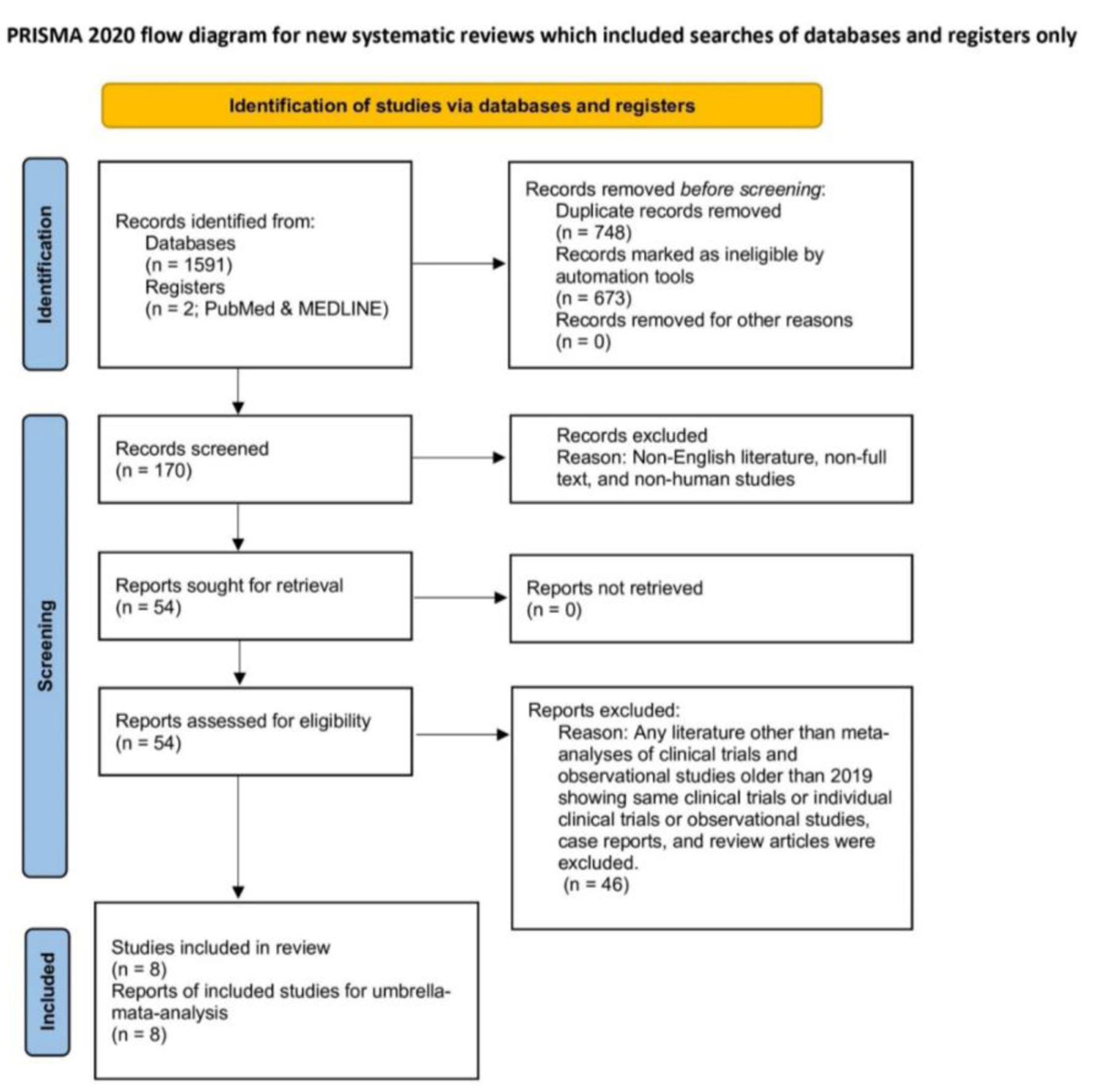
Figure 1. PRISMA flow diagram of study selection.
