechanisms and AF, we performed an updated systematic review and umbrella meta-analysis to examine long-term clinical results with PFO closure with medical therapy versus medical therapy alone.
| Materials and Methods | ▴Top |
Endpoint
Our study’s main aim was to compare the risk of recurrent stroke in patients with CS, embolic stroke of undetermined source (ESUS), or transient ischemic attack (TIA) who had surgical PFO closure combined with medical therapy to patients who received medical treatment only. A secondary aim of this study was to evaluate new-onset non-valvular AF, mortality, and major bleeding (gastrointestinal (GI) bleeding, serious bleeding, fatal bleeding, thrombolysis in myocardial infarction (TIMI)-defined major bleeding, and hemorrhagic stroke) following both interventions. Study-specific definitions are mentioned in Table 1 [24-31].
 Click to view | Table 1. Study Characteristics Showing Meta-Analyses Comparing Surgical PFO Closure Plus Medical Therapy vs. Medical Therapy Alone as the Management of Cryptogenic Shock |
Search strategy and selection criteria
We performed an umbrella meta-analysis using previously published meta-analysis (studies) using PRISMA guidelines from January 1, 2019 to August 31, 2021. We used PubMed for finding out a meta-analysis comparing surgical PFO closure plus medical therapy vs. medical therapy alone as the management of CS. We used following keywords to identify the literature: ((((((((Cryptogenic stroke[Title/Abstract]) OR (Cryptogenic Embolism Strokes[Title/Abstract])) OR (Cryptogenic Ischemic Strokes[Title/Abstract])) OR (Cryptogenic Embolism[Title/Abstract])) OR (embolic stroke of undetermined significance[Title/Abstract])) OR (embolic stroke of undetermined origin[Title/Abstract])) OR (ischemic stroke[Title/Abstract])) OR (embolic stroke[Title/Abstract])) OR (non-cardioembolic stroke[Title/Abstract]) AND ((((((((surgical PFO closure[Title/Abstract]) OR (medical treatment[Title/Abstract])) OR (surgical PFO closure plus medical treatment vs medical therapy alone[Title/Abstract])) OR (Platelet Aggregation Inhibitors[Title/Abstract])) OR (Patent Foramen Ovale closure[Title/Abstract])) OR (Septal Occluder Device[Title/Abstract])) OR (Combined Modality Therapy[Title/Abstract])) OR (Patent Foramen Ovale Closure[Title/Abstract])) OR (Antiplatelet Therapy[Title/Abstract].
Study selection
All studies were identified using the search strategy described above and independently screened for eligibility by Chetna Dengri and Nishel Kothari, with any disagreement resolved through discussion with UP and NP. For full-text review, studies describing meta-analyses of clinical trials or observational studies were considered. PRISMA flow diagram of study selection is depicted in Figure 1.
