| Cardiology Research, ISSN 1923-2829 print, 1923-2837 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, Cardiol Res and Elmer Press Inc |
| Journal website https://www.cardiologyres.org |
Original Article
Volume 14, Number 1, February 2023, pages 54-62
The Complexity of Peripheral Arterial Disease and Coronary Artery Disease in Diabetic Patients: An Observational Study
Khaled Alya, b , Sameh Sabeta, Alaa Elkieya, Hany Fakhrya
aCardiology Department, Faculty of Medicine, Ain Shams University, Cairo, Egypt
bCorresponding Author: Khaled Aly, Cardiology Department, Faculty of Medicine, Ain Shams University, Cairo, Egypt
Manuscript submitted January 3, 2023, accepted February 2, 2023, published online February 25, 2023
Short title: Complexity of PAD and CAD in Diabetics
doi: https://doi.org/10.14740/cr1463
| Abstract | ▴Top |
Background: Atherosclerosis is a systemic disease that causes luminal narrowing. Patients with peripheral arterial disease (PAD) also exhibit an increased risk of death from cardiovascular complications. This risk is the same for symptomatic or asymptomatic patients. Over a 5-year period, patients with PAD have a 20% chance of suffering from a stroke or myocardial infarction. Additionally, their mortality rate is 30%. This study aimed to assess the relationship between coronary artery disease (CAD) complexity using SYNTAX score and PAD complexity using Trans-Atlantic Inter-Society Consensus II (TASC II) score.
Methods: The study was designed as single-center cross-sectional observational and included 50 diabetic patients referred for elective coronary angiography and peripheral angiography was done.
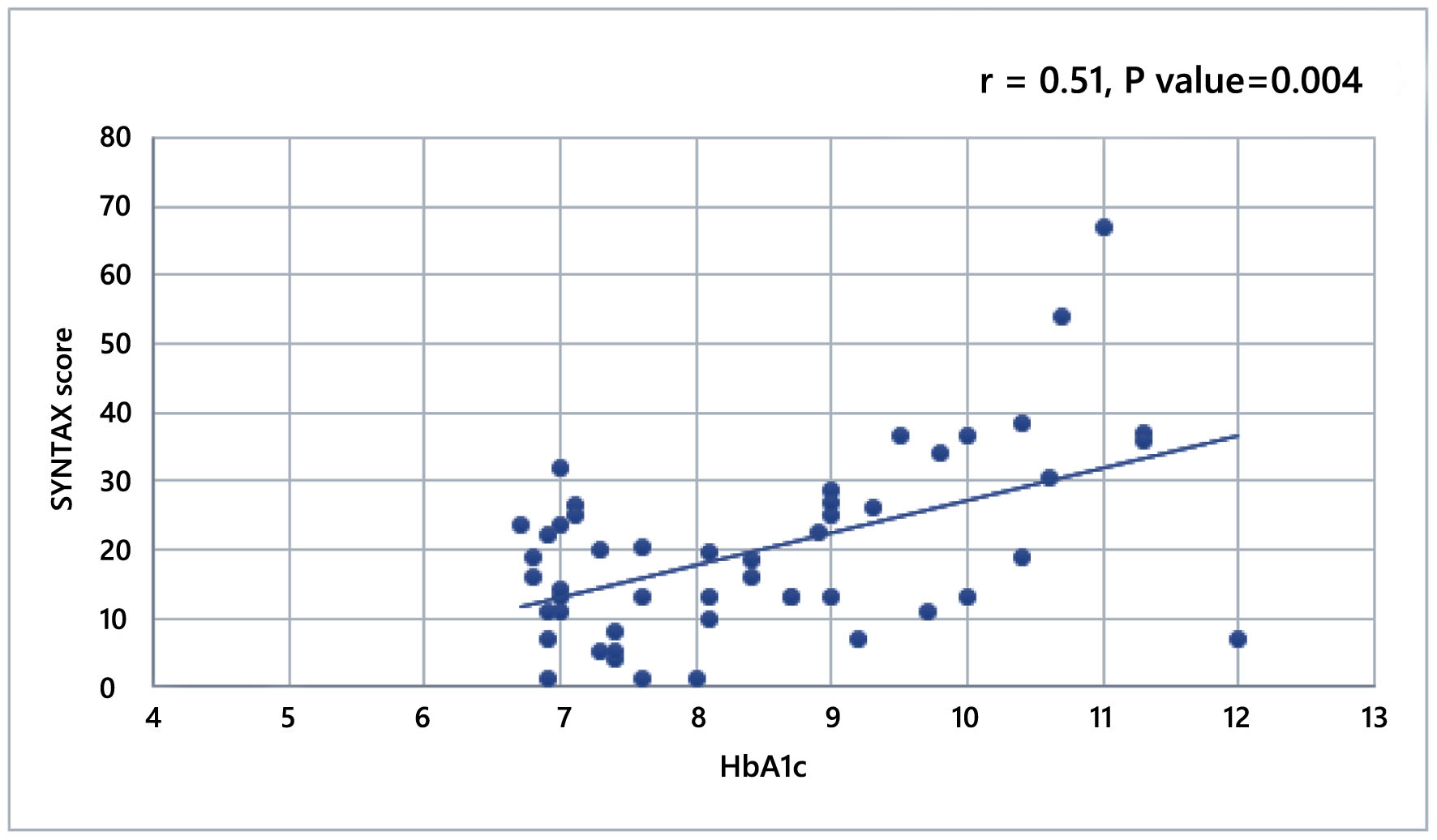
Results: Most of the patients were males (80%) and smokers (80%) with mean age of 62 years. The mean SYNTAX score was 19.88. There was a significant negative correlation between SYNTAX score and ankle brachial index (ABI) (r = -0.48, P = 0.001) and a significant positive correlation with glycated hemoglobin (HbA1c) level (R2 = 26, P = 0.004). Complex PAD was found in nearly half of the patients with 48% having TASC II C or D classes. Those with TASC II classes C and D had higher SYNTAX scores (P = 0.046).