| Cardiology Research, ISSN 1923-2829 print, 1923-2837 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, Cardiol Res and Elmer Press Inc |
| Journal website https://www.cardiologyres.org |
Original Article
Volume 14, Number 5, October 2023, pages 342-350
Secondary Prevention of Cryptogenic Stroke and Outcomes Following Surgical Patent Foramen Ovale Closure Plus Medical Therapy vs. Medical Therapy Alone: An Umbrella Meta-Analysis of Eight Meta-Analyses Covering Seventeen Countries
Figures
Table
| Study, year | Study period | Study design | Population diagnosis | Mean/median age in years | Male (%) | Studies in meta-analysis | Total sample size | PFO closure + medical therapy vs. medical therapy alone (intervention or comparison) | Outcomes and effect measures |
|---|---|---|---|---|---|---|---|---|---|
| Countries of the RCTs or observational studies: France, Germany, US, Canada, United Kingdom, Denmark, Finland, Norway, Sweden, Austria, Belgium, Poland, Slovakia, Switzerland, Brazil, Australia, South Korea. PFO: patent foramen ovale; RCTs: randomized controlled trials; TIA: transient ischemic attack; HR: hazard ratio; RR: relative risk; OR: odds ratio. | |||||||||
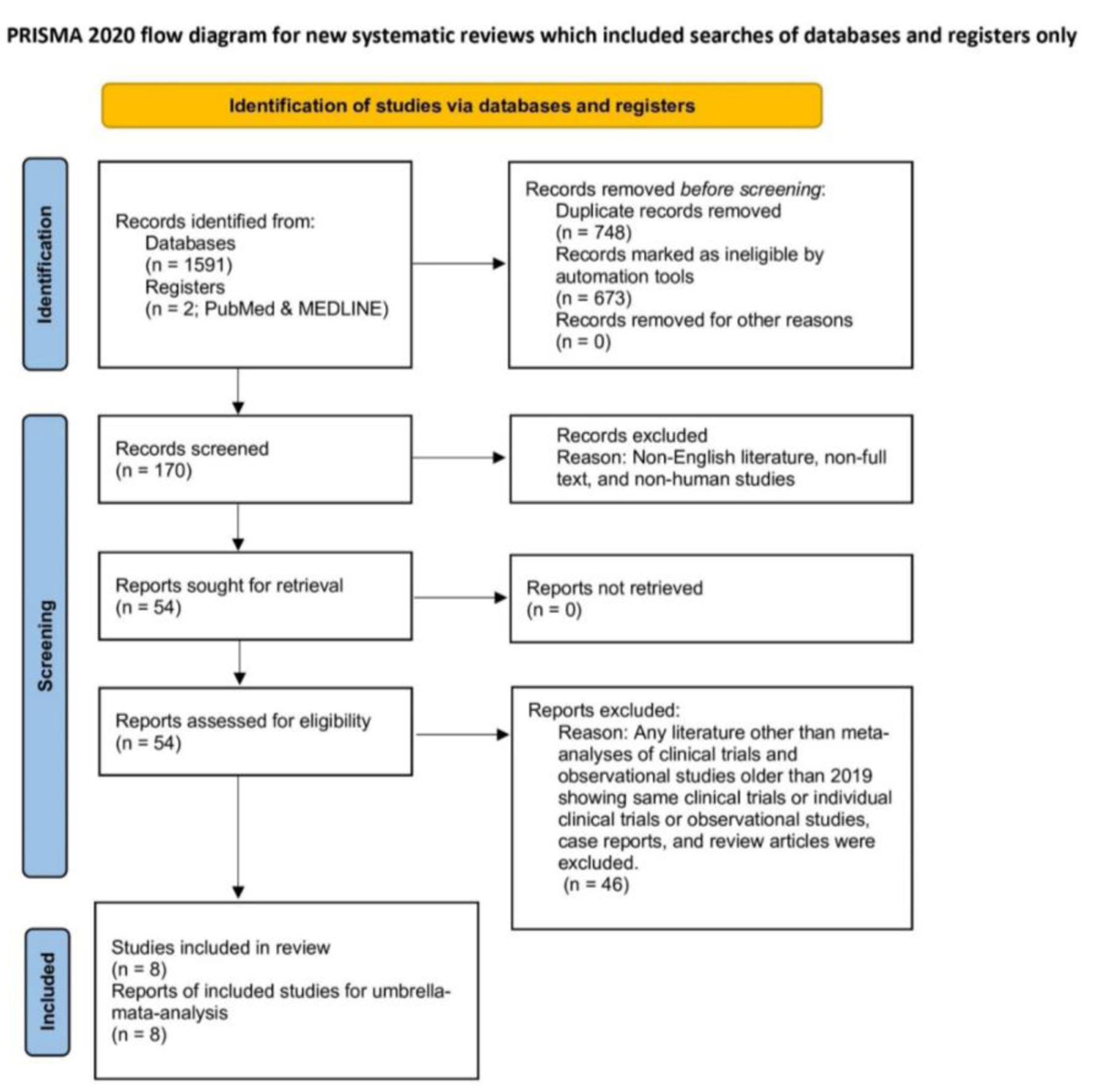
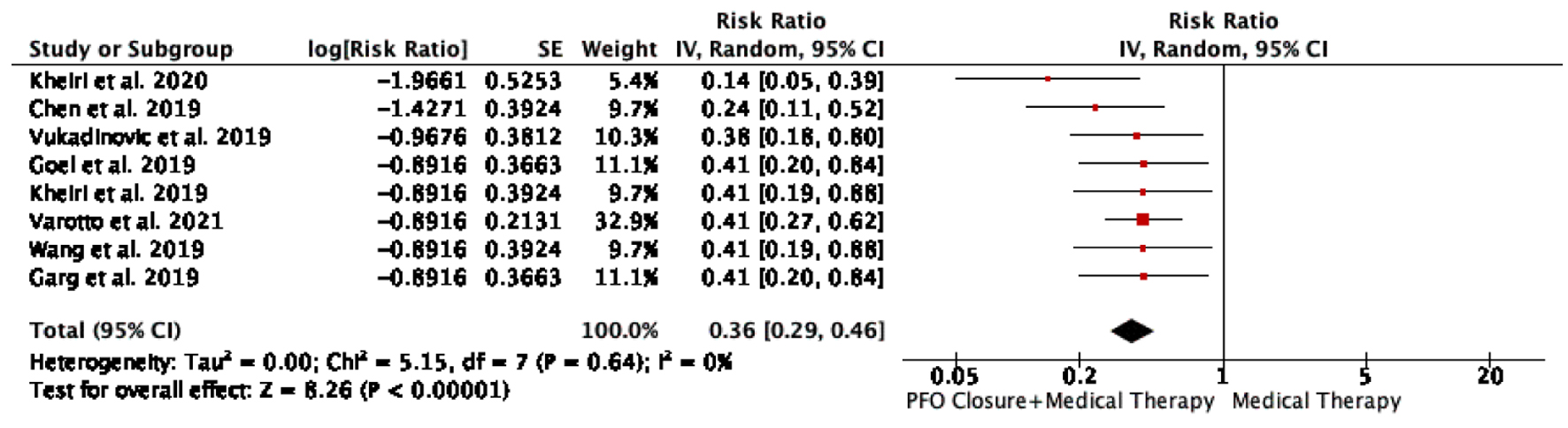
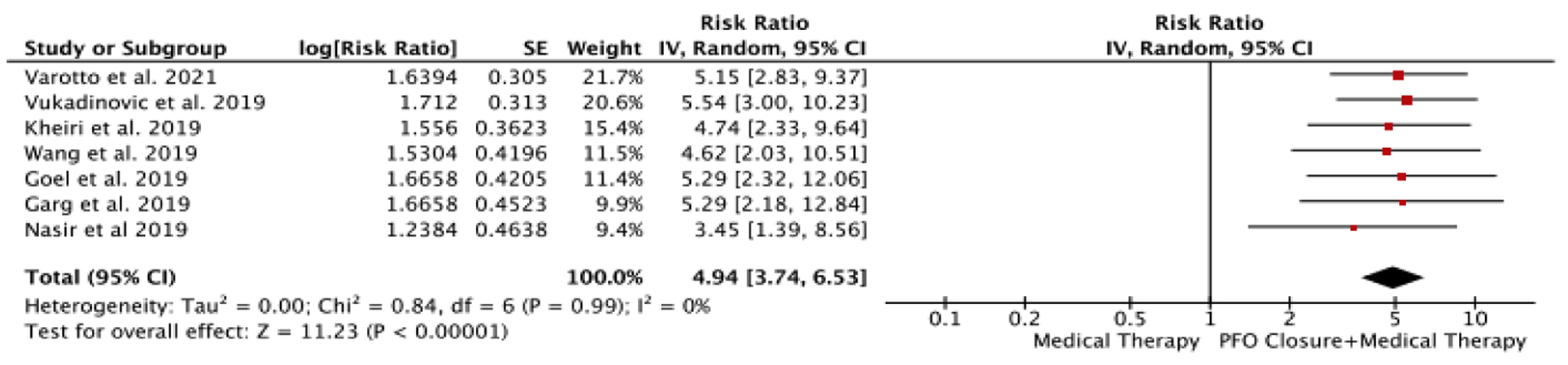
| Varotto et al, 2021 [24] | 2012 - 2018 | Meta-analysis of RCTs | Cryptogenic stroke or TIA | 45.4 - 46.2 | - | 6 | 3,560 | 1,889 vs. 1,671 | Recurrent stroke/TIA (37/1,889 vs. 77/1,671) (OR: 0.41 (0.27 - 0.6)); Atrial fibrillation (95/1,889 vs. 17/1,671) (OR: 5.15 (2.83 - 9.37); inverted from 0.20 (0.11 - 0.32)) |
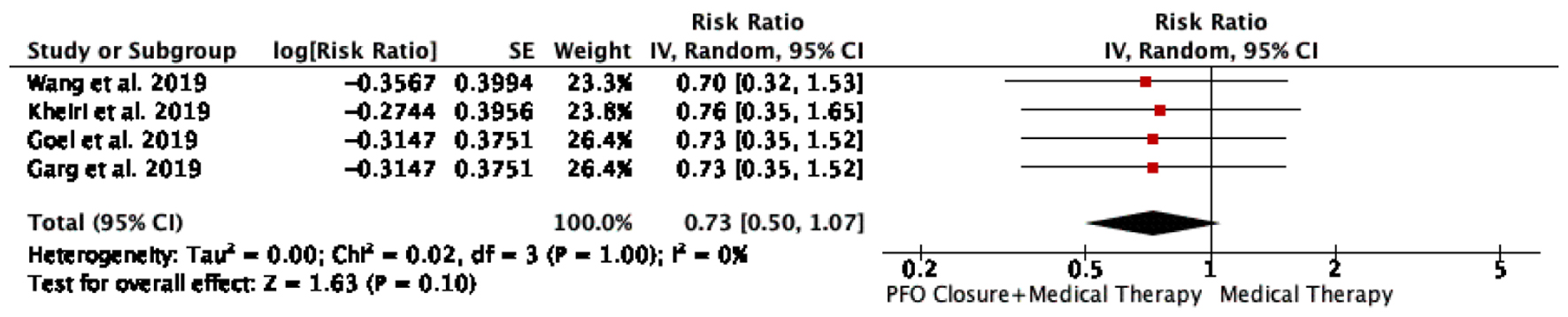
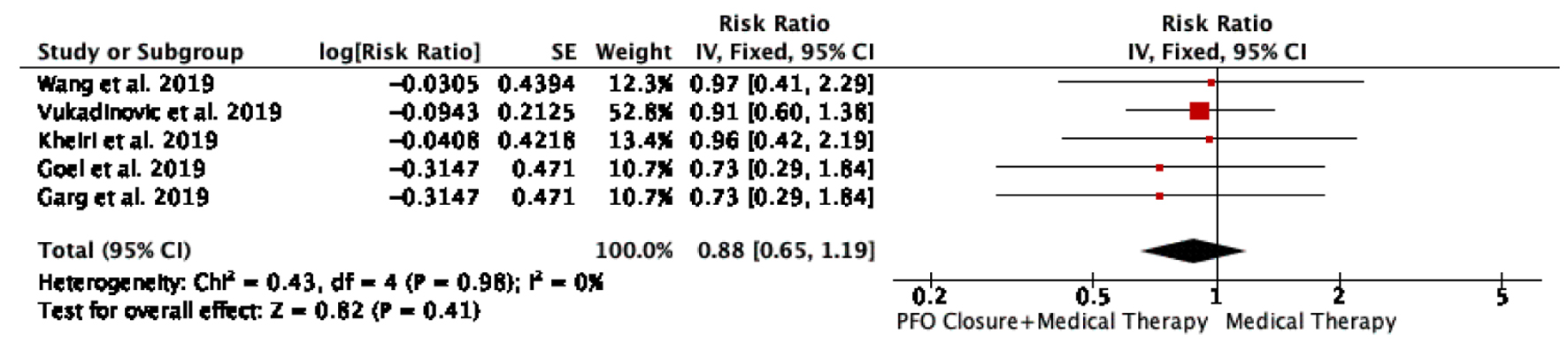
| Wang et al, 2019 [25] | 2012 - 2017 | Meta-analysis of RCTs | Cryptogenic stroke or TIA | 45 | 55 | 5 | 3,440 | 1,829 vs. 1,611 | Recurrent stroke (38/1,829 vs. 75/1,611) (OR: 0.41 (0.19 - 0.88)); Reduction in TIA (46/1,829 vs. 63/1,611) (OR: 0.71 (0.48 - 1.04)); All-cause mortality (13/1,829 vs. 16/1,611) (OR: 0.7 (0.32 - 1.52)); Atrial fibrillation (75/1,829 vs. 12/1,611) (OR: 4.62 (2.03 - 10.49)); Major bleeding (24/1,829 vs. 19/1,611) (OR: 0.97 (0.41 - 2.29)) |