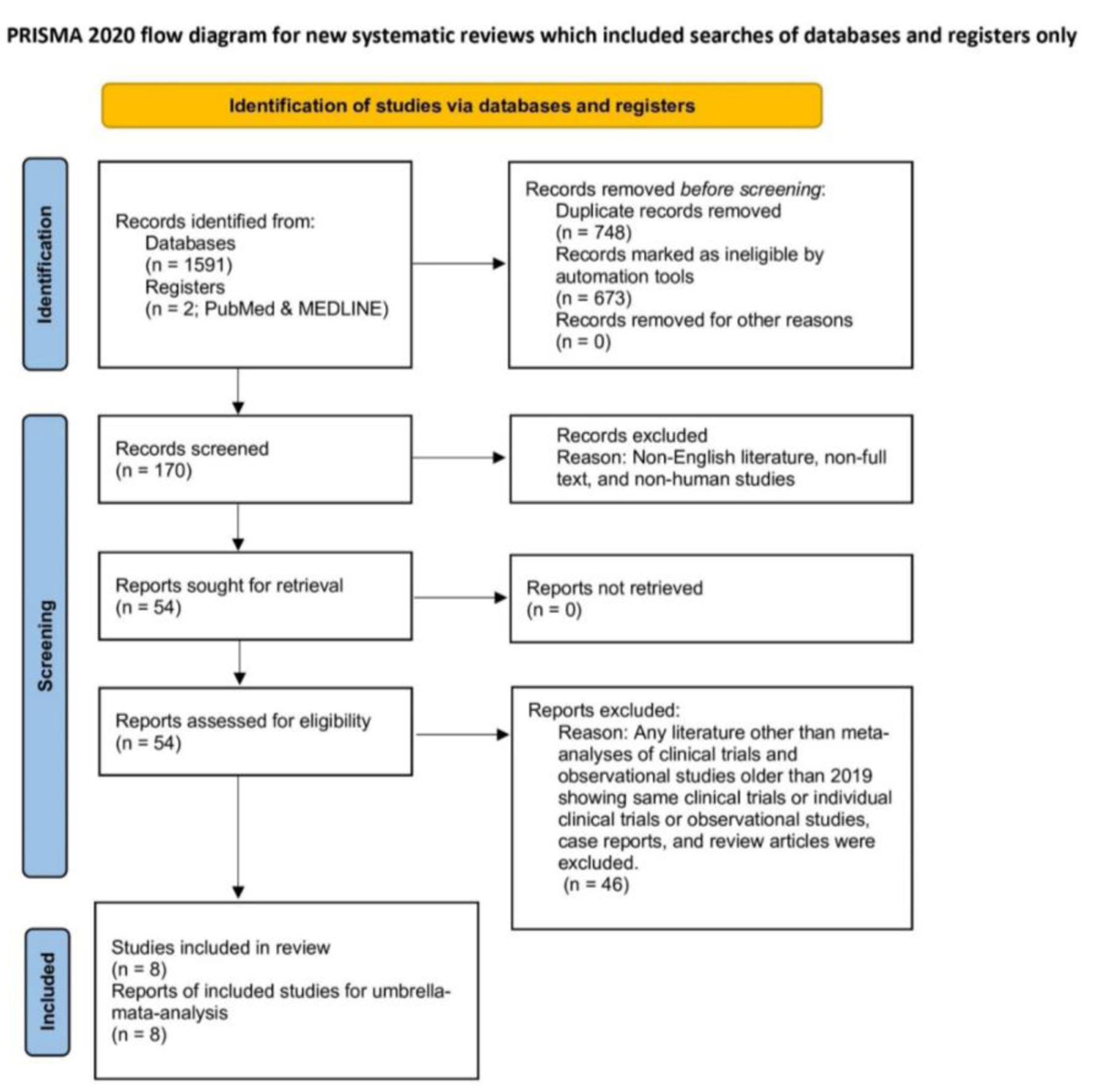 Click for large image | Figure 1. PRISMA flow diagram of study selection. |
Data extraction and quality assessment
The included studies’ data were gathered using a data extraction form to evaluate the literature synthesis. After consulting with UP and NP, the data extraction form was created (Table 1).
Extracted information included: study setting (study name, year of publication, and country), study design, study population demographics (mean/median age and sex%), sample size, details on CS (type of stroke), details of the intervention and control, outcomes following intervention and control, and information for the assessment of the risk of bias (using Newcastle-Ottawa Scale (NOS)).
Statistical analysis
We performed an umbrella meta-analysis using Review Manager V.5.4 (The Nordic Cochrane Centre, The Cochrane Collaboration, Copen-Hagen, Denmark). Data on interventions and outcomes with relative risks (RRs) were extracted, and for individual meta-analysis, we calculated log RRs from each outcome. The generic inverse variance was used to calculate and obtain pooled RRs from log RR along with its 95% confidence interval (CI) to describe the outcome comparison between surgical PFO closure + medical treatment vs. medical therapy alone. Random-effect models were used regardless of heterogeneity to estimate the combined effect. P-value < 0.05 was considered significant. The results were presented in forest plots for individual outcomes. To evaluate heterogeneity, we used I2 statistics, and > 50% was considered significant heterogeneity. In situations with high heterogeneity, funnel plots (Supplementary Material 1, www.cardiologyres.org) were used for sensitivity analysis using the leave-one-out method. Publication bias was assessed individually, and overall study bias was described using the NOS (Supplementary Material 2, www.cardiologyres.org).
Human subjects were not involved so no informed consent or IRB approval was needed.
| Results | ▴Top |
We screened 54,729 and 65,001 articles on CS and surgical PFO closure, respectively. Out of these, 1,591 studies had details on PFO closure and medical therapy in the management of secondary CS, ESUS, or TIA prevention. After excluding studies other than meta-analysis, we found 52 meta-analyses fitting in the eligibility for the data collection. After a detailed assessment, as of August 31, 2021, a total of eight meta-analysis studies were selected to evaluate the outcomes. Studies before January 2019, non-human and non-English studies were excluded (Fig. 1). Among a total of 41,880 patients, 14,942 received PFO closure + medical therapy, while 26,938 patients received medical therapy alone (Table 1).