Conclusions: Diabetic patients with more complex CAD had more complex PAD. In diabetic patients with CAD, those with worse glycemic control had higher SYNTAX scores and the higher the SYNTAX score, the lower the ABI.
Keywords: Peripheral arterial disease; Coronary artery disease; TASC II; SYNATX score
| Introduction | ▴Top |
Atherosclerosis is a systemic disease of the large and medium-sized arteries causing luminal narrowing (focal or diffuse) [1].
Patients with peripheral arterial disease (PAD) have a 2-3% chance of suffering a myocardial infarction (MI). There is a 2 - 3 times higher chance of developing angina compared to age-matched controls. Patients with PAD also exhibit an increased risk of death from cardiovascular complications [2]. This risk is the same for patients with symptomatic PAD or asymptomatic PAD. Over a 5-year period, patients with PAD have a 20% chance of suffering from a stroke or MI. Additionally, their mortality rate is 30% [3].
The AGATHA study discovered that patients with PAD in only one vascular territory had a 35% chance of having disease in at least one other territory. This information suggests that patients with PAD have a significantly greater risk of contracting cerebrovascular disease or coronary heart disease [2, 3].
By the time a patient presents with PAD, it is already severe. About 20-30% of patients with PAD also have diabetes mellitus. However, it is likely that only a fraction of PAD cases is diagnosed by asymptomatic presentations and lower degrees of PAD. To detect low degrees of PAD, a patient can be tested using an ankle brachial index (ABI) [3].
The SYNTAX score is a validated scoring system used to the assessment of complexity and anatomical severity of coronary artery disease (CAD). It correlates well with major adverse cardiovascular events and cardiovascular mortality [4, 5].
Trans-Atlantic Inter-Society Consensus II (TASC II) classification is an internationally derived definition that is dedicated for the assessment of PAD according to anatomical distribution, number, and nature of lesions [6].
In this study, we tried to find the relationship of complexity of PAD and CAD in a group of diabetic patients. Most of the available data included diabetics as well as non-diabetics.
| Materials and Methods | ▴Top |
This is a prospective cross-sectional observational study. It included 50 diabetic patients referred for elective coronary angiography with documented CAD and PAD detected by peripheral angiogram. An informed written consent was taken from each participant.
The aim of this study was to assess the relationship between CAD complexity using SYNTAX score and PAD complexity using TASC II classification in diabetic patients.
The study was approved by the local Institutional Ethical Committee of Faculty of Medicine, Ain Shams University. This study was conducted in compliance with the ethical standards of the responsible institution on human subjects as well as with the Helsinki Declaration.
Sampling
All 50 patients, in the time period from August 2016 till July 2017, were enrolled using quota sampling from patients referred for elective coronary angiogram with documented PAD by examination and confirmed by duplex ultrasound.
Inclusion criteria
Patients with chronic coronary syndrome undergoing diagnostic coronary angiography with documented CAD and PAD were included.
Exclusion criteria
Exclusion criteria included: 1) patient’s refusal, 2) vasculitis, 3) contraindication for coronary angiography (e.g., active bleeding, coagulopathy, active infection, etc.), 4) non-atherosclerotic stenosis, 5) acute limb-threatening ischemia, 6) patients with known or suspected infectious or inflammatory conditions, and 7) patients with serum creatinine more than 1.3 mg/dL.
Procedures
Procedures included: 1) History taking. 2) Complete physical examination. 3) Laboratory investigations. 4) Coronary angiography. It was performed using conventional techniques and was analyzed by experienced interventional cardiologists. 5) SYNTAX scoring. SYNTAX score was calculated using an online calculator [7]. A SYNTAX score of 0 indicates no measurable coronary disease, while a score 1 indicates the presence of CAD, with CAD complexity increasing as the SYNTAX score increases. The SYNTAX score algorithm includes: dominance; number of lesions; segments involved per lesion with lesion characteristics; total occlusions with subtotal occlusions (number of segments, age of total occlusion, blunt stump, bridge collaterals, first segment beyond occlusion visible by anterograde or retrograde filling, and side branch involvement); trifurcation, number of diseased segments; bifurcation type and angulation; aortic osteal lesion; severe tortuosity; lesion length; heavy calcification; thrombus; diffuse disease with numbers of segments. 6) Peripheral angiography and TASC II classification (Tables 1, 2 [6]). Peripheral angiography was done at the same index coronary angiography procedure by experienced interventional cardiologist for both lower limbs. It was performed using conventional techniques and was analyzed by experienced interventional cardiologists.
