| Cardiology Research, ISSN 1923-2829 print, 1923-2837 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, Cardiol Res and Elmer Press Inc |
| Journal website http://www.cardiologyres.org |
Case Report
Volume 10, Number 4, August 2019, pages 236-240
A Case of Isolated Left Ventricular Non-Compaction Cardiomyopathy in a HIV Patient Presenting With Acute Heart Failure
Bibi Ayeshaa, Rafeeq Ahmeda, b, Umut Gomcelia, Carlos Manriquea, Marin Nicua, Sridhar Chilimuria
aDepartment of Medicine, BronxCare Hospital Center, Bronx, NY 10457, USA
bCorresponding Author: Rafeeq Ahmed, Department of Medicine, BronxCare Hospital Center, 1650 Grand Concourse, 10th Floor, Bronx, NY 10457, USA
Manuscript submitted May 24, 2019, accepted June 24, 2019
Short title: Isolated LVNC Cardiomyopathy in a HIV Patient
doi: https://doi.org/10.14740/cr889
| Abstract | ▴Top |
The etiology of cardiomyopathy in a HIV patient is multifactorial. Identifying the etiology of cardiomyopathy in a HIV patient needs extensive evaluation. Common causes include ischemic cardiomyopathy, myocarditis due to viral infections and opportunistic infections, cocaine abuse, alcoholic heart disease, drug toxicity or due to nutritional deficiencies. However, in a number of cases the etiology is unknown. We report a case of 36-year-old African American man with history of HIV who presented with acute heart failure due to left ventricular non-compaction (LVNC). Transthoracic and transesophageal echocardiogram showed significant left ventricular trabeculations and blood flow in deep recesses. Endomyocardial biopsy was suggestive of LVNC. He underwent left ventricular assist device implantation for destination therapy and subsequently cardiac transplantation. The diagnosis of LVNC is often made by echocardiogram. As LVNC could be a normal variant, a comprehensive diagnostic assessment including multimodality imaging, a systematic screening of first degree relatives, and a comprehensive clinical and genetic assessment by a multidisciplinary team may be needed to arrive at the diagnosis. Early diagnosis and timely intervention may reduce the risk of premature death in these young patients.
Keywords: Cardiomyopathy; HIV; Left ventricular non-compaction
| Introduction | ▴Top |
The etiology of cardiomyopathy in a HIV patient is multifactorial. Various known causes include ischemic cardiomyopathy, myocarditis caused directly due to viral infections (HIV, Coxsackievirus, cytomegalovirus and Ebstein-Barr virus) or due to an opportunistic infection (toxoplasmosis and cryptococcosis), dysregulated immune function, cocaine abuse, alcoholic heart disease, drug toxicity (zidovudine and pentamidine), or due to nutritional factors like selenium and L-carnitine deficiency [1]. However, in a number of cases, the etiology is unknown. This article reports a case of a 36-year-old African American man with history of HIV and hepatitis B presenting with cardiomyopathy due to left ventricular non-compaction (LVNC). LVNC is a heterogeneous myocardial disorder characterized by structural and functional abnormal heart muscle and absence of other diseases sufficient to cause the observed myocardial abnormality [2]. LVNC can be regarded as an isolated entity or as one of the traits that may recur in cardiac and non-cardiac diseases [2]. Anatomically it is characterized by prominent trabeculae, intratrabecular recesses, and a left ventricular myocardium with two distinct compacted and non-compacted layers [3-5]. Continuity exists between the left ventricular cavity and deep intratrabecular recesses, both of which are filled with blood with no evidence of communication with the epicardial coronary artery system [4, 5].
