| Cardiology Research, ISSN 1923-2829 print, 1923-2837 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, Cardiol Res and Elmer Press Inc |
| Journal website https://www.cardiologyres.org |
Short Communication
Volume 14, Number 1, February 2023, pages 69-78
The Effects of Percutaneous Coronary Intervention on Biomarkers and Quality of Life in Patients With Chronic Total Coronary Artery Obstruction
I. Made Junior Rina Arthaa, f , I. Made Baktab
, Ida Bagus Putra Manuabac
, I. Wayan Witaa
, Mohammad Saifur Rohmand
, I. Nyoman Mantik Astawae
, Agha Bhargaha
aCardiology and Vascular Medicine Department, Faculty of Medicine, Universitas Udayana-Prof. I.G.N.G. Ngoerah General Hospital, Denpasar, Bali, Indonesia
bInternal Medicine Department, Faculty of Medicine Universitas Udayana-Prof. I.G.N.G. Ngoerah General Hospital, Denpasar, Bali, Indonesia
cFaculty of Chemistry and Science, Universitas Udayana, Denpasar, Bali, Indonesia
dDepartment of Cardiology, Universitas Brawijaya-Saiful Anwar Hospital, Malang, Indonesia
eVirology Laboratory, Department of Animal Disease, Faculty of Veterinary Medicine, Universitas Udayana, Bali, Indonesia
fCorresponding Author: I. Made Junior Rina Artha, Cardiology and Vascular Medicine Department, Faculty of Medicine, Universitas Udayana-Prof. I.G.N.G. Ngoerah General Hospital, Denpasar, Bali, Indonesia
Manuscript submitted November 24, 2022, accepted February 2, 2023, published online February 25, 2023
Short title: Effects of PCI on Biomarkers in CTO Patients
doi: https://doi.org/10.14740/cr1455
| Abstract | ▴Top |
Background: Chronic total occlusion (CTO) is an angiographic picture of total occlusion without blood flow which is estimated to have lasted at least 3 months. This study attempted to provide an overview of the levels of matrix metalloproteinase-9 (MMP-9), soluble suppression tumorigenicity 2 (sST2), and N-terminal pro-B-type natriuretic peptide (NT-pro-BNP) as remodeling, inflammatory, and atherosclerotic markers, as well as changes in the angina severity in patients with CTO who underwent percutaneous coronary intervention (PCI) compared to those without PCI.
Methods: This study is a preliminary report with quasi-experimental design study with a pre-test and post-test approach to compare PCI’s effect in CTO patients towards changes in MMP-9, sST2, NT-pro-BNP levels, and changes in the angina severity. Twenty subjects underwent PCI and 20 subjects with optimal medical therapy, who were then assessed at baseline and 8 weeks after intervention.
Results: The results of this preliminary report showed that decreased MMP-9 (pre-test: 12.07 ± 1.27 ng/mL vs. post-test: 9.91 ± 5.19 ng/mL, P = 0.049), sST2 (pre-test: 37.65 ± 20.00 ng/mL vs. post-test: 29.74 ± 15.17 ng/mL, P = 0.026) and NT-pro-BNP (pre-test: 0.63 ± 0.23 ng/mL vs. post-test: 0.24 ± 0.10 ng/mL, P < 0.001) levels were found after 8 weeks of PCI compared to those without such intervention. The levels of NT-pro-BNP were lower in the PCI group (0.24 ± 0.10 ng/mL) than in the non-PCI group (0.56 ± 0.23 ng/mL; P < 0.001). Moreover, there was an improvement of angina severity in PCI group than without PCI (P < 0.039).
Conclusions: Although this preliminary report found a significant decrease in MMP-9, NT-pro-BNP, and sST2 levels in CTO patients who had undergone PCI compared to those without PCI, as well as improved angina severity in these patients, this study still has limitations. The number of samples was so small that similar studies with larger sample sizes or multicenter investigations are required to deliver more trustworthy and useful results. Nevertheless, we encourage this study as a preliminary baseline for further studies in the future.
Keywords: Coronary intervention; Chronic total obstruction; MMP-9; NT-pro-BNP; sST2
| Introduction | ▴Top |
Chronic total occlusion (CTO) is an angiographic picture of total occlusion without blood flow or thrombolysis in myocardial infarction score of 0 (TIMI 0), which is estimated to have lasted at least 3 months [1]. CTO incidence is found in 20-30% of coronary heart disease patients who undergo coronary angiography examination, and the majority of CTO patients have no history of myocardial infarction [2]. The formation of collateral vessels to compensate for worsening arterial occlusion appears to reduce myocardial damage so that it causes no symptoms or only mild clinical symptoms [3].
Histopathologically, thrombotic lesions that clog arteries develop over time from “soft” plaques to “hard” lesions [4]. The severity and extent of hard plaque calcification increase with the duration of CTO formation [4]. Collagen, which is the main component of fibrous tissue that acts as an occlusive barrier, will also increase over time; and this is one of the reasons for the technical difficulties involved in percutaneous coronary intervention (PCI) procedures with high failure (15-32%) compared to procedures for non-occlusive lesions (around 3%) [5-7].
Therapy using a PCI approach in CTO patients is still a needed technique and is considered at the forefront of coronary intervention. Referrals of patients with CTO to undergo PCI are still low in many countries, although success rates have reached more than 80% in Japan, USA, and Europe [8]. The benefits of PCI in CTO are considered controversial for three main reasons. First, PCI at CTO is considered technically difficult by interventional cardiologists, with a lower success rate than other coronary lesions. Second, the Occluded Artery Trial (OAT) clinical trial demonstrated a little benefit of PCI over medical therapy in patients with occluded arteries after acute myocardial infarction (AMI) [9]. Third, the PCI procedure can last several hours with high radiation exposure, contrast agents, and costs. In patients with CTO, the indication for coronary angiography and interventional revascularization is associated with clinical symptoms experienced [10].