 Click to view | Table 1. TASC II Classification of Aortoiliac Lesions [6] |
 Click to view | Table 2. TASC II Classification of Femoral Popliteal Lesions [6] |
Statistical analysis
We used the statistical package SPSS 17. Continuous variables were reported as means ± standard deviation (SD) or as median and interquartile range (IQR) when skewed. Categorical variables were reported as percentages and compared using the χ2 test. Continuous variables were compared by the Mann-Whitney U test. Kruskal-Wallis test was used when more than two groups were compared. A P value of < 0.05 was considered statistically significant. All tests were two-sided. Correlations between continuous homogenous variables were done using Pearson correlation coefficient.
| Results | ▴Top |
Baseline characteristics
Most of the 50 diabetic patients were males (80%), hypertensives (84%) and smokers (80%). All of them had high low-density lipoprotein (LDL) levels, with mean of 157 mg/dL and the majority had uncontrolled diabetic mellitus (DM) with high levels of glycated hemoglobin (HbA1c) with mean of 8.47±1.47%. Most of the cohort had no symptoms of PAD (94%) (Table 3).
 Click to view | Table 3. Demographic and Baseline Characteristics |
SYNTAX score
The mean SYNTAX score was 19.88 ± 13.34, where 60% had a score < 22 (mild CAD), 24% had a score between 22 and 32 (moderate), and 16% had a score > 33 (severe) (Fig. 1).
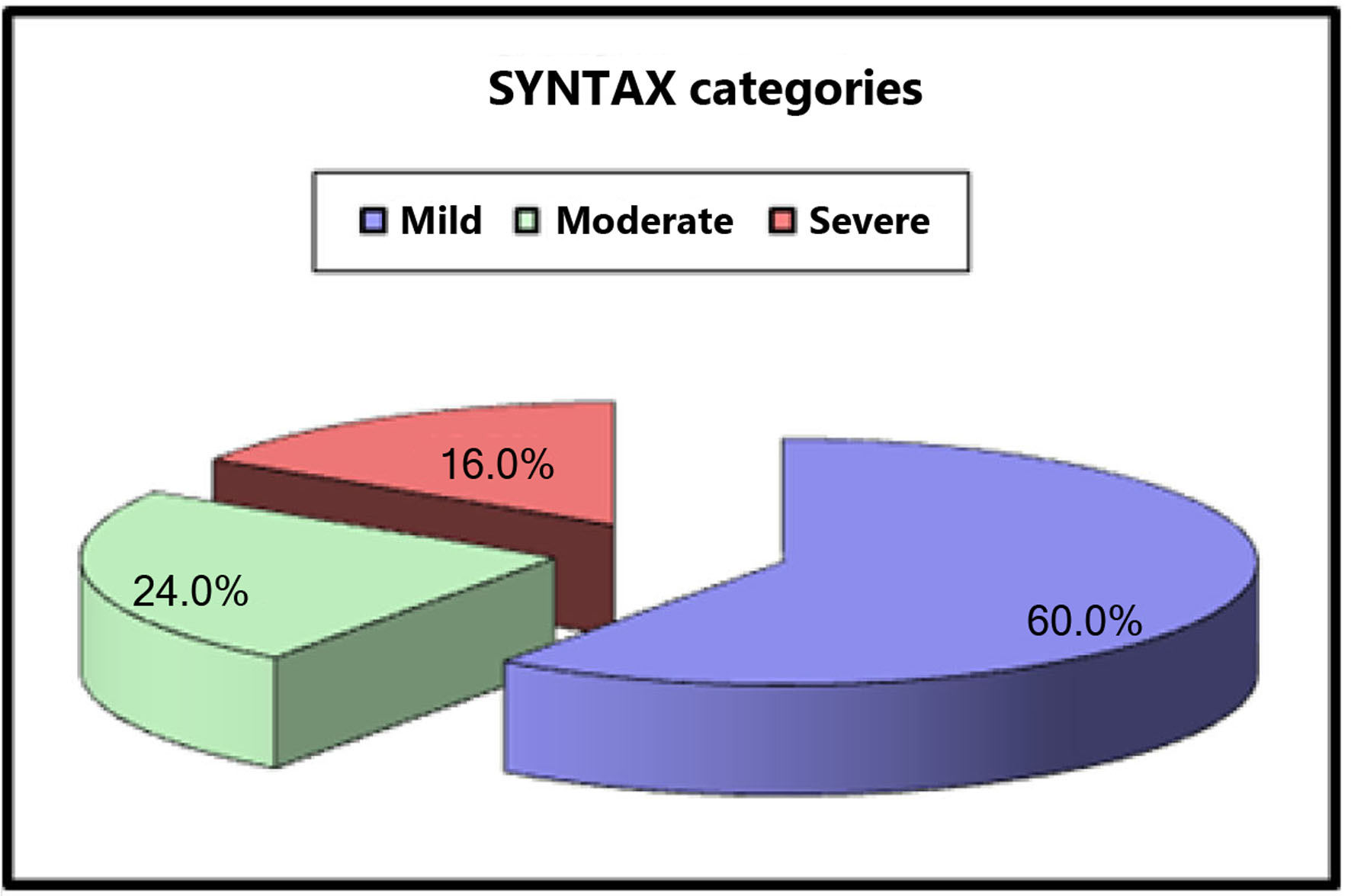 Click for large image | Figure 1. SYNTAX score categories. |
TASC II classification
The PAD classification and complexity was nearly evenly distributed with 24% TASC II A, 28% TASC II B, 22% TASC II C and 26% TASC II D (Fig. 2).