| Case Report | ▴Top |
A 36-year-old African American man with a history of HIV (CD4 count of 1,024) and hepatitis B presented with 6 weeks of progressive shortness of breath. He complained of orthopnea, paroxysmal nocturnal dyspnea and decreased exercise tolerance but denied symptoms of chest pain, palpitations, dizziness or syncope. He had no past surgical history and was not taking any medications at home. He had 12 pack-year history of smoking. There was no family history of cardiomyopathy or sudden cardiac death. On physical examination, temperature was 98.2 °F, heart rate 120 beats per minute (bpm), blood pressure 116/71 mm Hg, respiratory rate 20 breaths/min and saturation 98% on room air. He had hepato-jugular reflux with jugular venous distension and S3 gallop on auscultation with bilateral lower lung rales. Laboratory tests showed elevated pro-brain natriuretic peptide. Chest radiograph was suggestive of pulmonary edema and an electrocardiogram revealed sinus tachycardia. Transthoracic echocardiogram showed ejection fraction of 17%, dilated left ventricle (LV), severe mitral regurgitation and left ventricular trabeculations (Figs. 1, 2). He developed acute hypoxic respiratory failure and hemodynamic instability requiring intubation, mechanical ventilation, inotropic therapy, and intra-aortic balloon pump for circulatory support. He was started on standard pharmacotherapy for acute decompensated heart failure along with anticoagulation for thromboembolism prophylaxis. Transesophageal echocardiogram showed significant left ventricular trabeculations and blood flow in deep recesses (Fig. 2). Endomyocardial biopsy showed endocardial fibroelastosis and intertrabecular recesses; the fibroelastosis was seen extending on the surface of myocardial trabeculations and recesses suggestive of LVNC (Fig. 3). He underwent left ventricular assist device implantation for destination therapy and implantable cardioverter defibrillator placement for primary prevention of sudden cardiac death. Patient subsequently underwent cardiac transplantation.