Primary outcome
Reduction of recurrent stroke or TIA
We found eight meta-analyses out of 1,591 studies that evaluated the effect of interventions on the reduction of CS, recurrent stroke, or TIA. Our meta-analysis found that patients who received PFO closure and medical therapy had a 64% lower risk of recurrent strokes than those who received only medical therapy (pooled RR: 0.36; 95% CI: 0.29 - 0.46; P < 0.00001). There was no heterogeneity (I2 = 0%; P = 0.64), and the overall risk of bias was low (Fig. 2).
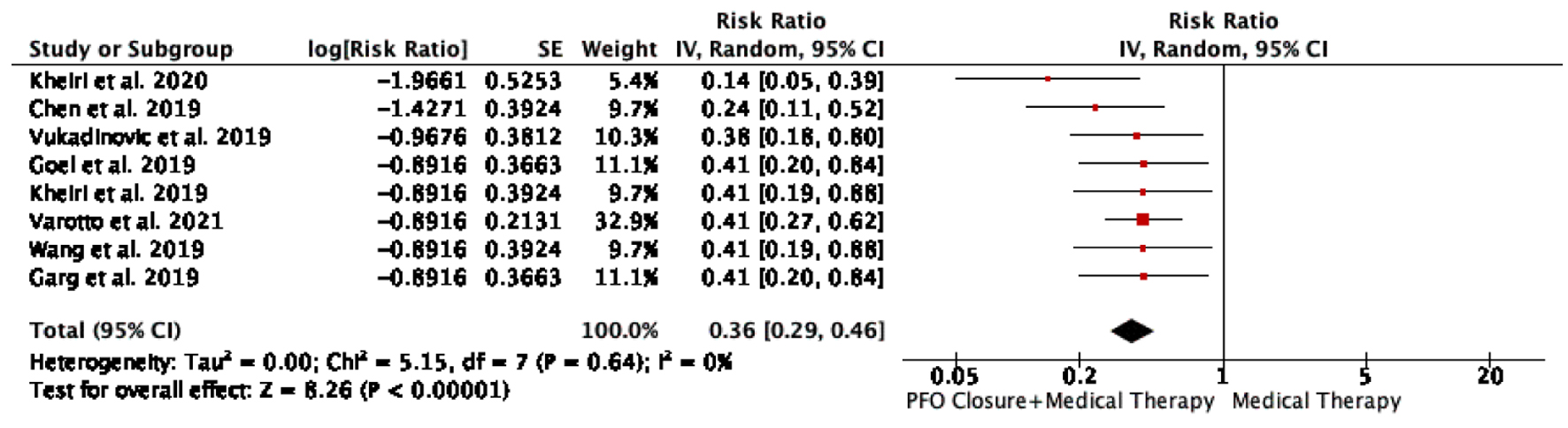 Click for large image | Figure 2. Recurrent stroke or TIA in patients with PFO closure plus medical therapy vs. medical therapy alone. PFO: patent foramen ovale; TIA: transient ischemic attack. |
Secondary outcomes
Mortality
Four meta-analyses reporting all-cause mortality were included. We found PFO closure plus medical therapy was associated with a 0.73 times lower risk of death (pooled RR: 0.73; 95% CI: 0.50 - 1.07; P = 0.10) compared to medical therapy alone. The heterogeneity was 0% (P = 1.00) (Fig. 3).