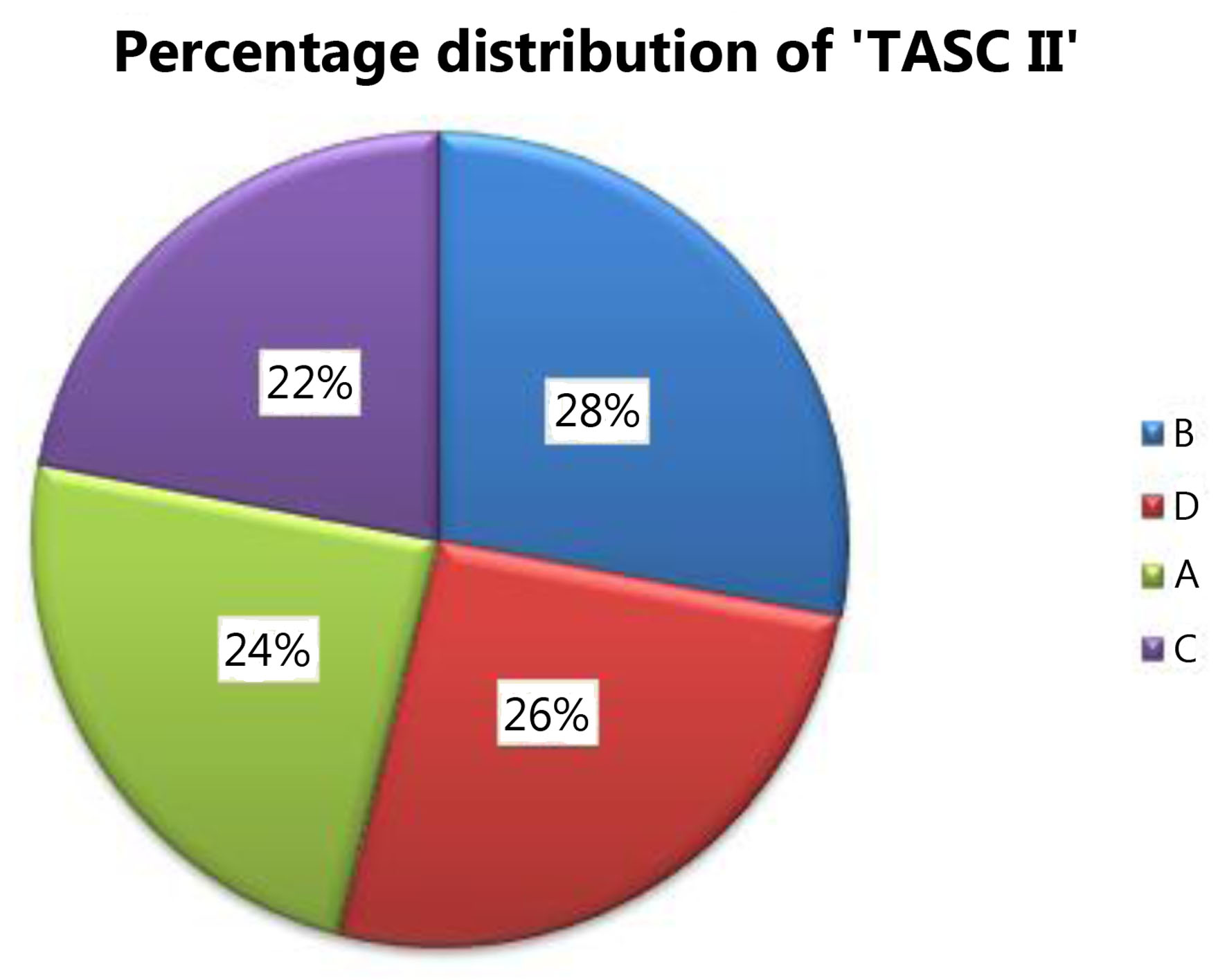 Click for large image | Figure 2. TASC II classification distribution. TASC II: Trans-Atlantic Inter-Society Consensus II. |
Relationship between complexity of CAD and PAD
Complex PAD anatomy represented by TASC II C and D classes showed higher SYNTAX scores (P = 0.046) (Fig. 3, Table 4).