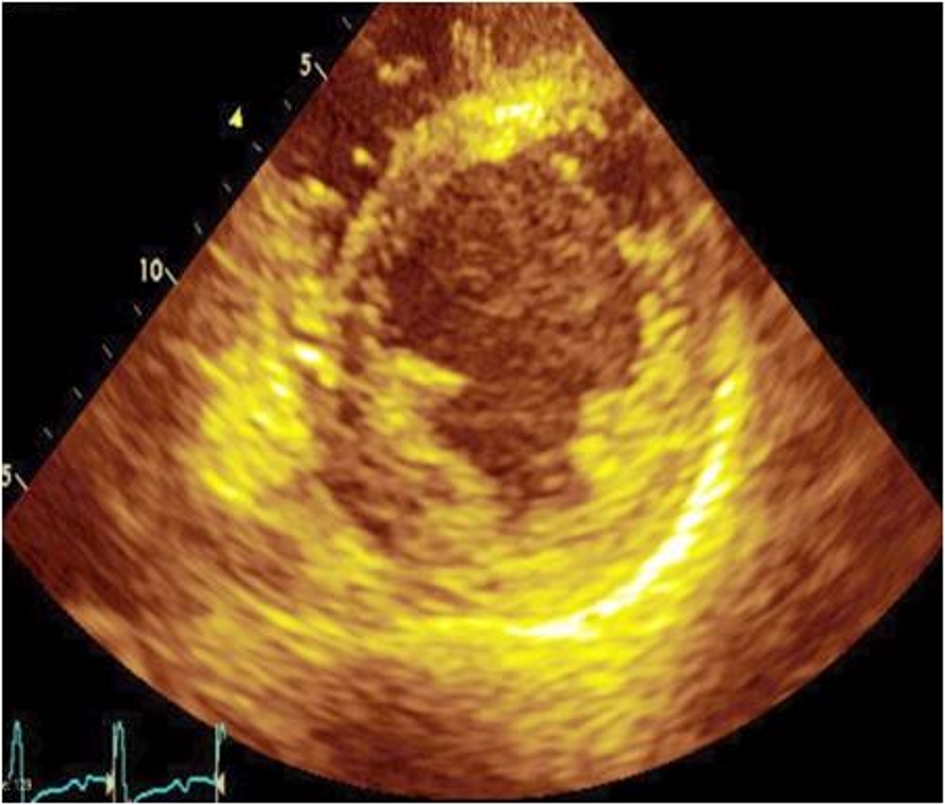 Click for large image | Figure 1. Transthoracic echocardiogram, parasternal short axis view of the left ventricle showing non-compaction of left ventricle. |
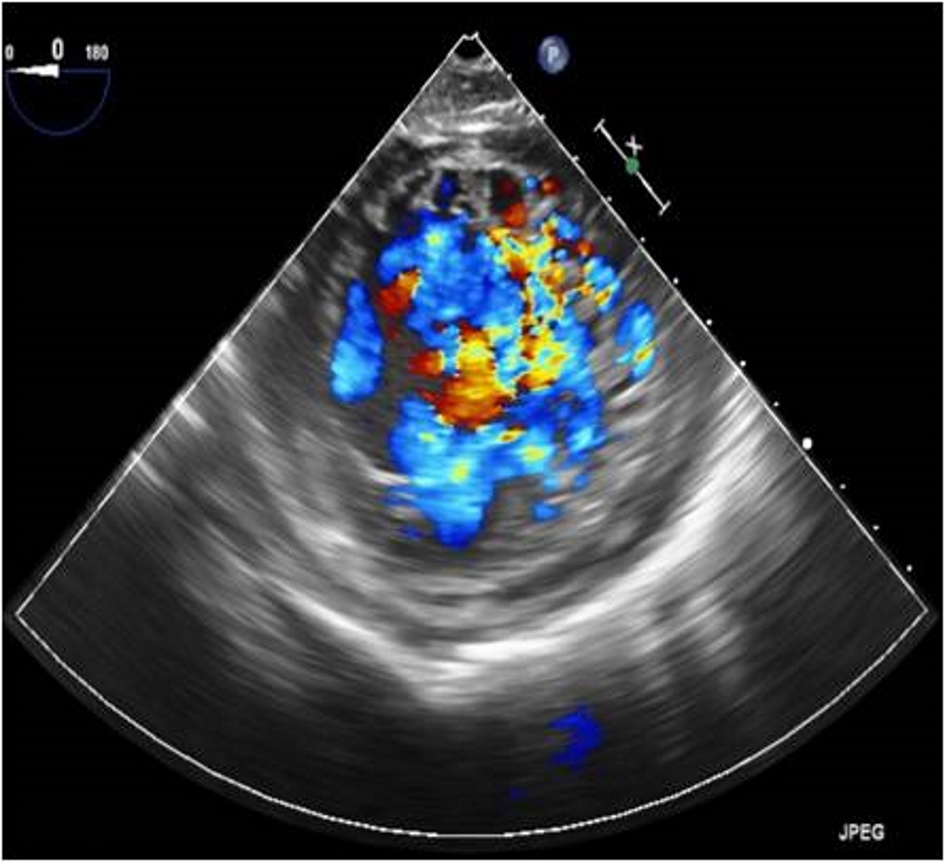 Click for large image | Figure 2. Transesophageal echocardiogram with color Doppler showing left ventricular non-compaction and blood flow in deep recesses. |
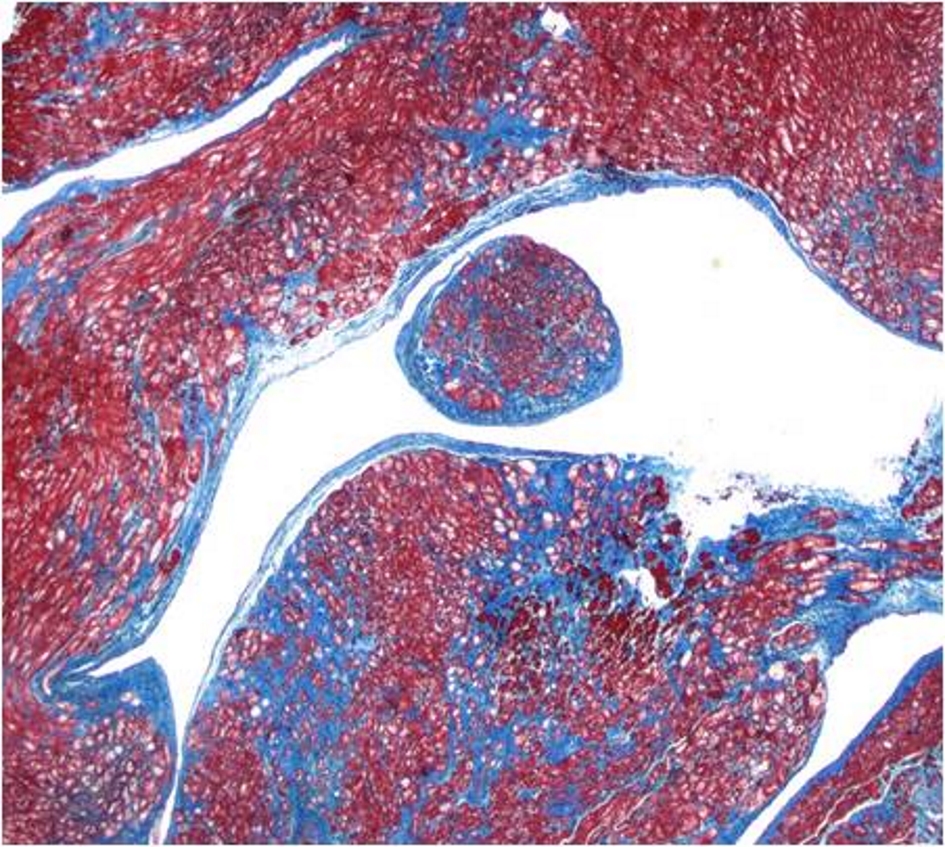 Click for large image | Figure 3. Endomyocardial biopsy showing endocardial fibroelastosis and intertrabecular recesses. Fibroelastosis extends on surface of myocardial trabeculations and recesses. |
| Discussion | ▴Top |
Historically, the prevalence of LVNC has been underestimated due to the lack of knowledge about this rare condition and its similarity to other diseases of the myocardium and endocardium. However, diagnosis of LVNC has increased over the last 25 years. A study of pediatric patients with primary cardiomyopathy showed that 9% of the patients had LVNC [6].
The median age at diagnosis of isolated non-compaction cardiomyopathy in the initial case series of isolated non-compaction was 7 years ranging from 11 months to 22 years [3].
The 1995 World Health Organization (WHO)/International Society and Federation of Cardiology Task Force on the definition and classification of cardiomyopathies did not classify non-compaction as a distinct cardiomyopathy but it was rather grouped as an unclassified cardiomyopathy [7].
