| Cardiology Research, ISSN 1923-2829 print, 1923-2837 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, Cardiol Res and Elmer Press Inc |
| Journal website https://www.cardiologyres.org |
Original Article
Volume 15, Number 2, April 2024, pages 125-128
Prevalence of Aortic Root Pathologies in Platypnea-Orthodeoxia Syndrome Secondary to Intra-Cardiac Shunts
Omer Farooqa, f, Usman Ghanib, Harvey Friedmanc, Muhammad Sikander Akbard, Hammad Saudyed, Sundus Alame, Muhammad Junaid Khane, Sumeet Muttia
aInternal Medicine, Ascension St Francis Hospital, Evanston, IL 60202, USA
bNorthwest General Hospital and Research Center, Peshawar, Pakistan
cPulmonary and Critical Care Medicine, Ascension St Francis Hospital, Evanston, IL 60202, USA
dInterventional Cardiology, Ascension St Francis Hospital, Evanston, IL 60202, USA
eGloucestershire Royal Hospital, Gloucester GL1 3NN, UK
fCorresponding Author: Omer Farooq, Internal Medicine, Ascension St Francis Hospital, Evanston, IL 60202, USA
Manuscript submitted February 6, 2024, accepted March 18, 2024, published online April 15, 2024
Short title: Aortic Pathologies and Platypnea-Orthodeoxia
doi: https://doi.org/10.14740/cr1624
| Abstract | ▴Top |
Background: Atrial septal defects can allow right to left shunting of venous blood which presents clinically as platypnea-orthodeoxia syndrome. It is believed that concomitant presence of aortic root pathologies increases the likelihood of shunting.
Methods: The study included a review of 510 articles listed in PubMed of patients with platypnea-orthodeoxia syndrome. Case reports of patients with extra-cardiac etiologies of platypnea-orthodeoxia were excluded.
Results: We reviewed 191 case reports, and 98 cases (51.3%) had evidence of concomitant aortic root pathology. Furthermore, of the remaining 93 case reports, 69 ones excluded any mention of the nature of the aortic root altogether, further suggesting that this is an underreported number.
Conclusions: There is a high prevalence of aortic root pathologies in patients with platypnea-orthodeoxia syndrome secondary to intra-cardiac shunts. In patients with unexplained hypoxemia and incidental finding of aortic root pathology, it may be worthwhile to obtain postural oxygen saturation measurements to exclude intra-cardiac shunts as the potential cause.
Keywords: Platypnea-orthodeoxia syndrome; Atrial septal defect; Patent foramen ovale; Aortic aneurysm; Aortic elongation; Aortic root pathology; Platypnea; Orthodeoxia
| Introduction | ▴Top |
Platypnea-orthodeoxia syndrome (POS) is a phenomenon in which patients develop dyspnea and hypoxemia in the upright position; these symptoms resolve upon lying down [1, 2]. The most common etiology is an atrial septal defect (ASD), particularly patent foramen ovale (PFO), which allows right to left shunting of deoxygenated blood [3, 4]. The question arises: why does shunting only occur in the upright position? The answer to this may lie in spatial positioning of aortic root in relation to the atrial septum. It is hypothesized that in the upright position the aortic root sits on top of the atrial septum. This might introduce redundancy into the septum, which could magnify the opening of the ASD, thus allowing right to left shunting. In the lying position the relief of excessive weight could cause the septum to become taut thus effectively closing the shunt [5, 6]. It would then logically follow that in cases where the aortic root is heavier, as in certain aortic root pathologies, the likelihood of shunting should increase. Although some case reports have previously hypothesized this particular association, there have been no formal studies estimating the prevalence of aortic root pathologies in this subset of patients [7]. The aim of our review was to study this association in more depth.
| Materials and Methods | ▴Top |
Two investigators (O.F. and U.G.) independently performed a systematic search of the PubMed database from inception to 2022, using a search strategy that involved use of medical subject heading (MeSH) and various combinations of terms, including but not limited to “platypnea”, “orthodeoxia”, “atrial septal defect”, “patent foramen ovale”, “right to left cardiac shunt”, combined with the use of appropriate Boolean operators.