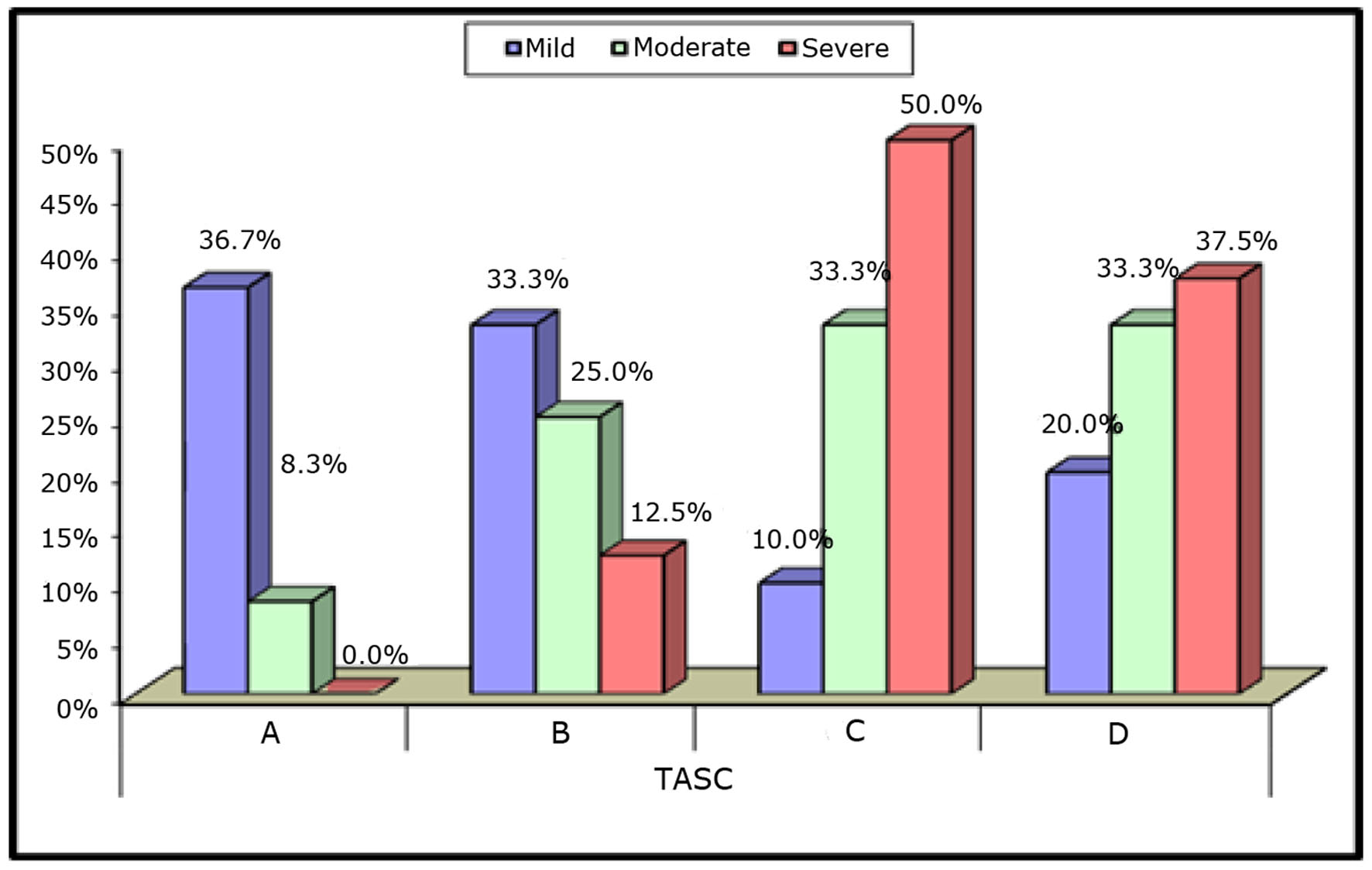 Click for large image | Figure 3. Relation between SYNTAX scores and TASC II classification. TASC II: Trans-Atlantic Inter-Society Consensus II. |
 Click to view | Table 4. SYNTAX Versus TASC II Class |
The highest median (IQR) SYNTAX score in patients with TASC II class C was 26.5 (19 - 36) (P < 0.001) (Fig. 4).