LVNC can be regarded as an isolated entity or as one of the traits that may recur in cardiac and non-cardiac diseases [2]. LVNC is categorized into 7 groups [2]: 1) Isolated LVNC with normal systolic and diastolic function; 2) LVNC associated with left ventricular dilation and dysfunction at onset such as Barth syndrome; 3) LVNC in hearts fulfilling the diagnostic criteria for dilated cardiomyopathy, hypertrophic cardiomyopathy, restrictive cardiomyopathy, or arrythmogenic right ventricular cardiomyopathy; in these cases, cardiomyopathy and LVNC are both present; 4) LVNC associated with congenital heart disease (CHD), ranging from patent ductus arteriosus or atrial/ventricular septal defects to more severe diseases, such as the Ebstein anomaly or hypoplastic left heart syndrome; these disorders can be either sporadic or familial, with CHD in more than one family member; 5) Syndromes with LVNC, either sporadic or familial, in which the non-compaction morphology is one of the cardiac traits associated with both monogenic defects and chromosomal anomalies; examples include Anderson-Fabry disease and Danon disease; 6) Acquired and potentially reversible isolated LVNC, which has been reported in athletes; it has also been reported in sickle cell anemia, pregnancy, myopathies, and chronic renal failure; and 7) Right ventricular non-compaction, which can be concomitant with that of the LV, or presents as a unique anatomic area of non-compaction.
The spectrum of the initial presentation is wide, non-specific and depends on many factors. It depends on whether LVNC occurs in isolation or in association with a syndrome, CHD, or other diseases, whether LVNC is studied in a pediatric or adult population or whether LVNC is diagnosed in asymptomatic patients during family screening. Clinical symptoms at initial presentation are mainly the result of systolic/diastolic ventricular dysfunction and include non-specific chest pain/discomfort, heart failure symptoms, or arrhythmias [3, 4, 8-15].