Measurement of biomarker levels can be used to determine the prognosis of CTO patients and risk stratification in patients with cardiovascular disease. Biomarkers that play a role in markers of the disease course of CTO vary widely. There are remodeling and inflammatory markers (matrix metalloproteinase (MMP), C-reactive protein, N-terminal pro-B-type natriuretic peptide (NT-pro-BNP), and interleukin (IL)-2) and atherogenesis and remodeling markers (soluble suppression tumorigenicity 2 (sST2)). These biomarkers are important markers in the pathogenesis and prognostic factors of cardiovascular disease mortality, development of CTO lesions, and the acute incidence of myocardial infarction [11].
B-type natriuretic peptide (BNP) is a biomarker that has been used as a new biomarker to detect coronary heart disease in the last decade. BNP levels greatly increase in acute coronary syndromes due to increased ventricular wall stress caused by ischemia or infarction [10]. NT-pro-BNP is known as the N-terminal form of circulating BNP that circulates longer in the blood and is a biomarker that has prognostic value in predicting death from cardiovascular disease [12]. A revascularization study found findings supporting an increase in the NT-pro-BNP biomarker due to ischemia as evidenced by a transient increase in balloon inflation through the PCI intervention (when ischemia occurs), and a decrease in NT-pro-BNP levels when ischemia resolves [13]. In the research conducted by Gupta et al, regarding the role of NT-pro-BNP biomarkers in patients with stable coronary heart disease undergoing PCI procedures, it was shown that there was a change in the NT-pro-BNP value at 8 weeks post-PCI (pre-test: 224.36 pg/mL; post-test: 168.68; P = 0.016). However, in this study, there was still no change in cardiac function from echocardiographic parameters such as ejection fraction, ventricular filling function, and ventricular mass which were examined before and 8 weeks after PCI [10].
MMP function is to degrade the extracellular matrix and reduce plaque stability. Increased MMP expression has been found in atherosclerotic lesions and plays an important role in extracellular remodeling, atheroma formation, and plaque rupture [14]. In particular, MMP-2 and MMP-9 are associated with coronary atherosclerotic plaque remodeling [15]. More specifically, MMP-9 has a role in the degradation of coronary artery plaque, making it easier for it to undergo a rupture and subsequent remodeling to become a chronic obstructive lesion [15]. A 15-year cohort study conducted by Eldrup et al on the role of the MMP-9 biomarker on the risk of AMI and unstable angina pectoris found that MMP-9 values greater than 37 ng/mL were associated with a 38% greater risk of developing AMI, compared with people whose MMP-9 is lower than the predefined cut-off value [16]. Patients with CTO were found to have elevated levels of NT-pro-BNP and MMP-9 in the blood. This condition characterizes the presence of recurrent ischemic episodes, and the high levels of these two biomarkers can be used to predict the patient’s clinical outcome. Various medical interventions or therapies that can reduce NT-pro-BNP and MMP-9 are logically able to improve clinical outcomes in patients with CTO [17].
sST2 is a recent biomarker in coronary heart disease that can act as a decoy receptor and abolish the effects of the IL-33/ST2L complex, thereby causing loss of cardioprotective effects, which leads to heart fibrosis, accelerated atherogenesis, and inflammation [18]. A study by Dieplinger et al who examined serum sST2 in patients with stable coronary artery disease, found higher serum sST2 in the deceased group than in the survival group (21.4 vs. 18.5 ng/mL, P < 0.001); and serum sST2 greater than 24.6 ng/mL was associated with a 60% chance of 12-year survival compared with patients who had an sST2 < 15.6 ng/mL, i.e., with a 90% survival probability [19]. It suggests a significant role of sST2 in coronary heart disease.
The presence of total chronic blockage causes total obstruction of the coronary artery pathways, which causes tissue ischemia; this will cause a symptom of refractory chest pain (refractory angina), which is very common and provides discomfort. It contributes to the decreased quality of life of CTO patients [20]. PCI procedure is known to be beneficial in patients with CTO. At the vascular level, PCI is able to overcome obstruction that occurs in the coronary arteries and at the tissue level. PCI is able to improve ischemia conditions that occur so that it will lead to improvement of heart function, chronic inflammation, and remodeling in cardiomyocytes. A study conducted by Hirai et al, who assessed changes in quality of life in CTO patients with refractory angina (angina that did not go away with medical therapy) evaluated by the Seattle Angina Questionnaire (SAQ), found that the PCI group had improvements in angina frequency, quality of life, and satisfaction with therapy taken compared to the group without CTO [21].
The current studies on CTO patients comparing the benefits of PCI and other medical therapies are still limited to evaluating changes in echocardiographic parameters, mortality, recurrence of infarction, chest pain symptoms, and quality of life. There are still no studies evaluating the levels of MMP-9, sST2, and NT-pro-BNP as remodeling, inflammatory, and atherosclerotic biomarkers in CTO cases. Based on the description above, this study aims to fill the knowledge gap at the bio-molecular level by comparing the levels of these biomarkers in CTO patients, who received PCI with patients without PCI and comparing the improvement in the quality of life of patients with angina components.
| Materials and Methods | ▴Top |
Ethical clearance
All procedures performed in this study were reviewed and approved by the ethical committee standard of Prof. I.G.N.G. Ngoerah General Hospital following the Declaration of Helsinki (2013) (letter of exemption with approval number: 2567/UN14.2.2.VII.14/LT/2020).
Population subject
It is a preliminary report with a quasi-experimental design, and with a pre-test and post-test approach to compare the effect of PCI in CTO patients. Forty subjects were recruited from January through June 2019. The inclusion criteria in this study were: 1) coronary heart disease (CHD) patients who showed CTO on coronary angiography that involved only one coronary artery branch occlusion; 2) patients who were willing to sign the informed consent of the study to undergo elective PCI; 3) patients who did not have heart failure abnormalities; 4) age between 40 and 70 years; 5) not in the acute phase of myocardial infarction; 6) not having abnormalities on the 12-lead electrocardiography (ECG) (signs of acute ischemia in the form of ST-elevation or ST depression); 7) left ventricular ejection fraction (LVEF) > 50%; 8) angiography with critical stenosis > 90%; and 9) normal valvular function. Based on the included samples, patients who were: 1) with multi-vessel disease; 2) with stage V renal failure requiring regular hemodialysis; 3) with malignancy; 4) with conditions that do not allow elective PCI intervention; and 5) with diastolic dysfunction (> grade 1) on echocardiography, should be excluded from the study sample.