The inclusion criteria for our study were as follows: 1) Case reports with clinical evidence of POS; 2) Known ASD as the underlying etiology; 3) Articles in English or with an English translation.
A total of 510 studies were reviewed. After excluding descriptive studies and case reports with extra-cardiac etiologies of POS, a total of 164 studies (case reports and case series) were obtained that met the inclusion criteria. These 164 studies yielded 191 case reports for full text review.
An Excel spreadsheet was created where findings of each case report were stored, including nature of the ASD, age and sex of patient, presence or absence of aortic root pathology and, if present, nature of the aortic root pathology.
The Institutional Review Board (IRB) approval and ethical compliance are not applicable.
| Results | ▴Top |
Of the 191 case reports reviewed, 98 (51.3%) had concomitant aortic root pathologies. The overwhelming majority of these were aortic root aneurysms, noted in 82 (83.7%) patients. The remaining pathologies included aortic root elongation in nine (9.2%) patients and a tortuous aorta in seven (7.1%) patients. Most of these aortic root pathologies were incidentally picked up on computed tomography (CT) angiography performed as workup of hypoxemia in these patients. The remaining few aortic pathologies were observed on echocardiography.
The mean age of patients with concomitant aortic root pathologies was 74 years. Fifty-two percent of these patients were male. None of the patients had any significant additional cardiac defects.
The literature review process and findings of our study are illustrated in Figure 1.
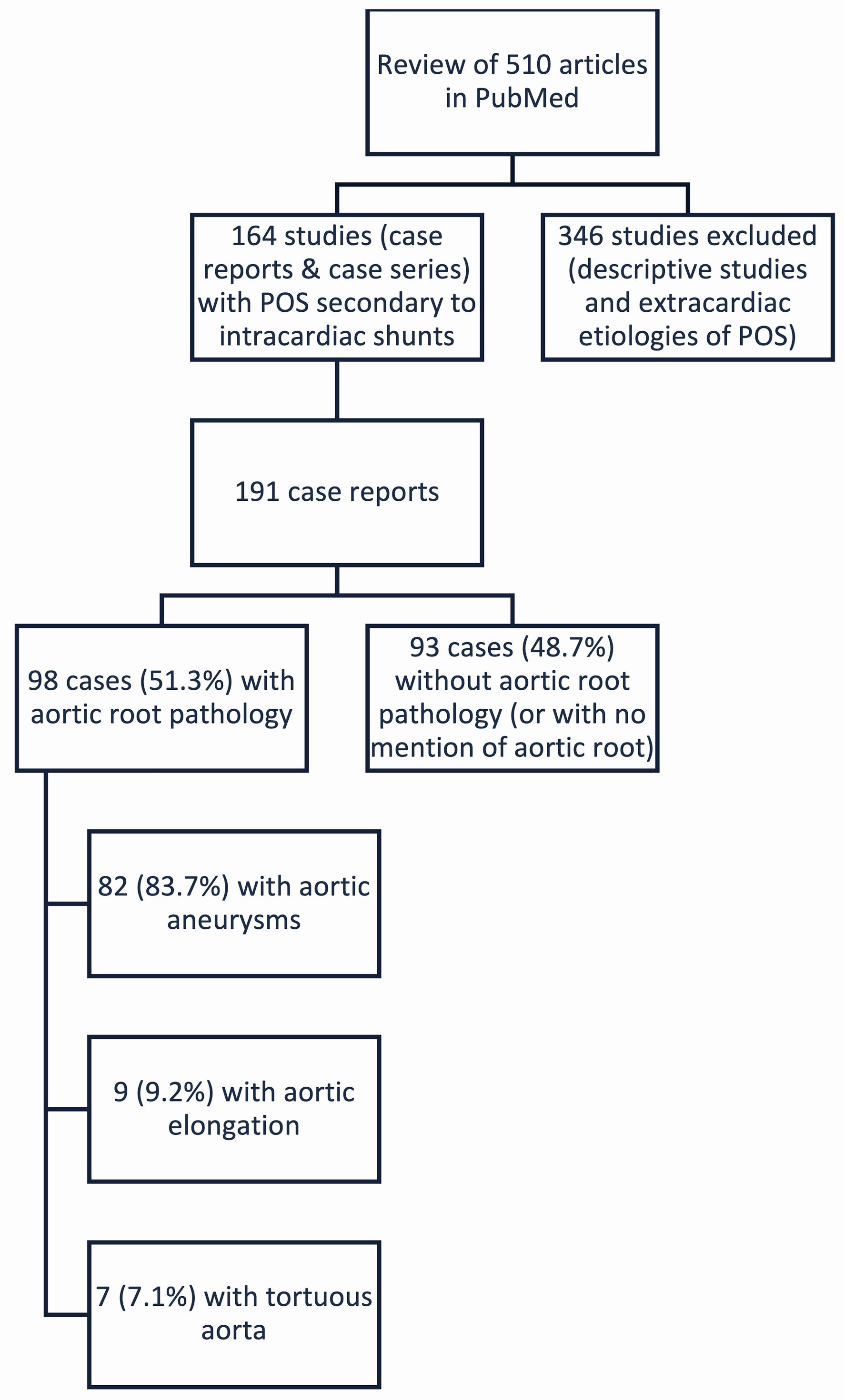 Click for large image | Figure 1. Illustration of the literature review process. POS: platypnea-orthodeoxia syndrome. |
It is important to note that in our review of the remaining 93 case reports without aortic root pathologies, 69 case reports excluded any mention of the nature of the aortic root altogether. It is possible that some of these cases could have underreported aortic pathologies, thereby highlighting the need for consistent reporting of aortic root sizes in future case reports.
| Discussion | ▴Top |
Platypnea-orthodeoxia is a syndrome characterized by dyspnea and hypoxemia in the upright position that resolves upon recumbency, an inverse of the presentation seen with congestive heart failure. The most common etiology is ASD, such as PFO. Other less common causes can include intra-pulmonary shunts and ventilation-perfusion (V/Q) mismatch [8-10].