The diagnosis of LVNC is often made by echocardiography. The ratio of non-compacted myocardium to compacted myocardium at the end of systole is > 2:1, which is the most often used echocardiographic criteria that were proposed by Jenni et al [15]. The criteria also include presence of segmental thickening of the myocardial wall of the LV with two layers comprising of prominent trabeculations and deep recesses with a thin epicardial layer and a thick endocardial layer. The absence of coexisting cardiac abnormalities is required to fulfill the criteria. LV diastolic dysfunction, reduced global LV systolic function, abnormal structure of papillary muscles, and LV thrombi are non-specific findings that can be seen on echocardiography [16]. Cardiac magnetic resonance (CMR) can be used in correlation with an echocardiogram to localize and quantify the extent of non-compaction. CMR offers a detailed view of the cardiac morphology of the non-compacted myocardial layer in the LV in any image plane including the apical and lateral segments, which are not well visualized by echocardiogram [17].
All patients with LVNC should receive family and genetic counseling. Heart Failure Society of America (HFSA) recommends obtaining careful family history for at least three generations and screening first-degree relatives of patients with cardiomyopathy including LVNC. Clinical screening should include history, physical examination, electrocardiogram, echocardiogram, and creatine kinase MM fraction. Asymptomatic first-degree relatives with negative initial screening should be rescreened at 3-year intervals beginning in childhood or any time that symptoms or signs appear [18].
There is no therapy specific for patients with LVNC. Despite limitations of the published risk factors for adverse outcomes, they are helpful to guide treatment, including medical therapy and device therapy. Although so far unproven by prospective studies, timely institution of evidence-based standard heart failure treatment in asymptomatic patients with worsening LV systolic function may prevent the occurrence of complications [11, 19, 20].
Therapy for LVNC is largely dictated by concomitant clinical findings associated with myocardial dysfunction or significant arrhythmias, or both, or CHD. Patients with evidence of systolic or diastolic dysfunction should be managed on the basis of existing heart failure management recommendations [21]. For patients with LVNC and associated systolic dysfunction or dilated cardiomyopathy phenotypes, oral treatments typically include anti-congestive medications that help to favorably remodel the LV, including angiotensin-converting enzyme inhibitors and β blockers, and an aldosterone antagonist. Loop diuretics should be considered for patients with evidence of congestion or volume overload, and aspirin is used to reduce the risk of thrombotic complications. Inpatient treatments include intravenous diuretics or vasodilatory drugs, or both, in the setting of acute decompensated heart failure. Inotropes can be used in patients with evidence of low cardiac output and poor end-organ perfusion. Implantable-cardioverter defibrillators are an option if patients meet criteria for implantation as recommended in published guidelines. Advanced pacing strategies, such as cardiac resynchronization, are also used, and result in improvement in some patients [17, 22]. Ventricular assist devices and cardiac transplantation are possibilities for patients with end-stage disease. Patients with associated hypertrophic cardiomyopathy might benefit from symptomatic treatment with β blockers or calcium channel blockers when LV outflow tract obstruction is present. Internal cardioverter defibrillator placement should be considered for patients with increased risk of sudden cardiac death [23]. The thromboembolic risks associated with LVNC are well known [9, 24]. They are mainly reported in adults [24], and thus antiplatelet or systemic anticoagulation should be considered in adults, especially when the LV or atria are dilated. The incidence of stroke or other embolic events in children remains poorly characterized, and antiplatelet drugs might be an option in those with depressed left ventricular systolic dysfunction, evidence of spontaneous echocardiographic contrast, severe left ventricular dilation, or dilated atria. The presence of atrial fibrillation might also prompt use of systemic anticoagulation. In patients with primary diastolic dysfunction, drug treatment might be instituted but none has proven benefit.
Outcomes of patients with LVNC are largely associated with the presence of myocardial dysfunction or clinically significant arrhythmias, or both. In 2013, Brescia et al [25] reported that of 242 children with LVNC at a single center, 150 (62%) had myocardial dysfunction and 80 (33%) had a clinically significant arrhythmia, both of which were strongly associated with mortality (P < 0.001 and P = 0.002, respectively). Similar reports cite myocardial dysfunction or ventricular arrhythmias as predictors of mortality in adults.