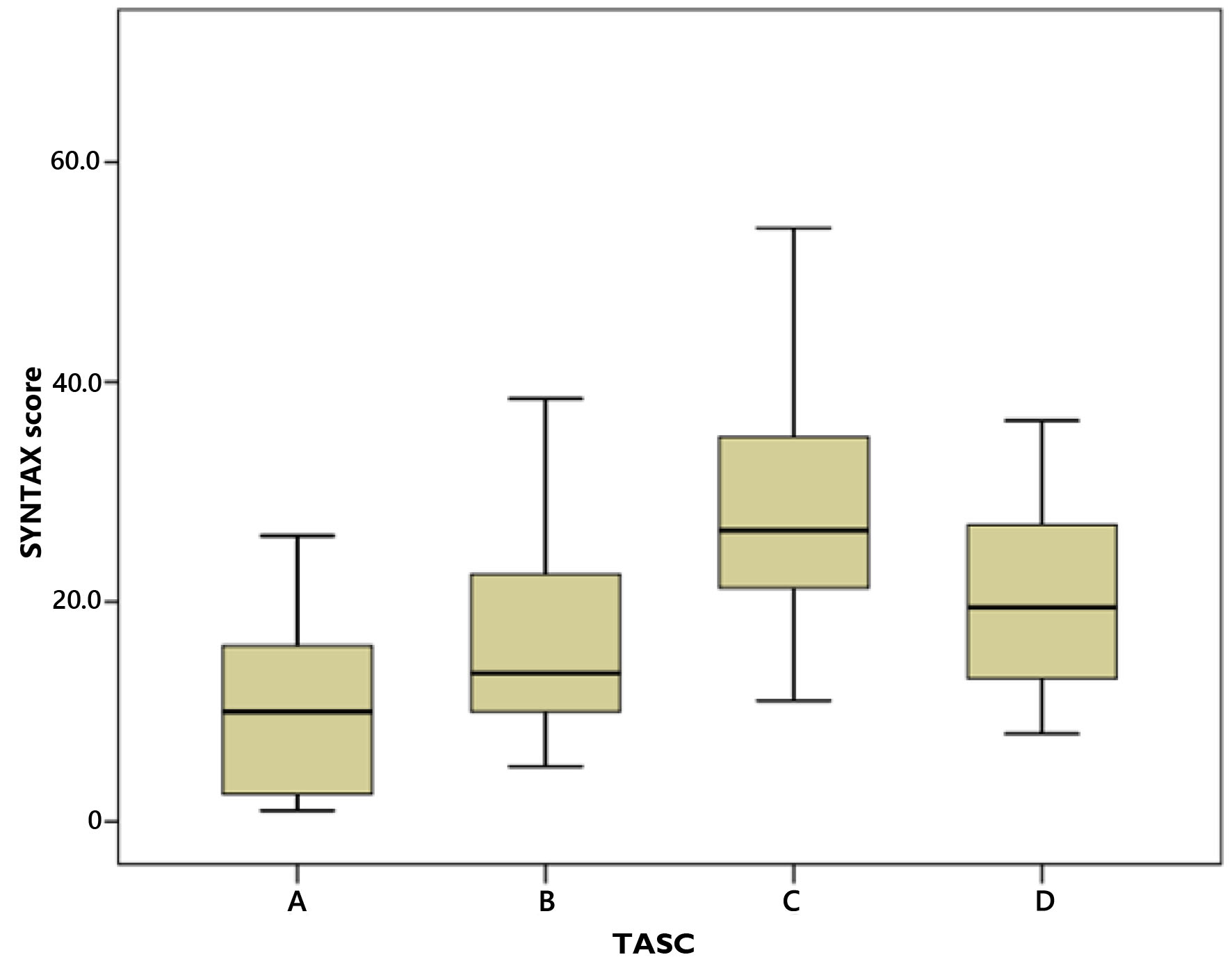 Click for large image | Figure 4. Relation between SYNTAX scores IQR and TASC II classification. IQR: interquartile range; TASC II: Trans-Atlantic Inter-Society Consensus II. |
Relationship between complexity of PAD and ABI
The mean ABI was 0.8 ± 0.07 which is lower with increased complexity of the PAD as shown in Table 5, where all the patients in TASC II D class had low ABI < 0.9 (P = 0.001).
 Click to view | Table 5. TASC II Class and ABI |
Relationship between complexity of CAD and ABI
The higher the SYNTAX score, the lower the ABI with a significant negative correlation between SYNTAX score and ABI with correlation coefficient of -0.48 and R2 of 23 (P < 0.001) (Fig. 5).