In patients with ASD, pathophysiology most likely involves spatial positioning of the aortic root relative to the atrial septum [8]. In the upright position, the aortic root lies superior to the septum, weighing down on it. The flaccidity introduced into the septum from the additional weight magnifies the opening of the underlying ASD. This increases the probability of right to left shunting. Upon lying down, the excess weight is relieved thus narrowing the opening. Excess weight from aortic root pathologies, such as aortic root aneurysms, can therefore potentiate the probability of shunting. This pathomechanism has been previously hypothesized and studied in small scale retrospective studies [6].
From our review of case reports, it is evident that nearly half of these patients have concomitant aortic root pathologies. The most common aortic root pathology seen is an aneurysm as previously mentioned. In addition, aortic root elongation seen with increasing age can be another potential trigger [11, 12]. Patients with ASDs may remain asymptomatic early throughout life, with symptoms developing as the aortic root elongates with age [13].
One notable aspect of this study is the aforementioned underreporting of aortic root size in many of the studies reviewed. The association between aortic root size and platypnea-orthodeoxia has not been widely studied, which leads many authors to omit mention of aortic root size in their case reports. It is highly likely that in many of the studies not reporting the aortic root size, a considerable number had underlying aortic root pathologies. The actual prevalence may therefore be even higher. Our hope is that our study further highlights this association thus enabling consistent reporting of aortic root sizes in these patients, allowing future studies to explore this association in more depth.
This association does carry significant diagnostic implications. Most of these patients initially present with unexplained hypoxemia, and nearly all of them undergo CT pulmonary angiography to rule out pulmonary embolism. In such cases, if CT angiography is negative for pulmonary embolus but incidentally shows an aneurysmal aortic root, it should alert the reader to the possibility of an occult intracardiac shunt as the potential cause of hypoxemia. This can be followed up with simple bedside testing of postural oxygen saturation measurement. If postural oxygen discrepancy is observed, it can prevent unnecessary further diagnostic imaging and workup of hypoxemia [14, 15]. Diagnosis of the shunt can thereafter be confirmed with tilt-table transthoracic echocardiography with saline injection [11, 16-18].