Data collection
The selected sample was divided first into the PCI group and the non-PCI group (undergoing optimal medical therapy (OMT)). After signing the informed consent, the patient who will undergo PCI performs a preoperative procedure in which the first blood collection is carried out and then stored before PCI to measure the levels of MMP-9, sST2, and NT-pro-BNP; while blood collection of patients without PCI was carried out at the Clinical Pathology Laboratory, Prof. I.G.N.G. Ngoerah General Hospital. Blood samples obtained for examination of NT-pro-BNP, sST2, and MMP-9 were centrifuged at 1,550 g for 10 min, then stored at a temperature of -30 °C until the assay is carried out. This examination was performed using an analyzer (Roche Diagnostic, Manheim, Germany) and enzyme-linked immunosorbent assay (ELISA) kit for human NT-pro-BNP, sST2, and MMP-9 (Elabsciences, Houston, Texas). The PCI procedure was carried out in the Catheterization Laboratory of the Integrated Cardiac Service Unit, Prof. I.G.N.G. Ngoerah General Hospital, which was taken by a consultant in interventional cardiology at Prof. I.G.N.G. Ngoerah General Hospital, Denpasar. The procedure was performed through access to the radial/femoral artery, which was preceded by coronary angiography to determine the location of the CTO. The CTO lesion was then mechanically broken using CTO wire escalation. PCI was considered successful by confirming coronary angiography where residual stenosis < 20% was found, stent deployment was successful, and no complications. The stent was placed using several PCI balloons during the PCI procedure, and a drug-eluting stent was inserted; optimum medical treatment was performed using an angiotensin-converting enzyme (ACE)-inhibitor, beta-blocker, and dual antiplatelet, statin, and mineralocorticoid receptor antagonist (MRA) following the OMT procedure. Patients who failed the PCI procedure (the wire did not penetrate the lesion and the stent deployment was not successful) would be included in the group without PCI.
In patients without PCI (patients who refused PCI and failed PCI), optimal medical treatment was carried out using ACE-inhibitors, beta-blockers, dual antiplatelets, statins, nitrates, and aldosterone receptors antagonists according to OMT management procedures. Follow-up was carried out every 2 weeks in outpatient clinic conditions; this effort reduces a loss to follow-up. At week 8, after the phase I measurement of the biomarker, the patient was again called for a phase II measurement. Re-measurement of levels of MMP-9, sST2, NT-pro BNP, and quality of life, 8 weeks after phase I measurements were taken, in the PCI group, either electively or without PCI (OMT) at the Clinical Pathology Laboratory, Prof. I.G.N.G. Ngoerah General Hospital.
Statistical analysis
Statistical data analysis was performed using SPSS 23 software (Armonk, NY: IBM Corp.). We used Chi-square to analyze the categorical data and used t-test and Mann-Whitney to compare the numerical data in two groups for the bivariate analysis.
| Results | ▴Top |
In this study, 40 research subjects were included, consisting of groups of successful PCI and without PCI in the same amount, namely 20 people each. Characteristics of the study subject are described in Table 1.
 Click to view | Table 1. Baseline Characteristics of the Subject |
Furthermore, the basic blood laboratory parameters were also examined, which can be seen in Table 2. The characteristics of laboratory parameters in this study did not show any significant differences in the components of hemoglobin, total cholesterol, high-density lipoprotein (HDL) cholesterol, low-density lipoprotein (LDL) cholesterol, triglycerides, urea, and creatinine between the PCI and without PCI groups (P > 0.05).
 Click to view | Table 2. Blood Laboratory Test |
The levels of MMP-9, NT-pro-BNP, and sST2 were examined at initial conditions and 8 weeks afterward. In baseline conditions, serum MMP-9, sST2, and NT-pro-BNP levels in the PCI group (12.07 ± 1.27 ng/mL; 37.65 ± 20.00 ng/mL; and 0.63 ± 0.23 ng/mL, respectively) were not significantly different compared to the group without PCI (11.36 ± 1.51 ng/mL; 37.63 ± 15.39 ng/mL; and 0.49 ± 1.93 ng/mL, respectively) (P > 0.05), (Table 3). After 8 weeks, the three biomarker parameters were measured again. The results showed that the mean level of MMP-9 in the PCI group was 9.91 ± 5.19 ng/mL, and in the group without PCI 11.69 ± 6.51 ng/mL (P = 0.045). Significant differences (P < 0.05) were also found in the mean levels of sST2 and NT-pro-BNP in the PCI group (29.74 ± 15.17 ng/mL and 0.24 ± 0.10 ng/mL, respectively) and in the group without PCI 34.03 ± 20.24 ng/mL, P = 0.045; and 0.56 ± 0.23 ng/mL, P < 0.001, respectively (Table 4). The schematic differences in the levels of the three biomarkers can be seen here (Figs. 1-3).