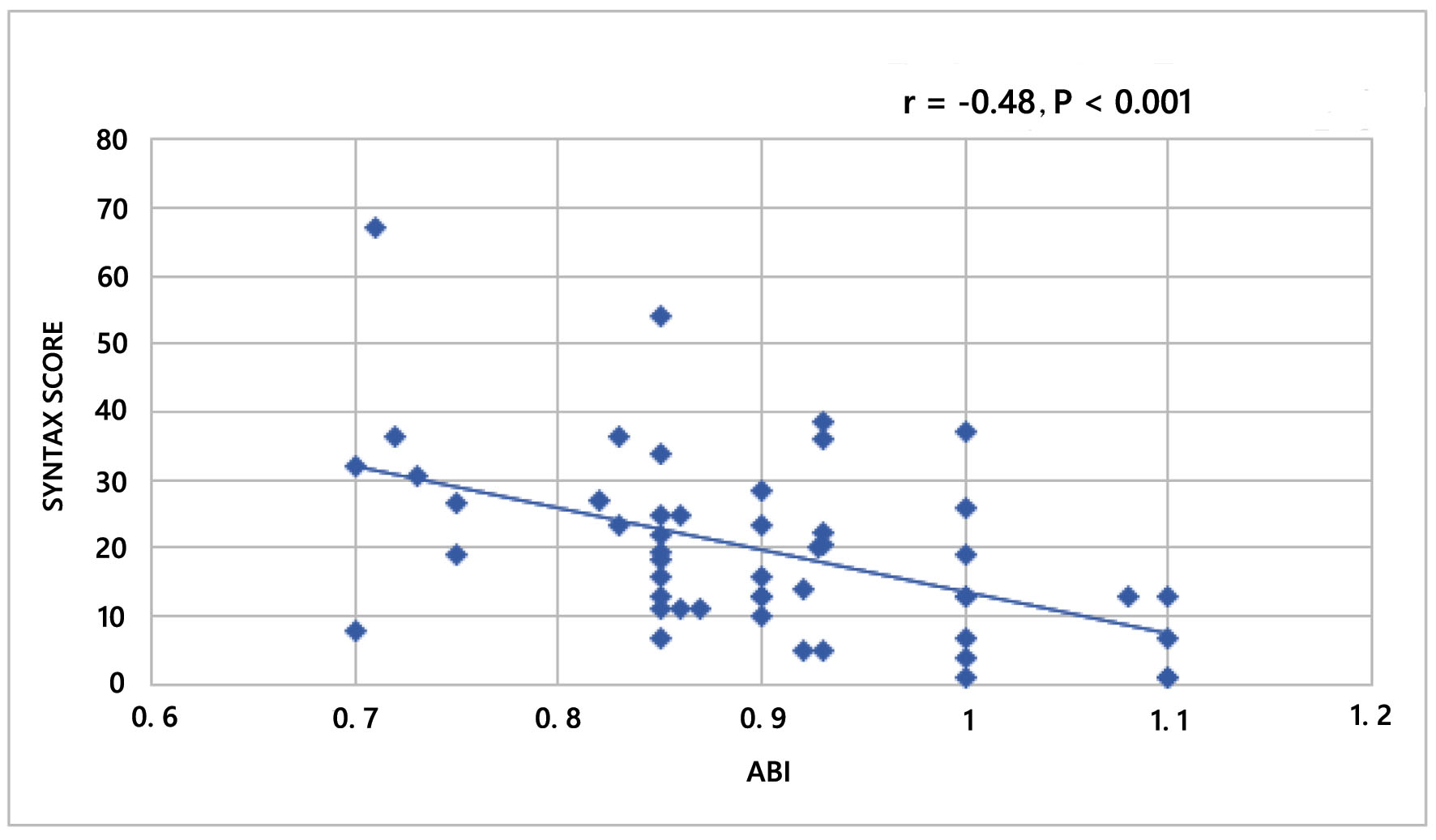 Click for large image | Figure 5. Correlation between SYNTAX score and ABI. ABI: ankle brachial index. |
Relationship between complexity of CAD and HbA1c
The higher the HbA1c, the higher the SYNTAX score with a significant positive correlation between SYNTAX score and HbA1c with correlation coefficient of 0.51 and R2 of 26 (P < 0.01) (Fig. 6).
 Click for large image | Figure 6. Correlation between SYNTAX score and HbA1c. HbA1c: glycated hemoglobin. |
| Discussion | ▴Top |
In this prospective cross-sectional observational study, we investigated the relationship between the complexity of CAD assessed by SYNTAX score and the complexity of associated PAD assessed by TASC II class in a group of diabetic patients with normal kidney functions.
Baseline characteristics
Most of the studied Egyptian cohort were males, smokers, hypertensives, with high LDL levels and inadequate glycemic control. Where these represent the traditional risk factors for atherosclerosis with high prevalence among the studied group, they were shown in the registry published by Shaheen et al [8] in the European Society of Cardiology Registry on ST elevation MI; compared to other countries, Egyptian patients had higher prevalence of traditional risk factors.
Relationship between complexity of CAD and PAD
Complex PAD anatomy represented by TASC II C and D classes showed higher SYNTAX scores. The median SYNTAX scores of diabetic patients with TASC II A, TASC II B, TASC II C, and TASC II D were 10, 13.5, 26.5, and 19.5, respectively, compared with the results in the study by Aykan et al [9]. They studied 449 patients, 30% of whom had diabetes. They found that patients with TASC II A, TASC II B, TASC II C, and TASC II D had median SYNTAX scores of 13.25, 14, 19, and 19, respectively. These findings were relatively higher in diabetic patients. Vuruskan et al [10] developed a scoring system (total peripheral score (TPS)) using the TASC II classification and the SYNTAX II score to predict CAD severity in patients with lower extremity arterial disease. They showed a modest positive correlation between TPS and SYNTAX (Pearson correlation = 0.467, P < 0.001).
Relationship between complexity of CAD and glycemic control
In the current study, mean HbA1c was 8.47% (higher than the target value in current guidelines) and was significantly positively correlated with CAD severity as represented by the SYNTAX score. The higher the HbA1c level, the higher the SYNTAX score.