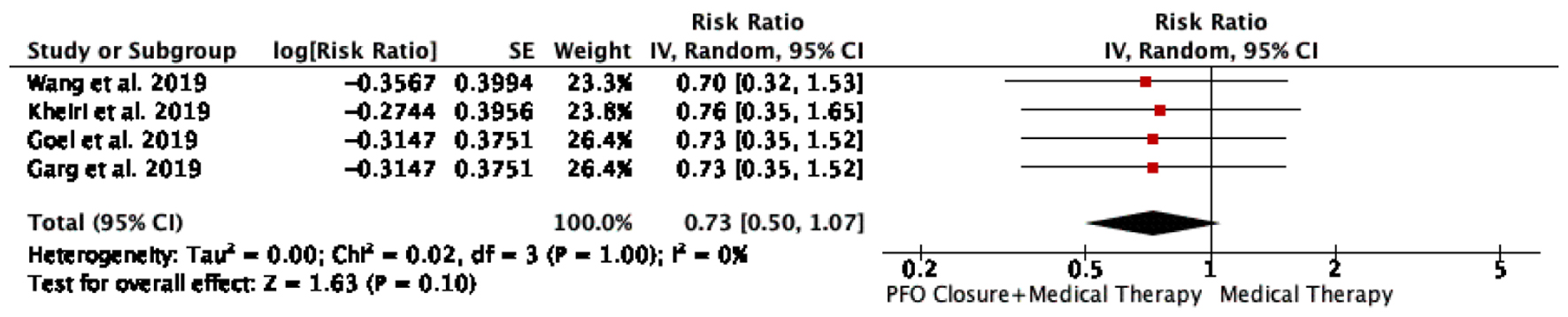 Click for large image | Figure 3. All-cause mortality in patients with PFO closure plus medical therapy vs. medical therapy alone. PFO: patent foramen ovale. |
Major bleeding
Five meta-analyses reported major bleeding as a complication. In our study, PFO closure plus medical therapy was associated with a 0.88 times lower risk of bleeding (pooled RR: 0.88; 95% CI: 0.65 - 1.19; P = 0.41) compared to medical therapy alone. The heterogeneity was 0% (P = 0.98) (Fig. 4).
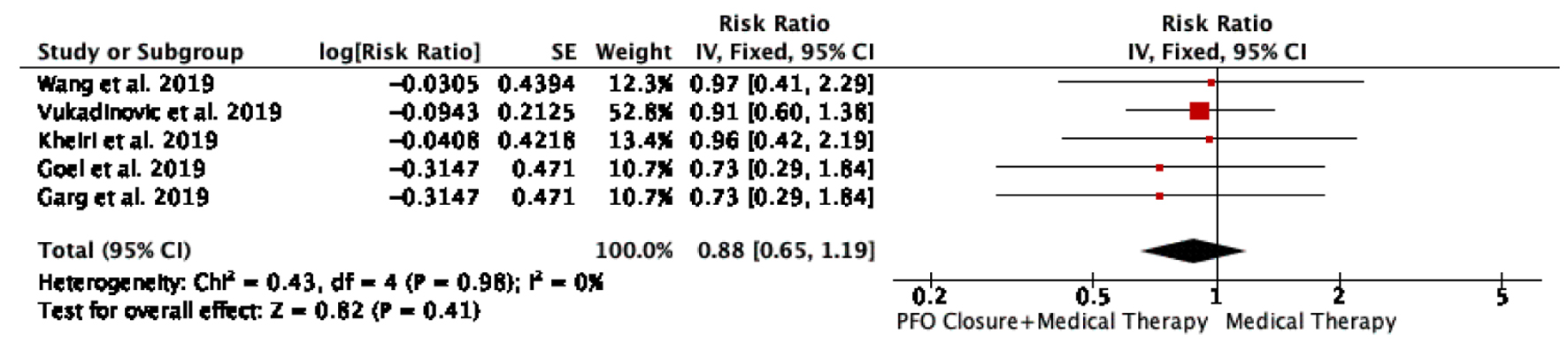 Click for large image | Figure 4. Major bleeding in patients with PFO closure plus medical therapy vs. medical therapy alone. PFO: patent foramen ovale. |
AF (new-onset or pre-existing AF)
Seven meta-analyses reported AF as a complication. We found that PFO closure plus medical therapy was associated with a 4.94 times higher risk of AF (pooled RR: 4.94; 95% CI: 3.74 - 6.53; P < 0.00001) in comparison with medical therapy alone. The heterogeneity was 0% (P = 0.99) (Fig. 5).