 Click to view | Table 3. Baseline Level of Serum MMP-9, sST2, and NT-pro-BNP in PCI and Without PCI Groups |
 Click to view | Table 4. Serum MMP-9, sST2, and NT-pro-BNP Levels in PCI and Without PCI Groups 8 Weeks Later |
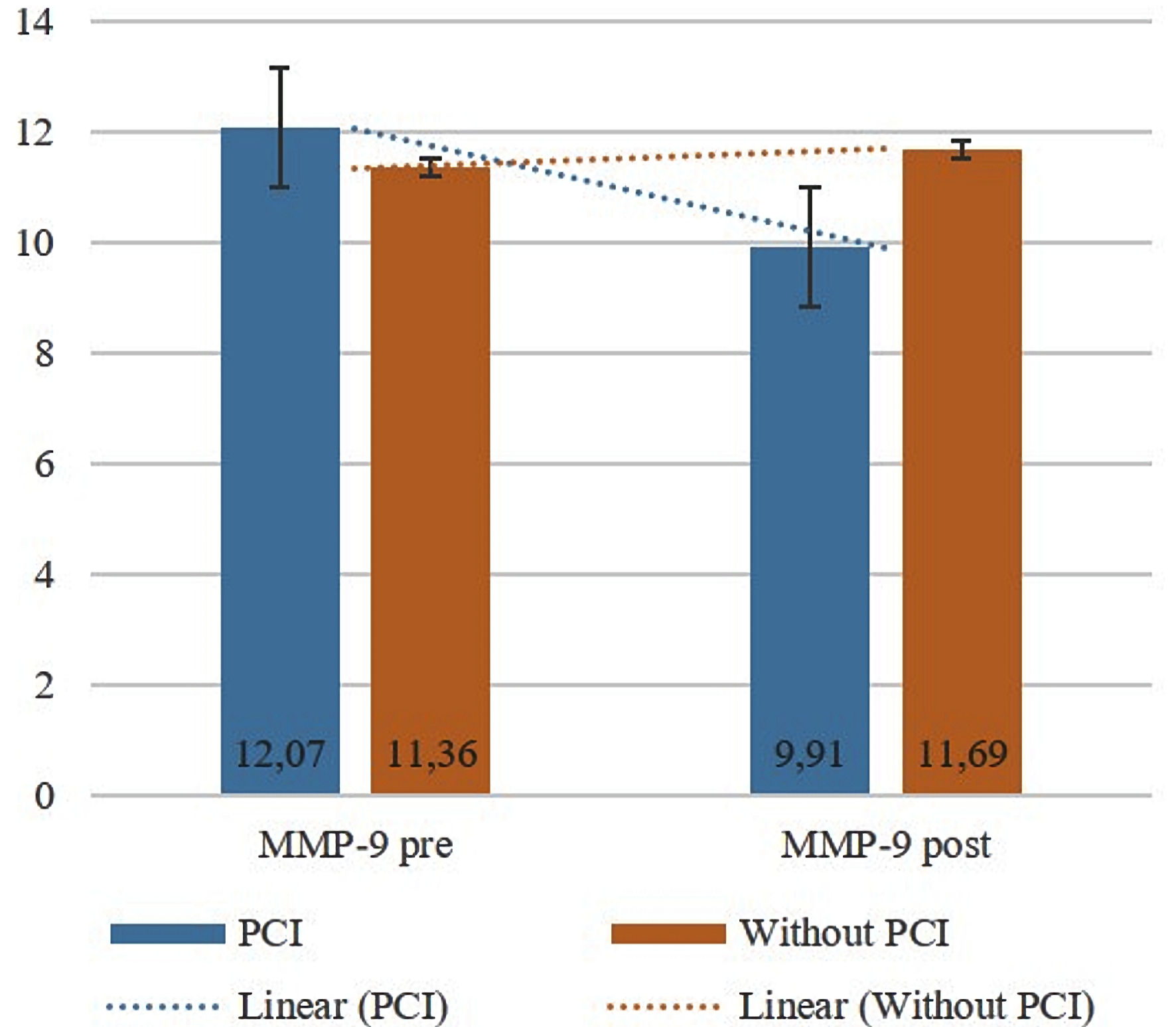 Click for large image | Figure 1. Comparison of MMP-9 levels at baseline and 8 weeks later (pre-/post-test) between the PCI and without PCI groups. Bars show the mean, and the black lines show the standard deviation. PCI: percutaneous coronary intervention; MMP-9: matrix metalloproteinase-9. |
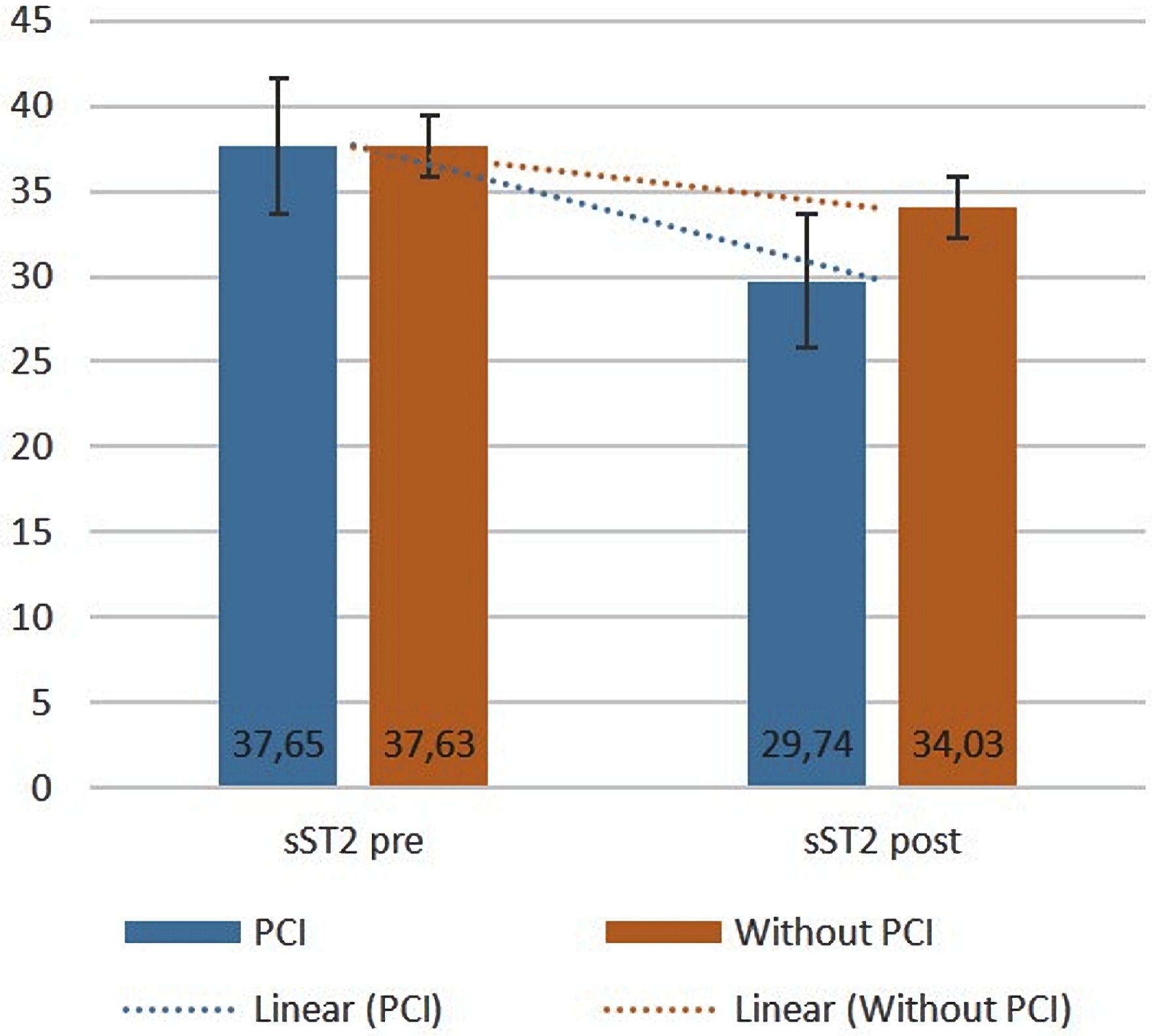 Click for large image | Figure 2. Comparison of sST2 levels at baseline and 8 weeks later (pre-/post-test) between the PCI and without PCI groups. Bars show the mean, and the black lines show the standard deviation. PCI: percutaneous coronary intervention; sST2: soluble suppression tumorigenicity 2. |
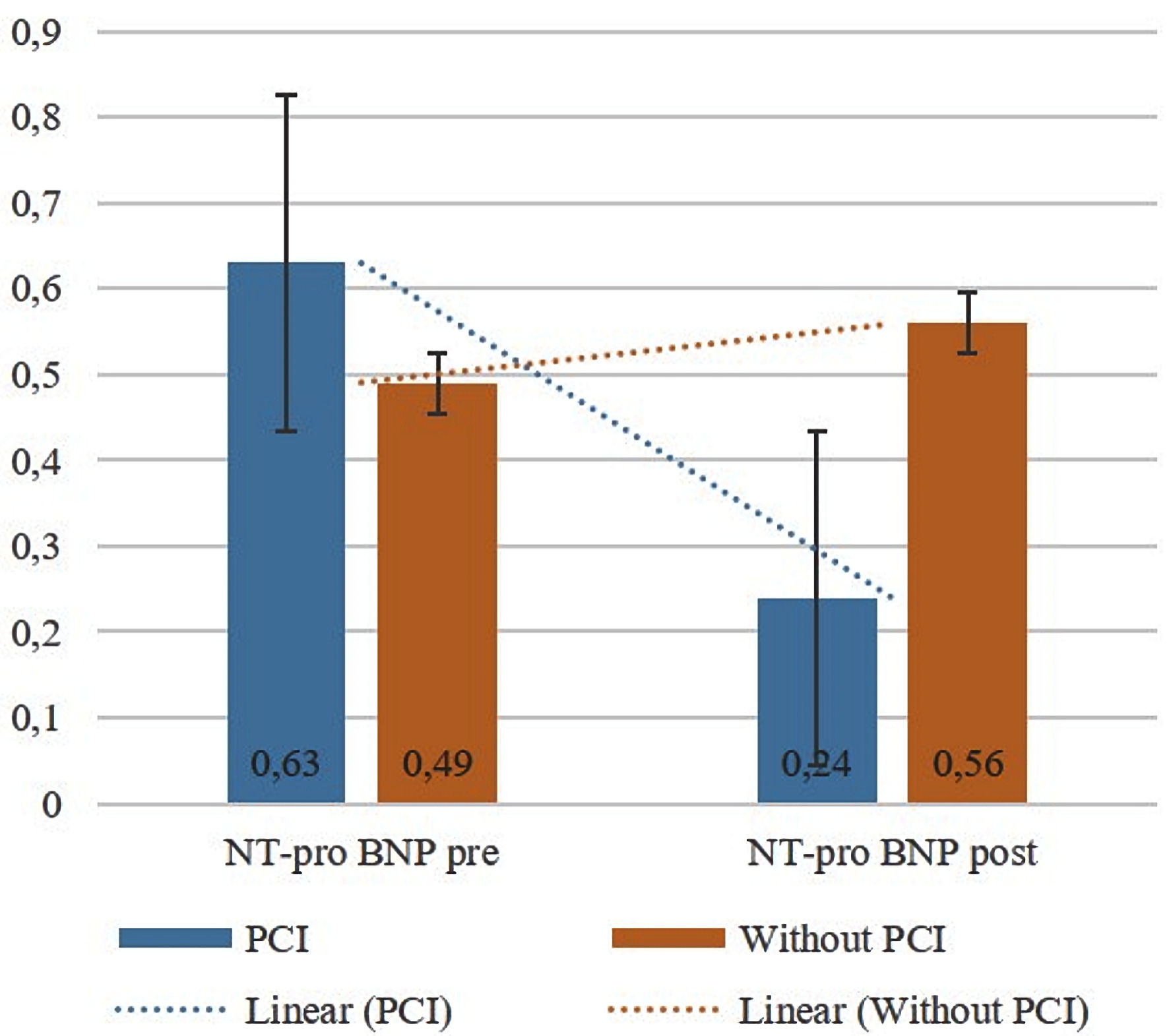 Click for large image | Figure 3. Comparison of NT-pro-BNP levels at baseline and 8 weeks later (pre-/post-test) between the PCI and without PCI groups. Bars show the mean, and the black lines show the standard deviation. PCI: percutaneous coronary intervention; NT-pro-BNP: N-terminal pro-B-type natriuretic peptide. |
The components of physical activity limitation, angina severity, therapy satisfaction, and quality of life were assessed using the SEATLE Angina questionnaire. At the initial assessment, there were no differences in physical activity limitation, angina severity, treatment satisfaction, and quality of life between the PCI and non-PCI groups (P = 0.061, P = 0.529, P = 0.151, P = 0.663, respectively). The same evaluation was carried out 8 weeks later on the same components. Significant differences between the two groups of subjects were only found in the variable of angina severity, in which the PCI group was found to have a higher score than the group without PCI (56.1 ± 3.75 vs. 52.85 ± 4.12, P = 0.039). Assessment of physical activity limitations found no significant difference between groups (68.81 ± 8.14 in PCI group vs. 64.10 ± 8.12 in non-PCI group, P = 0.063). Likewise, the assessment of therapy satisfaction and quality of life showed no significant difference between groups (53.30 ± 3.97 in PCI group vs. 51.35 ± 4.79 in non-PCI group; P = 0.169; 50.80 ± 9.34 in PCI group vs. 49.1 ± 7.19 in non-PCI group; P = 0.678). Table 5 compares the patients’ quality of life between the two groups.