Our results were consistent with similar findings by Dar et al [11]. They studied the prevalence of type 2 DM and association of HbA1c with severity of CAD in patients presenting as non-diabetic acute coronary syndrome and found a significant positive correlation between HbA1c and CAD complexity represented by Gensini score.
Study limitations
The main limitation of this study is being a single-center trial with relatively limited number of participants. A larger number of enrolled patients in the study population can also result in a higher positive correlation to be obtained in future studies.
The exclusion of patients with renal impairment also removed an important risk factor in diabetic patients with atherosclerotic CAD.
Conclusions
Diabetic patients with more complex CAD had more complex PAD. In diabetic patients with CAD, those with worse glycemic control had higher SYNTAX scores and the higher the SYNTAX score, the lower the ABI.
Acknowledgments
None to declare.
Financial Disclosure
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of Interest
The authors declare that they have no conflict of interest.
Informed Consent
No data were collected before detailed information was given to the patient and a written consent was obtained.
Author Contributions
KA conceptualized the project, reviewed the literature, collected the data, analyzed the data, and wrote the manuscript. HF conceptualized the project and collected the data. AE conceptualized the project, reviewed the literature, collected the data, and analyzed the data. SS conceptualized the project and reviewed the literature. All authors read and approved the final manuscript.
Data Availability
The data used to support the findings of this study are available from the corresponding author upon request.
Abbreviations
AAA: abdominal aortic aneurysm; ABI: ankle brachial index; ACS: acute coronary syndrome; CA: coronary angiography; CAD: coronary artery disease; CFA: common femoral artery; CIA: common iliac artery; DM: diabetes mellitus; EIA: external iliac artery; IQR: interquartile range; LDL: low-density lipoprotein; LVEF: left ventricular ejection fraction; MI: myocardial infarction; PAD: peripheral arterial disease; SFA: superficial femoral artery; TASC II: Trans-Atlantic Inter-Society Consensus II
| References | ▴Top |
- Writing Committee to Develop Clinical Data Standards for Peripheral Atherosclerotic Vascular Disease, Creager MA, Belkin M, Bluth EI, Casey DE, Jr., Chaturvedi S, Dake MD, et al. 2012 ACCF/AHA/ACR/SCAI/SIR/STS/SVM/SVN/SVS key data elements and definitions for peripheral atherosclerotic vascular disease: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Clinical Data Standards (Writing Committee to Develop Clinical Data Standards for Peripheral Atherosclerotic Vascular Disease). Circulation. 2012;125(2):395-467.
doi pubmed - Fowkes FG, Low LP, Tuta S, Kozak J, Investigators A. Ankle-brachial index and extent of atherothrombosis in 8891 patients with or at risk of vascular disease: results of the international AGATHA study. Eur Heart J. 2006;27(15):1861-1867.
doi pubmed - Thiruvoipati T, Kielhorn CE, Armstrong EJ. Peripheral artery disease in patients with diabetes: Epidemiology, mechanisms, and outcomes. World J Diabetes. 2015;6(7):961-969.
doi pubmed - Sianos G, Morel MA, Kappetein AP, Morice MC, Colombo A, Dawkins K, van den Brand M, et al. The SYNTAX Score: an angiographic tool grading the complexity of coronary artery disease. EuroIntervention. 2005;1(2):219-227.
- Serruys PW, Onuma Y, Garg S, Sarno G, van den Brand M, Kappetein AP, Van Dyck N, et al. Assessment of the SYNTAX score in the Syntax study. EuroIntervention. 2009;5(1):50-56.
doi pubmed - Norgren L, Hiatt WR, Dormandy JA, Nehler MR, Harris KA, Fowkes FG, TASC II Working Group. Inter-Society Consensus for the Management of Peripheral Arterial Disease (TASC II). J Vasc Surg. 2007;45(Suppl S):S5-67.
doi pubmed - http://www.syntaxscore.com.
- Shaheen S, Wafa A, Mokarab M, Zareef B, Bendary A, Abdelhameed T, Rashwan A, et al. Presentation, management, and outcomes of STEMI in Egypt: results from the European Society of Cardiology Registry on ST elevation myocardial infarction. Egypt Heart J. 2020;72(1):35.
doi pubmed - Aykan AC, Hatem E, Karabay CY, Gul I, Gokdeniz T, Kalaycioglu E, Turan T, et al. Complexity of lower extremity peripheral artery disease reflects the complexity of coronary artery disease. Vascular. 2015;23(4):366-373.
doi pubmed - Vuruskan E, Saracoglu E, Polat M, Duzen IV. Prediction of coronary artery disease severity in lower extremity artery disease patients: A correlation study of TASC II classification, Syntax and Syntax II scores. Cardiol J. 2017;24(5):495-501.
doi pubmed - Dar MI, Beig JR, Jan I, Shah TR, Ali M, Rather HA, Tramboo NA. Prevalence of type 2 diabetes mellitus and association of HbA1c with severity of coronary artery disease in patients presenting as non-diabetic acute coronary syndrome. Egypt Heart J. 2020;72(1):66.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cardiology Research is published by Elmer Press Inc.