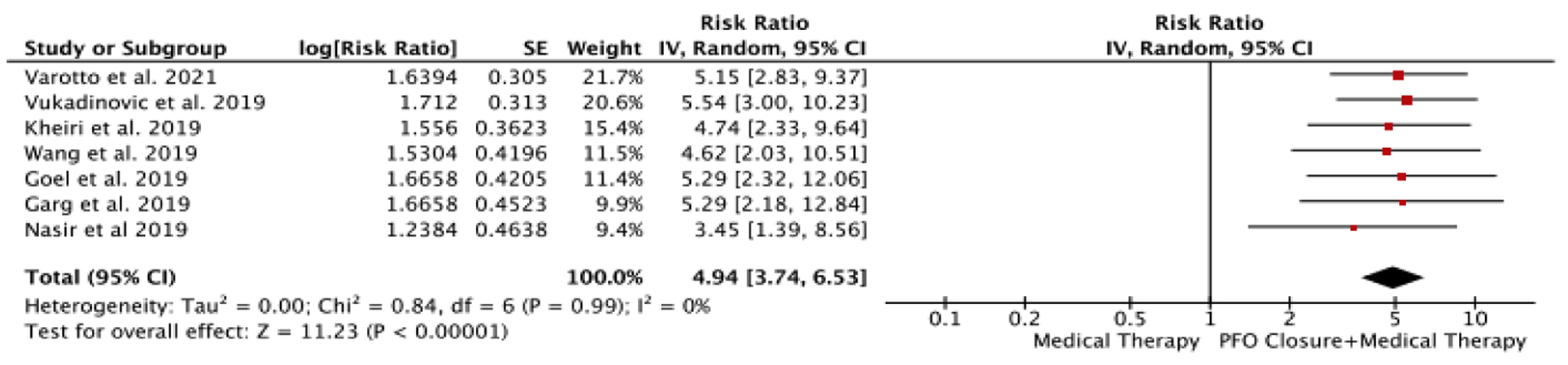 Click for large image | Figure 5. Atrial fibrillation (new onset or pre-existing) in patients with PFO closure plus medical therapy vs. medical therapy alone. PFO: patent foramen ovale. |
| Discussion | ▴Top |
Our meta-analysis of eight studies found that patients with PFO closure and medical therapy had a lower risk of recurrent stroke than those with medical therapy alone. The RR of recurrent stroke/TIA was 64% lower in those treated with PFO closure and medical therapy than in those treated only with medical therapy. The risk of poor composite outcomes was also lower in the group managed with PFO closure along with medical therapy. However, there was no difference in mortality or major bleeding between both groups. Antiplatelet and anticoagulation as medical therapy have both been studied individually and in combination as medical management for CS. Previous studies have suggested the benefits of oral anticoagulation over antiplatelet medications for the secondary prevention of PFO-related CS [23], but current guidelines prefer using antiplatelets alone [32, 33]. The majority of patients in the medical therapy group in the included studies received antiplatelet therapy, primarily aspirin followed by clopidogrel, with a minority receiving anticoagulation with vitamin-K antagonists. The administration of these drugs to patients was not standardized across trials or within trials, but was left to the discretion of the investigators, and event rates across different therapy regimens were not recorded. As a result, estimating whether there was a significant difference in events of interest across different medical therapy regimens compared to the interventional closure group was impossible [26].
In our meta-analysis, new-onset AF was found to be significantly associated with PFO closure. PFO closure and medical therapy patients had a 4.94-fold higher risk of AF than medical therapy alone. The device trigger is the most likely etiology for the higher incidence of AF in device closure. Given the difficulty in diagnosing paroxysmal AF, the possibility of having AF prior to device implantation cannot be ruled out or ignored. This could explain why the PFO closure group has a higher rate of AF. This argument is supported by the RESPECT trial findings, which excluded paroxysmal AF and found no difference in AF rates between the two groups (0.6% in both surgical closure and medical therapy group) [28]. The majority of the AF episodes were peri-procedural, with very little persistent or long-term AF. Post-implant AF typically occurred within 45 days of PFO closure and was noted to be transient, resolving spontaneously in the majority of cases but requiring electrical or pharmacological cardioversion in a few cases. Only a small percentage of all AF or atrial flutter reported after PFO closure progressed to permanent AF [14]. While AF is an independent risk factor for embolic strokes, long-term RCTs have not shown an increased incidence of strokes following device closures. The absence of prolonged cardiac monitoring for subclinical AF detection in patients with CS is a common limitation in previous trials. Although occult AF is uncommon among patients with < 60 years of age with CS [34], based on observational studies, the American Heart Association/American Stroke Association guidelines for stroke prevention recommend at least 30 days of cardiac monitoring in patients with no obvious cause of stroke/TIA to detect occult AF [14, 33]. A previous RCT (CRYSTAL AF) has supported prolonged cardiac monitoring, and the results showed that AF was more frequently detected in patients with recent CS (12.4% detection rate in the monitored group vs. 2% in the unmonitored group; HR 7.3; 95% CI: 2.6 - 20.8; P < 0.001) [15]. Furthermore, a meta-analysis of RCTs found that prolonged cardiac monitoring improved detection of AF after CS/TIA [17]. Therefore, even in the presence of PFO, AF should be considered as a potential cause of some presumptive CSs.