 Click to view | Table 5. Comparison of Physical Activity Limitation, Angina Severity, Therapy Satisfaction, and Quality of Life Between the PCI and Without PCI Groups at Baseline and After 8 Weeks |
| Discussion | ▴Top |
Effects of PCI on lowering MMP-9, sST2, and NT-pro-BNP levels in CTO patients
The overexpression and activity of MMP-9 cause instability in atherogenic plaques through extracellular matrix degradation, proliferation, and migration of vascular smooth muscle cells [22]. Although PCI can be performed on unstable atherogenic plaques, it also impacts MMP-9 levels. In this study, it was found that there was a decrease in MMP-9 levels before PCI compared with 8 weeks after PCI. In addition, there was a significant difference in MMP-9 levels after 8 weeks in the group that received the PCI procedure and the group that did not get the PCI procedure. MMP-9 levels in the eighth week after PCI were lower than that in the group without PCI. The PCI procedure, which eliminates the chronic ischemic burden in CTO patients, will certainly impact MMP-9. It is well known that MMP-9 has a role in continuous remodeling at the vascular and cardiomyocyte levels through four phases: 1) degradation of the extracellular matrix injured by preexisting ischemic injury; 2) cell migration and angiogenesis; 3) remodeling of the extracellular matrix and scar tissue formation with a decreased force of contraction; and 4) release of cytokines and chemokines that cause further inflammatory conditions for tissue remodeling and cause ventricular dilatation and degradation of atherosclerotic plaques [23]. The loss of ischemic load due to PCI in this study was able to eliminate the cause of the remodeling cascade caused by MMP-9 (i.e., chronic ischemic load) through the four stages mentioned above, which in this study were characterized by decreased MMP-9 levels and MMP-9 levels which were lower in the PCI than in non-PCI group.
The study results found that the sST2 level in the group receiving PCI treatment was significantly lower than that without PCI. It indicates that PCI treatment can reduce serum sST2 levels in CTO patients. The results of this study are in line with the results of several previous studies. The study of Zhang et al, which evaluated the relationship of sST2 levels with the no-reflow phenomenon and long-term prognosis in non-ST-segment elevation acute coronary syndrome (NSTE-ACS) patients who received PCI, showed that the majority (76.5%) of patients had low sST2 levels (≤ 34.2 ng/mL) after underwent PCI. This study involving 205 NSTE-ACS patients also showed that high sST2 levels (> 34.2 ng/mL) were predictive factors for patient prognosis at 1 year (area under the ROC curve (AUC): 0.84; 95% confidence interval (CI): 0.75 - 0.93; P value < 0.001) with a sensitivity and specificity of 72% and 84%, respectively. This study explains that a successful PCI procedure can reduce sST2 levels and prevent the no-reflow phenomenon caused by inadequate reperfusion, associated with high levels of sST2 and poor long-term and short-term prognosis [24]. Similar results were also found in the study of Somuncu et al, which described that the increase in sST2 levels after PCI in ST-segment elevation myocardial infarction (STEMI) patients described the no-reflow phenomenon. This study showed that there were 60 (15.8%) patients who experienced complications of PCI in the form of a no-reflow phenomenon, whereas, in the group of patients who experienced the no-reflow phenomenon, higher sST2 levels were found (14.2 ± 4.6 ng/mL) compared to the group of patients who did not experience the no-reflow phenomenon (11.3 ± 5.0 ng/mL). This study found that several factors that increase the risk of the no-reflow phenomenon include diabetes mellitus (DM) (odds ratio (OR): 2.12; 95% CI: 1.09 - 4.12, P value = 0.026) and a high thrombus burden in blood vessels experiencing occlusion (OR: 2.73; 95% CI: 1.46 - 5.11; P value = 0.002) [25].