The treatment for patients with platypnea-orthodeoxia due to intracardiac shunts involves closing the shunt itself [19-25]. Many of the patients reviewed in our study underwent subsequent cardiac repair with shunt closure. Those who did undergo shunt closure experienced complete resolution of POS. As such, therapeutic implications of this association may therefore appear limited on the surface, given that the treatment involves closure of the shunt and is not directed at the aortic root pathology itself. However, as we explore this association further, it may allow further insights into the relationship, potentially raising questions such as prophylactic closure of septal defects in patients with aortic root pathologies or at a certain age when the aortic root elongation may prove to be an inciting factor.
Conclusions
Aortic root pathologies are present in nearly half of the patients with POS secondary to intra-cardiac shunts, and possibly potentiate shunting. When encountered with a patient with unexplained hypoxemia where CT pulmonary angiography is negative for pulmonary embolism but incidentally reveals aortic root pathology, it may be worthwhile to obtain postural oxygen saturation measurements to exclude intra-cardiac shunts as the potential cause.
Acknowledgments
None to declare.
Financial Disclosure
No funding was obtained.
Conflict of Interest
The authors declare no conflict of interest.
Informed Consent
Not applicable.
Author Contributions
Conceptualization/study design, project administration, review and editing: Omer Farooq, Usman Ghani, Harvey Friedman, Muhammad Sikander Akbar, and Hammad Saudye. Data curation: Omer Farooq, Usman Ghani, Sundus Alam, Muhammad Junaid Khan, and Sumeet Mutti. Formal analysis: Omer Farooq, Usman Ghani, Harvey Friedman, Muhammad Sikander Akbar, Hammad Saudye, Sundus Alam, Muhammad Junaid Khan, and Sumeet Mutti. Writing: Omer Farooq, Usman Ghani, Sundus Alam, Muhammad Junaid Khan, and Sumeet Mutti.
Data Availability
Data are openly available in a public database (PubMed).
| References | ▴Top |
- Tobis JM, Abudayyeh I. Platypnea-Orthodeoxia syndrome: an overlooked cause of hypoxemia. JACC Cardiovasc Interv. 2016;9(18):1939-1940.
doi pubmed - Rodrigues P, Palma P, Sousa-Pereira L. Platypnea-Orthodeoxia syndrome in review: defining a new disease? Cardiology. 2012;123(1):15-23.
doi pubmed - Chen GP, Goldberg SL, Gill EA, Jr. Patent foramen ovale and the platypnea-orthodeoxia syndrome. Cardiol Clin. 2005;23(1):85-89.
doi pubmed - Agrawal A, Palkar A, Talwar A. The multiple dimensions of Platypnea-Orthodeoxia syndrome: A review. Respir Med. 2017;129:31-38.
doi pubmed - Eicher JC, Bonniaud P, Baudouin N, Petit A, Bertaux G, Donal E, Piechaud JF, et al. Hypoxaemia associated with an enlarged aortic root: a new syndrome? Heart. 2005;91(8):1030-1035.
doi pubmed pmc - Bertaux G, Eicher JC, Petit A, Dobsak P, Wolf JE. Anotomic interaction between the aortic root and the atrial septum: a prospective echocardiographic study. J Am Soc Echocardiogr. 2007;20(4):409-414.
doi pubmed - Chai J, Velasquez A. The spinnaker effect: Platypnea-orthodeoxia syndrome due to PFO and aortic aneurysm. Chest. 2018 Oct;154(4):57A.
doi - Knapper JT, Schultz J, Das G, Sperling LS. Cardiac Platypnea-Orthodeoxia syndrome: an often unrecognized malady. Clin Cardiol. 2014;37(10):645-649.
doi pubmed pmc - Robin ED, Laman D, Horn BR, Theodore J. Platypnea related to orthodeoxia caused by true vascular lung shunts. N Engl J Med. 1976;294(17):941-943.