Strengths and limitations
As far as we know, this is the first umbrella meta-analysis conducted on this topic. Our analysis includes multiple RCTs and observational studies from various countries, which is a strength of this study. A noteworthy strength of this meta-analysis is that it had no significant heterogeneity. However, the inclusion of overlapping RCTs could lead to an overestimation of the results. Furthermore, the study does not comment on the severity of stroke, disability, or outcome on follow-up. Our meta-analysis has several limitations that need to be considered. Firstly, it relies on aggregated data from various trials, which means it inherits the limitations present in the individual studies included. Another limitation is the overlap of RCTs used in the analysis. Secondly, the majority of RCTs experienced slow enrollment over several decades and had varying follow-up periods. This leads to challenges in comparing the initial phase data with more recent data due to changes in clinical practices and device advancements over time. Thirdly, the absence of patient-level data prevents the possibility of conducting further analyses that could adjust for potential confounding variables or perform stratified analyses. Furthermore, the study does not provide insights into the severity of stroke, disability, or long-term outcomes, which restricts the conclusions that can be drawn from this research. Fourthly, different types of PFO devices were used across the trials, necessitating the consideration of each device’s efficacy and safety when interpreting the results. Additionally, the inability of some studies in the meta-analysis to classify strokes as minor or major poses a limitation in the categorization of stroke severity. Lastly, the varying medical therapy strategies permitted in the trials could have influenced the final outcomes within each individual study and across all RCTs. This factor should be considered while interpreting the overall findings.
Conclusion
In our meta-analysis, we discovered that surgical closure of the PFO not only reduced the risk of recurrent stroke, but was also safer with respect to mortality and bleeding risk in patients with CS. Given the greater benefits of PFO closure in addition to medical therapy, more research is needed to assess the efficacy of early closure and specific risk profiles that would benefit from early intervention to reduce the burden of stroke. More studies should evaluate the risk benefit profile of PFO closure in patients with pre-existing or at risk of AF as our study shows a significant relationship between PFO surgical closure and AF.
| Supplementary Material | ▴Top |
Suppl 1. Funnel plots.
Suppl 2. Risk of bias of included studies.
Acknowledgments
None to declare.
Financial Disclosure
None to declare.
Conflict of Interest
The authors declare that there is no conflict of interest.
Informed Consent
Not applicable.
Author Contributions
Conceptualization: Urvish Patel, Chetna Dengri, Appala Suman Peela. Methodology: Urvish Patel, Shamik Shah, Syed Nazeer Mahmood. Acquisition of data: Chetna Dengri, David Pielykh, Aakash Baskar, Muhammad Imtiaz Tar, Greshaben Patel, Neel Patel. Software: Urvish Patel, Chetna Dengri, David Pielykh. Formal analysis and investigation: Urvish Patel, Chetna Dengri, David Pielykh, Aakash Baskar, Muhammad Imtiaz Tar, Greshaben Patel, Nishel Kothari, Neel Patel, Renu, Sri Abirami Selvam. Resources: Shamik Shah, Syed Nazeer Mahmood, Appala Suman Peela. Validation: Amit Munshi Sharma, Vikramaditya Samela Venkata, Shamik Shah, Syed Nazeer Mahmood, Appala Suman Peela, Neel Patel. Data Curation: Chetna Dengri, David Pielykh, Aakash Baskar, Muhammad Imtiaz Tar, Neel Patel. Writing - original draft preparation: Chetna Dengri, Nishel Kothari, Neel Patel, Renu. Writing - review, critical feedback, and editing: Urvish Patel, Sri Abirami Selvam, Amit Munshi Sharma, Vikramaditya Samela Venkata, Shamik Shah, Syed Nazeer Mahmood, Appala Suman Peela, Neel Patel. Visualization: Urvish Patel, Chetna Dengri, Neel Patel. Project administration: Chetna Dengri, Neel Patel. Supervision: Urvish Patel, Appala Suman Peela.