One study investigating only CTO patients showed that poorly collateralized coronary arteries were associated with significantly higher serum NT-pro-BNP levels compared with well-developed collateral coronary arteries. It is caused by the protection against myocardial ischemia provided by developing collaterals; and increased levels of NT-pro-BNP may simply reflect the humoral status required for stimulation of angiogenesis in patients with poor collateral arteries [26, 27]. Our study results showed that the mean level of NT-pro-BNP in patients undergoing PCI was lower than in patients who did not undergo PCI (0.24 ± 0.10 ng/mL vs. 0.56 ± 0.23 ng/mL, 95% CI: 0.20 - 0.4, P < 0.001). These findings indicate a significant difference in serum NT-pro-BNP levels between the group undergoing PCI and the group not undergoing PCI. The results in this study are also in line with the research conducted by Diao et al, who studied the levels of NT-pro-BNP and D-dimer in predicting no-reflow events in acute coronary syndrome patients undergoing PCI. NT-pro-BNP levels was lower at 2 h to 6 months after PCI compared to that before PCI. This study also found that NT-pro-BNP levels were higher in the no-reflow group than in the reflow group. The findings in this study indicate that preoperative levels of NT-pro-BNP in combination with D-dimer can also be used as predictive biomarkers for the incidence of no-reflow after PCI [28].
PCI improves the quality of life of CTO patients, especially in angina severity
When compared to the group without PCI, the difference of quality of life in patients receiving PCI of this study was not statistically significant (P > 0.05). The results of this study are in contrast to the study conducted by Weintraub et al, who reported an improvement in quality of life in patients who received PCI compared to those who did not, and the difference between the two groups was statistically significant. However, a significant difference was only found in the first to sixth postoperative month (P < 0.001), whereas at 12 to 36 months, there was no significant difference between the two groups [29].
Another study that summarized the results of evaluating the effectiveness of PCI compared to medication in patients with stable ischemic heart disease for 5 - 8 years has reported that PCI is more effective than OMT in improving the quality of life of patients, as measured by increasing the patient’s activity capacity and the severity of occurring angina [30]. Despite having the same outcome, the process to achieve complete relief of angina symptoms in patients treated with medication takes longer than in the PCI group. The presence of angina will impact limitations and even a decrease in inpatient activity. A recent study conducted in 2021 also confirmed that the quality of life in chronic coronary syndrome (CCS) patients was better in the group with PCI + OMT than in the group receiving OMT only (P = 0.007) [31]. In this study, only an improvement in angina symptoms was found; this could be due to a shorter observation time (8 weeks) on the quality of life in patients with CTO, which is generally assessed at 6 months.
Study limitation
The study we conducted has drawbacks. Our study has a limited time span, namely from January to June 2019. Within this limited period, we were only able to get 40 subjects in this study, which could cause subject bias. It can also affect the external validation of data if a similar study is conducted with a much larger study population. Thus, similar follow-up studies with larger sample sizes or multicenter studies need to be conducted to provide more valid and generalizable results. As a result of the limited time of the study, the parameters we examined on research subjects, which is quality of life and other related parameters, can also potentially cause bias. This is because the assessment of quality of life requires a longer time more than 8 weeks, as we did in our study. However, this research can still provide an initial picture of how PCI plays a role in improving angina severity score. In addition, this study was not blinded so that it has the potential to cause bias in sample selection.
Conclusions
Based on the results of this preliminary report, there are differences in the biomarkers of MMP-9, sST2, NT-pro-BNP, and quality of life in CTO patients undergoing PCI compared to those without PCI. In CTO patients, PCI reduced MMP-9, sST2, and NT-pro-BNP levels significantly, compared to non-PCI. Performing PCI surgery was also found to improve the quality of life of CTO patients, especially in angina severity compared to patients without PCI. Although this preliminary report found a significant decrease in those markers and improvement in angina severity score in CTO patients who had undergone PCI compared to those without PCI, this study still has limitations; namely, the sample size is so small. In order to provide more reliable and applicable results, similar follow-up studies with bigger sample numbers or multicenter studies are required.
Acknowledgments
We would like to thank all the Cath. Lab, Prof. I.G.N.G. Ngoerah General Hospital, Denpasar, Bali, Indonesia staff who were involved in this research.
Financial Disclosure
None to declare.
Conflict of Interest
All authors declare no conflict of interest regarding this research.
Informed Consent
All of study participants have given their informed consent.
Author Contributions
IMJRA contributes to defining the study concept and study design, clinical studies, manuscript review and guarantor. AB contributes to literature search, data acquisition, statistical analysis, manuscript preparation, and manuscript editing. IMB, MSR, and IWW contribute to literature search, manuscript editing, and review. IBPM and INMA contribute to statistical analysis and manuscript review.
Data Availability
The authors declare that data supporting the findings of this study are available within the article.
Abbreviations
AMI: acute myocardial infarction; BNP: B-type natriuretic peptide; CCS: chronic coronary syndrome; CTO: chronic total occlusion; ELISA: enzyme-linked immunosorbent assay; LVEF: left ventricular ejection fraction; MMP: matrix metalloproteinase; NT-pro-BNP: N-terminal pro-B-type natriuretic peptide; OAT: Occluded Artery Trial; OMT: optimal medical therapy; PCI: percutaneous coronary intervention; sST2: soluble suppression tumorigenicity 2; TIMI 0: thrombolysis in myocardial infarction score of 0
| References | ▴Top |
- Sianos G, Werner GS, Galassi AR, Papafaklis MI, Escaned J, Hildick-Smith D, Christiansen EH, et al. Recanalisation of chronic total coronary occlusions: 2012 consensus document from the EuroCTO club. EuroIntervention. 2012;8(1):139-145.
doi pubmed - Fefer P, Knudtson ML, Cheema AN, Galbraith PD, Osherov AB, Yalonetsky S, Gannot S, et al. Current perspectives on coronary chronic total occlusions: the Canadian Multicenter Chronic Total Occlusions Registry. J Am Coll Cardiol. 2012;59(11):991-997.
doi pubmed - Habib GB, Heibig J, Forman SA, Brown BG, Roberts R, Terrin ML, Bolli R. Influence of coronary collateral vessels on myocardial infarct size in humans. Results of phase I thrombolysis in myocardial infarction (TIMI) trial. The TIMI Investigators. Circulation. 1991;83(3):739-746.
doi pubmed - Srivatsa SS, Edwards WD, Boos CM, Grill DE, Sangiorgi GM, Garratt KN, Schwartz RS, et al. Histologic correlates of angiographic chronic total coronary artery occlusions: influence of occlusion duration on neovascular channel patterns and intimal plaque composition. J Am Coll Cardiol. 1997;29(5):955-963.