doi pubmed - Asami-Noyama M, Harada M, Hisamoto Y, Kobayashi T, Oishi K, Edakuni N, Hirano T, et al. Platypnea-Orthodeoxia syndrome in a patient with ongoing COVID-19. Respirol Case Rep. 2022;10(8):e01009.
doi pubmed pmc - Popp G, Melek H, Garnett AR, Jr. Platypnea-Orthodeoxia related to aortic elongation. Chest. 1997;112(6):1682-1684.
doi pubmed - Medina A, de Lezo JS, Caballero E, Ortega JR. Platypnea-Orthodeoxia due to aortic elongation. Circulation. 2001;104(6):741.
doi pubmed - Sanikommu V, Lasorda D, Poornima I. Anatomical factors triggering Platypnea-Orthodeoxia in adults. Clin Cardiol. 2009;32(11):E55-57.
doi pubmed pmc - Strunk BL, Cheitlin MD, Stulbarg MS, Schiller NB. Right-to-left interatrial shunting through a patent foramen ovale despite normal intracardiac pressures. Am J Cardiol. 1987;60(4):413-415.
doi pubmed - Seward JB, Hayes DL, Smith HC, Williams DE, Rosenow EC, 3rd, Reeder GS, Piehler JM, et al. Platypnea-Orthodeoxia: clinical profile, diagnostic workup, management, and report of seven cases. Mayo Clin Proc. 1984;59(4):221-231.
doi pubmed - Roxas-Timonera M, Larracas C, Gersony D, Di Tullio M, Keller A, Homma S. Patent foramen ovale presenting as Platypnea-Orthodeoxia: diagnosis by transesophageal echocardiography. J Am Soc Echocardiogr. 2001;14(10):1039-1041.
doi pubmed - Song JK. Pearls and pitfalls in the transesophageal echocardiographic diagnosis of patent foramen ovale. J Am Soc Echocardiogr. 2023;36(9):895-905.e893.
doi pubmed - Lombardi M, Del Buono MG, Princi G, Locorotondo G, Lombardo A, Vergallo R, Montone RA, et al. Platypnoea-orthodeoxia syndrome as an uncommon cause of dyspnoea: a literature review. Intern Med J. 2022;52(6):921-925.
doi pubmed pmc - Godart F, Rey C, Prat A, Vincentelli A, Chmait A, Francart C, Porte H. Atrial right-to-left shunting causing severe hypoxaemia despite normal right-sided pressures. Report of 11 consecutive cases corrected by percutaneous closure. Eur Heart J. 2000;21(6):483-489.
doi pubmed - Zier LS, Sievert H, Mahadevan VS. To close or not to close: contemporary indications for patent foramen ovale closure. Expert Rev Cardiovasc Ther. 2016;14(11):1235-1244.
doi pubmed - Rohrhoff N, Vavalle JP, Halim S, Kiefer TL, Harrison JK. Current status of percutaneous PFO closure. Curr Cardiol Rep. 2014;16(5):477.
doi pubmed - Zavalloni D, Lisignoli V, Barbaro C, Mennuni M, Tosi P, Marcheselli S, Presbitero P. Platypnoea-orthodeoxia syndrome secondary to patent foramen ovale (PFO): a challenging subset for PFO percutaneous closure. Heart Lung Circ. 2013;22(8):642-646.
doi pubmed - Gama ECA, Luz A, Oliveira F, Brochado B, Santos R, Alexandre A, Campinas A, et al. Platypnoea orthodeoxia syndrome and patent foramen ovale closure: single-centre experience and long-term follow-up. Heart Lung Circ. 2022;31(11):1547-1552.
doi pubmed - Giblett JP, Williams LK, Kyranis S, Shapiro LM, Calvert PA. Patent foramen ovale closure: state of the art. Interv Cardiol. 2020;15:e15.
doi pubmed pmc - Tobis JM, Narasimha D, Abudayyeh I. Patent foramen ovale closure for hypoxemia. Interv Cardiol Clin. 2017;6(4):547-554.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cardiology Research is published by Elmer Press Inc.