Data Availability
The data are collected from the studies published online, publicly available, and specific details related to data and/or analysis will be made available upon request.
| References | ▴Top |
- Writing Group Members, Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, et al. Heart disease and stroke statistics-2016 update: a report from the American Heart Association. Circulation. 2016;133(4):e38-360.
doi pubmed - Saver JL. Clinical practice. Cryptogenic stroke. N Engl J Med. 2016;374(21):2065-2074.
doi pubmed - Sacco RL, Ellenberg JH, Mohr JP, Tatemichi TK, Hier DB, Price TR, Wolf PA. Infarcts of undetermined cause: the NINCDS Stroke Data Bank. Ann Neurol. 1989;25(4):382-390.
doi pubmed - Li L, Yiin GS, Geraghty OC, Schulz UG, Kuker W, Mehta Z, Rothwell PM, et al. Incidence, outcome, risk factors, and long-term prognosis of cryptogenic transient ischaemic attack and ischaemic stroke: a population-based study. Lancet Neurol. 2015;14(9):903-913.
doi pubmed pmc - Ji R, Schwamm LH, Pervez MA, Singhal AB. Ischemic stroke and transient ischemic attack in young adults: risk factors, diagnostic yield, neuroimaging, and thrombolysis. JAMA Neurol. 2013;70(1):51-57.
doi pubmed - Melkumova E, Thaler DE. Cryptogenic stroke and patent foramen ovale risk assessment. Interv Cardiol Clin. 2017;6(4):487-493.
doi pubmed - Finsterer J. Management of cryptogenic stroke. Acta Neurol Belg. 2010;110(2):135-147.
pubmed - Kottoor SJ, Arora RR. Cryptogenic stroke: to close a patent foramen ovale or not to close? J Cent Nerv Syst Dis. 2018;10:1179573518819476.
doi pubmed pmc - Overell JR, Bone I, Lees KR. Interatrial septal abnormalities and stroke: a meta-analysis of case-control studies. Neurology. 2000;55(8):1172-1179.
doi pubmed - Meissner I, Whisnant JP, Khandheria BK, Spittell PC, O'Fallon WM, Pascoe RD, Enriquez-Sarano M, et al. Prevalence of potential risk factors for stroke assessed by transesophageal echocardiography and carotid ultrasonography: the SPARC study. Stroke Prevention: Assessment of Risk in a Community. Mayo Clin Proc. 1999;74(9):862-869.
doi pubmed - Khairy P, O'Donnell CP, Landzberg MJ. Transcatheter closure versus medical therapy of patent foramen ovale and presumed paradoxical thromboemboli: a systematic review. Ann Intern Med. 2003;139(9):753-760.
doi pubmed - Wahl A, Juni P, Mono ML, Kalesan B, Praz F, Geister L, Raber L, et al. Long-term propensity score-matched comparison of percutaneous closure of patent foramen ovale with medical treatment after paradoxical embolism. Circulation. 2012;125(6):803-812.
doi pubmed - Agarwal S, Bajaj NS, Kumbhani DJ, Tuzcu EM, Kapadia SR. Meta-analysis of transcatheter closure versus medical therapy for patent foramen ovale in prevention of recurrent neurological events after presumed paradoxical embolism. JACC Cardiovasc Interv. 2012;5(7):777-789.
doi pubmed - Furlan AJ, Reisman M, Massaro J, Mauri L, Adams H, Albers GW, Felberg R, et al. Closure or medical therapy for cryptogenic stroke with patent foramen ovale. N Engl J Med. 2012;366(11):991-999.
doi pubmed - Meier B, Kalesan B, Mattle HP, Khattab AA, Hildick-Smith D, Dudek D, Andersen G, et al. Percutaneous closure of patent foramen ovale in cryptogenic embolism. N Engl J Med. 2013;368(12):1083-1091.
doi pubmed - Saver JL, Carroll JD, Thaler DE, Smalling RW, MacDonald LA, Marks DS, Tirschwell DL, et al. Long-term outcomes of patent foramen ovale closure or medical therapy after stroke. N Engl J Med. 2017;377(11):1022-1032.
doi pubmed - Carroll JD, Saver JL, Thaler DE, Smalling RW, Berry S, MacDonald LA, Marks DS, et al. Closure of patent foramen ovale versus medical therapy after cryptogenic stroke. N Engl J Med. 2013;368(12):1092-1100.
doi pubmed - Mas JL, Derumeaux G, Guillon B, Massardier E, Hosseini H, Mechtouff L, Arquizan C, et al. Patent foramen ovale closure or anticoagulation vs. antiplatelets after stroke. N Engl J Med. 2017;377(11):1011-1021.