Echocardiographers and clinicians have to be cautioned not to over diagnose LVNC. Non-compaction of the left ventricular myocardium may reflect a morphological trait and there is a grey zone between a normal variant and a pathological myocardial structure with clinical relevance. A comprehensive diagnostic assessment including multimodality imaging, a systematic screening of first degree relatives, and a comprehensive clinical, and genetic assessment by a multidisciplinary team may provide the information to determine whether LVNC is just a morphological expression or phenotypic variant of other cardiomyopathies of a primary genetic disorder [26].
Conclusions
Identifying the etiology of cardiomyopathy in a HIV patient needs extensive evaluation. Rare condition like LVNC should not be missed in these patients. The diagnosis of LVNC is often missed due to a lack of awareness. Early diagnosis and timely intervention may reduce the risk of premature death in these young patients.
Acknowledgments
This case was presented at American Medical Association (AMA) research symposium in November 2015 as podium presentation by one of the author.
Financial Disclosure
None.
Conflict of Interest
None.
Informed Consent
Verbal consent was obtained.
Author Contributions
BA, RA, and UG prepared the manuscript; CM, MN and SC reviewed the manuscript.
| References | ▴Top |
- Lewis W. Cardiomyopathy in AIDS: a pathophysiological perspective. Prog Cardiovasc Dis. 2000;43(2):151-170.
doi pubmed - Arbustini E, Favalli V, Narula N, Serio A, Grasso M. Left ventricular noncompaction: a distinct genetic cardiomyopathy? J Am Coll Cardiol. 2016;68(9):949-966.
doi pubmed - Chin TK, Perloff JK, Williams RG, Jue K, Mohrmann R. Isolated noncompaction of left ventricular myocardium. A study of eight cases. Circulation. 1990;82(2):507-513.
doi pubmed - Pignatelli RH, McMahon CJ, Dreyer WJ, Denfield SW, Price J, Belmont JW, Craigen WJ, et al. Clinical characterization of left ventricular noncompaction in children: a relatively common form of cardiomyopathy. Circulation. 2003;108(21):2672-2678.
doi pubmed - Engberding R, Yelbuz TM, Breithardt G. Isolated noncompaction of the left ventricular myocardium - a review of the literature two decades after the initial case description. Clin Res Cardiol. 2007;96(7):481-488.
doi pubmed - Andrews RE, Fenton MJ, Ridout DA, Burch M, British Congenital Cardiac Association. New-onset heart failure due to heart muscle disease in childhood: a prospective study in the United kingdom and Ireland. Circulation. 2008;117(1):79-84.
doi pubmed - Richardson P, McKenna W, Bristow M, Maisch B, Mautner B, O'Connell J, Olsen E, et al. Report of the 1995 World Health Organization/International Society and Federation of Cardiology Task Force on the Definition and Classification of cardiomyopathies. Circulation. 1996;93(5):841-842.
doi pubmed - Oechslin EN, Attenhofer Jost CH, Rojas JR, Kaufmann PA, Jenni R. Long-term follow-up of 34 adults with isolated left ventricular noncompaction: a distinct cardiomyopathy with poor prognosis. J Am Coll Cardiol. 2000;36(2):493-500.
doi - Ichida F, Hamamichi Y, Miyawaki T, Ono Y, Kamiya T, Akagi T, Hamada H, et al. Clinical features of isolated noncompaction of the ventricular myocardium: long-term clinical course, hemodynamic properties, and genetic background. J Am Coll Cardiol. 1999;34(1):233-240.
doi - Aras D, Tufekcioglu O, Ergun K, Ozeke O, Yildiz A, Topaloglu S, Deveci B, et al. Clinical features of isolated ventricular noncompaction in adults long-term clinical course, echocardiographic properties, and predictors of left ventricular failure. J Card Fail. 2006;12(9):726-733.
doi pubmed - Stanton C, Bruce C, Connolly H, Brady P, Syed I, Hodge D, Asirvatham S, et al. Isolated left ventricular noncompaction syndrome. Am J Cardiol. 2009;104(8):1135-1138.
doi pubmed - Lilje C, Razek V, Joyce JJ, Rau T, Finckh BF, Weiss F, Habermann CR, et al. Complications of non-compaction of the left ventricular myocardium in a paediatric population: a prospective study. Eur Heart J. 2006;27(15):1855-1860.