| Vukadinovic et al, 2019 [26] | 2012 - 2018 | Meta-analysis of RCTs | Cryptogenic stroke or TIA | - | - | 6 | 3,560 | 1,889 vs. 1,671 | Reduction of stroke (37/1,889 vs. 77/1,671) (RR: 0.38 (0.18 - 0.82)); Reduction in stroke/ TIA (79/1,889 vs. 132/1,671) (RR: 0.56 (0.43 - 0.74)); Atrial fibrillation (78/1,844 vs. 12/1,667) (RR: 5.54 (3 - 10.2)); Major bleeding (43/1,820 vs. 42/1,583) (RR: 0.91 (0.6 - 1.3)) |
| Kheiri et al, 2019 [27] | 2012 - 2017 | Meta-analysis of RCTs | Cryptogenic stroke or TIA | 45.3 ± 9.7 | 54.97% | 5 | 3,440 | 1,829 vs. 1,611 | Reduction in stroke (37/1,829 vs. 72/1,611) (OR: 0.41 (0.19 - 0.90)); Reduction in TIA (44/1,829 vs. 56/1,611) (OR: 0.77 (0.51 - 1.14)); Atrial fibrillation (91/1,784 vs. 17/1,607) (OR: 4.74 (2.33 - 9.61)); All-cause mortality (13/1,784 vs. 15/1,607) (OR: 0.76 (0.35 - 1.65)); Major bleeding (24/1,760 vs. 19/1,523) (OR: 0.96 (0.42 - 2.22)) |
| Goel et al, 2019 [28] | 2012 - 2018 | Meta-analysis of RCTs | Cryptogenic stroke or TIA | 46 | 55% | 6 | 3,747 | 1,889 vs. 1,858 | Reduction in stroke (37/1,889 vs. 80/1,858) (RR: 0.41 (0.20 - 0.83)); Reduction in TIA (43/1,448 vs. 61/1,635) (RR: 0.79 (0.54 - 1.16)); Atrial fibrillation (76/1,784 vs. 12/1,794) (RR: 5.29 (2.32 - 12.06); All-cause mortality (13/1,889 vs. 16/1,858) (RR: 0.73 (CI: 0.35 - 1.55)); Major bleeding (24/1,820 vs. 32/1,770) (RR: 0.73 (0.29 - 1.84)) |