doi pubmed - Sondergaard L, Kasner SE, Rhodes JF, Andersen G, Iversen HK, Nielsen-Kudsk JE, Settergren M, et al. Patent foramen ovale closure or antiplatelet therapy for cryptogenic stroke. N Engl J Med. 2017;377(11):1033-1042.
doi pubmed - Kitsios GD, Thaler DE, Kent DM. Potentially large yet uncertain benefits: a meta-analysis of patent foramen ovale closure trials. Stroke. 2013;44(9):2640-2643.
doi pubmed pmc - Li J, Liu J, Liu M, Zhang S, Hao Z, Zhang J, Zhang C. Closure versus medical therapy for preventing recurrent stroke in patients with patent foramen ovale and a history of cryptogenic stroke or transient ischemic attack. Cochrane Database Syst Rev. 2015;2015(9):CD009938.
doi pubmed pmc - Stortecky S, da Costa BR, Mattle HP, Carroll J, Hornung M, Sievert H, Trelle S, et al. Percutaneous closure of patent foramen ovale in patients with cryptogenic embolism: a network meta-analysis. Eur Heart J. 2015;36(2):120-128.
doi pubmed - Kent DM, Dahabreh IJ, Ruthazer R, Furlan AJ, Reisman M, Carroll JD, Saver JL, et al. Device closure of patent foramen ovale after stroke: pooled analysis of completed randomized trials. J Am Coll Cardiol. 2016;67(8):907-917.
doi pubmed pmc - Varotto L, Bregolin G, Paccanaro M, De Boni A, Bonanno C, Perini F. The closure of patent foramen ovale in preventing subsequent neurological events: a bayesian network meta-analysis to identify the best device. Cerebrovasc Dis. 2020;49(2):124-134.
doi pubmed - Wang TKM, Wang MTM, Ruygrok P. Patent foramen ovale closure versus medical therapy for cryptogenic stroke: meta-analysis of randomised trials. Heart Lung Circ. 2019;28(4):623-631.
doi pubmed - Vukadinovic D, Schirmer SH, Vukadinovic AN, Ukena C, Scheller B, Mahfoud F, Bohm M. Interventional closure vs. medical therapy of patent foramen ovale for secondary prevention of stroke: updated meta-analysis. Clin Res Cardiol. 2019;108(2):157-166.
doi pubmed - Kheiri B, Abdalla A, Osman M, Ahmed S, Hassan M, Bachuwa G. Patent foramen ovale closure versus medical therapy after cryptogenic stroke: An updated meta-analysis of all randomized clinical trials. Cardiol J. 2019;26(1):47-55.
doi pubmed pmc - Goel S, Patel S, Zakin E, Pasam RT, Gotesman J, Malik BA, Ayzenberg S, et al. Patent foramen ovale closure versus medical therapy for cryptogenic stroke: An updated systematic review and meta-analysis. Indian Heart J. 2019;71(6):446-453.
doi pubmed pmc - Nasir UB, Qureshi WT, Jogu H, Wolfe E, Dutta A, Majeed CN, Tan WA. Updated meta-analysis of closure of patent foramen ovale versus medical therapy after cryptogenic stroke. Cardiovasc Revasc Med. 2019;20(3):187-193.
doi pubmed - Garg A, Thawabi M, Rout A, Sossou C, Cohen M, Kostis JB. Recurrent stroke reduction with patent foramen ovale closure versus medical therapy based on patent foramen ovale characteristics: a meta-analysis of randomized controlled trials. Cardiology. 2019;144(1-2):40-49.
doi pubmed - Kheiri B, Simpson TF, Osman M, Golwala H, Radaideh Q, Dalouk K, Stecker EC, et al. Meta-analysis of secondary prevention of cryptogenic stroke. Cardiovasc Revasc Med. 2020;21(10):1285-1290.
doi pubmed - Hart RG, Catanese L, Perera KS, Ntaios G, Connolly SJ. Embolic stroke of undetermined source: a systematic review and clinical update. Stroke. 2017;48(4):867-872.
doi pubmed - Hart RG, Diener HC, Coutts SB, Easton JD, Granger CB, O'Donnell MJ, Sacco RL, et al. Embolic strokes of undetermined source: the case for a new clinical construct. Lancet Neurol. 2014;13(4):429-438.
doi pubmed - Homma S, Di Tullio MR. Patent foramen ovale and stroke. J Cardiol. 2010;56(2):134-141.
doi pubmed pmc
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cardiology Research is published by Elmer Press Inc.