doi pubmed - Wald R, Veldtman G, Golding F, Kirsh J, McCrindle B, Benson L. Determinants of outcome in isolated ventricular noncompaction in childhood. Am J Cardiol. 2004;94(12):1581-1584.
doi pubmed - Murphy RT, Thaman R, Blanes JG, Ward D, Sevdalis E, Papra E, Kiotsekoglou A, et al. Natural history and familial characteristics of isolated left ventricular non-compaction. Eur Heart J. 2005;26(2):187-192.
doi pubmed - Jenni R, Oechslin E, Schneider J, Attenhofer Jost C, Kaufmann PA. Echocardiographic and pathoanatomical characteristics of isolated left ventricular non-compaction: a step towards classification as a distinct cardiomyopathy. Heart. 2001;86(6):666-671.
doi pubmed - Lofiego C, Biagini E, Pasquale F, Ferlito M, Rocchi G, Perugini E, Bacchi-Reggiani L, et al. Wide spectrum of presentation and variable outcomes of isolated left ventricular non-compaction. Heart. 2007;93(1):65-71.
doi pubmed - Petersen SE, Selvanayagam JB, Wiesmann F, Robson MD, Francis JM, Anderson RH, Watkins H, et al. Left ventricular non-compaction: insights from cardiovascular magnetic resonance imaging. J Am Coll Cardiol. 2005;46(1):101-105.
doi pubmed - Hershberger RE, Lindenfeld J, Mestroni L, Seidman CE, Taylor MR, Towbin JA, Heart Failure Society of A. Genetic evaluation of cardiomyopathy - a Heart Failure Society of America practice guideline. J Card Fail. 2009;15(2):83-97.
doi pubmed - Dickstein K, Cohen-Solal A, Filippatos G, McMurray JJ, Ponikowski P, Poole-Wilson PA, Stromberg A, et al. ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2008: the Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2008 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association of the ESC (HFA) and endorsed by the European Society of Intensive Care Medicine (ESICM). Eur Heart J. 2008;29(19):2388-2442.
- Hunt SA, Abraham WT, Chin MH, Feldman AM, Francis GS, Ganiats TG, Jessup M, et al. 2009 Focused update incorporated into the ACC/AHA 2005 Guidelines for the Diagnosis and Management of Heart Failure in Adults A Report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines Developed in Collaboration With the International Society for Heart and Lung Transplantation. J Am Coll Cardiol. 2009;53(15):e1-e90.
- Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE, Jr., Drazner MH, Fonarow GC, et al. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2013;62(16):e147-239.
- Alhabshan F, Smallhorn JF, Golding F, Musewe N, Freedom RM, Yoo SJ. Extent of myocardial non-compaction: comparison between MRI and echocardiographic evaluation. Pediatr Radiol. 2005;35(11):1147-1151.
doi pubmed - Gersh BJ, Maron BJ, Bonow RO, Dearani JA, Fifer MA, Link MS, Naidu SS, et al. 2011 ACCF/AHA guideline for the diagnosis and treatment of hypertrophic cardiomyopathy: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Developed in collaboration with the American Association for Thoracic Surgery, American Society of Echocardiography, American Society of Nuclear Cardiology, Heart Failure Society of America, Heart Rhythm Society, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. J Am Coll Cardiol. 2011;58(25):e212-260.
- Pitta S, Thatai D, Afonso L. Thromboembolic complications of left ventricular noncompaction: case report and brief review of the literature. J Clin Ultrasound. 2007;35(8):465-468.
doi pubmed - Brescia ST, Rossano JW, Pignatelli R, Jefferies JL, Price JF, Decker JA, Denfield SW, et al. Mortality and sudden death in pediatric left ventricular noncompaction in a tertiary referral center. Circulation. 2013;127(22):2202-2208.
doi pubmed - Oechslin E, Jenni R. Left ventricular non-compaction revisited: a distinct phenotype with genetic heterogeneity? Eur Heart J. 2011;32(12):1446-1456.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cardiology Research is published by Elmer Press Inc.