| Nasir et al, 2019 [29] | 2012 - 2018 | Meta-analysis of RCTs | Cryptogenic stroke or TIA | - | - | 6 | 3,510 | 1,839 vs. 1,671 | Reduction in stroke/TIA (28/1,839 vs. 66/1,671) (OR: 0.34 (0.15 - 0.79); Atrial fibrillation (86/1,829 vs. 22/1,614) (OR: 3.45 (1.39 - 8.58)) |
| Garg et al, 2019 [30] | 2012 - 2018 | Meta-analysis of RCTs | Cryptogenic stroke and TIA | 46 | 55% | 6 | 3,747 | 1,889 vs. 1,858 | Recurrent stroke (37/1,889 vs. 80/1,858) (RR: 0.41 (0.20 - 0.83); Reduction in TIA (43/1,448 vs. 61/1,635) RR: 0.79 (0.54 - 1.16); Atrial fibrillation (76/1,784 vs. 61/1,794) (RR: 5.29 (2.18 - 43.63)); All-cause mortality (13/1,889 vs. 16/1,858) (RR: 0.73 (0.35 - 1.55)); Major bleeding (24/1,820 vs. 32/1,770) (RR: 0.73 (0.29 - 1.84)) |
| Kheiri et al, 2020 [31] | 2002 - 2018 | Meta-analysis of RCTs and Observational studies | Cryptogenic stroke and embolic stroke of undetermined source | 61.2 ± 13.5 | 60.8% | 10 | 16,876 | 1,889 vs. 1,4987 | Recurrent stroke (HR: 0.14 (0.05 - 0.31)) |