doi pubmed - Jaffe R, Leung G, Munce NR, Thind AS, Leong-Poi H, Anderson KJ, Qi X, et al. Natural history of experimental arterial chronic total occlusions. J Am Coll Cardiol. 2009;53(13):1148-1158.
doi pubmed - Werner GS, Hochadel M, Zeymer U, Kerber S, Schumacher B, Grube E, Hauptmann KE, et al. Contemporary success and complication rates of percutaneous coronary intervention for chronic total coronary occlusions: results from the ALKK quality control registry of 2006. EuroIntervention. 2010;6(3):361-366.
doi pubmed - Michael TT, Karmpaliotis D, Brilakis ES, Alomar M, Abdullah SM, Kirkland BL, Mishoe KL, et al. Temporal trends of fluoroscopy time and contrast utilization in coronary chronic total occlusion revascularization: insights from a multicenter United States registry. Catheter Cardiovasc Interv. 2015;85(3):393-399.
doi pubmed - Dash D. Coronary chronic total occlusion intervention: A pathophysiological perspective. Indian Heart J. 2018;70(4):548-555.
doi pubmed - Hochman JS, Lamas GA, Buller CE, Dzavik V, Reynolds HR, Abramsky SJ, Forman S, et al. Coronary intervention for persistent occlusion after myocardial infarction. N Engl J Med. 2006;355(23):2395-2407.
doi pubmed - Gupta A, Beig JR, Tramboo NA, Afroze D, Hafeez I, Rather HA. The effect of percutaneous coronary revascularization on plasma N-terminal pro-B-type natriuretic peptide levels in stable coronary artery disease. Indian Heart J. 2018;70(2):282-288.
doi pubmed - James SK, Lindahl B, Siegbahn A, Stridsberg M, Venge P, Armstrong P, Barnathan ES, et al. N-terminal pro-brain natriuretic peptide and other risk markers for the separate prediction of mortality and subsequent myocardial infarction in patients with unstable coronary artery disease: a Global Utilization of Strategies To Open occluded arteries (GUSTO)-IV substudy. Circulation. 2003;108(3):275-281.
doi pubmed - Ribeiro DG, Silva RP, Barboza DR, Lima-Junior RC, Ribeiro RA. Clinical correlation between N-terminal pro-B-type natriuretic peptide and angiographic coronary atherosclerosis. Clinics (Sao Paulo). 2014;69(6):405-412.
doi - Tateishi J, Masutani M, Ohyanagi M, Iwasaki T. Transient increase in plasma brain (B-type) natriuretic peptide after percutaneous transluminal coronary angioplasty. Clin Cardiol. 2000;23(10):776-780.
doi pubmed - Dollery CM, McEwan JR, Henney AM. Matrix metalloproteinases and cardiovascular disease. Circ Res. 1995;77(5):863-868.
doi pubmed - Pasterkamp G, Schoneveld AH, Hijnen DJ, de Kleijn DP, Teepen H, van der Wal AC, Borst C. Atherosclerotic arterial remodeling and the localization of macrophages and matrix metalloproteases 1, 2 and 9 in the human coronary artery. Atherosclerosis. 2000;150(2):245-253.
doi pubmed - Eldrup N, Kragelund C, Steffensen R, Nordestgaard BG. Prognosis by C-reactive protein and matrix metalloproteinase-9 levels in stable coronary heart disease during 15 years of follow-up. Nutr Metab Cardiovasc Dis. 2012;22(8):677-683.
doi pubmed - McClure SJ, Gall S, Schechter CB, Kearney M, Zaman AG. Percutaneous coronary revascularization reduces plasma N-terminal pro-B-type natriuretic peptide concentration in stable coronary artery disease. J Am Coll Cardiol. 2007;49(25):2394-2397.
doi pubmed - Miller AM, Liew FY. The IL-33/ST2 pathway—A new therapeutic target in cardiovascular disease. Pharmacol Ther. 2011;131(2):179-186.
doi pubmed - Dieplinger B, Egger M, Haltmayer M, Kleber ME, Scharnagl H, Silbernagel G, de Boer RA, et al. Increased soluble ST2 predicts long-term mortality in patients with stable coronary artery disease: results from the Ludwigshafen risk and cardiovascular health study. Clin Chem. 2014;60(3):530-540.
doi pubmed - Ahn JH, Yang JH, Song YB, Hahn JY, Choi JH, Lee SH, Gwon HC, et al. Impact of chronic total coronary occlusion location on long-term survival after percutaneous coronary intervention. Rev Esp Cardiol (Engl Ed). 2019;72(9):717-723.
doi pubmed - Hirai T, Grantham JA, Sapontis J, Cohen DJ, Marso SP, Lombardi W, Karmpaliotis D, et al. Quality of life changes after chronic total occlusion angioplasty in patients with baseline refractory angina. Circ Cardiovasc Interv. 2019;12(3):e007558.
doi pubmed - Li T, Li X, Feng Y, Dong G, Wang Y, Yang J. The role of matrix metalloproteinase-9 in atherosclerotic plaque instability. Mediators Inflamm. 2020;2020:3872367.
doi pubmed - Cleutjens JP, Creemers EE. Integration of concepts: cardiac extracellular matrix remodeling after myocardial infarction. J Card Fail. 2002;8(6 Suppl):S344-S348.
doi pubmed - Zhang Q, Hu M, Ma S. Association of soluble suppression of tumorigenicity with no-reflow phenomenon and long-term prognosis in patients with non-ST-segment elevation acute coronary syndrome after percutaneous coronary intervention. J Atheroscler Thromb. 2021;28(12):1289-1297.
doi pubmed - Somuncu MU, Akgun T, Cakir MO, Akgul F, Serbest NG, Karakurt H, Can M, et al. The Elevated Soluble ST2 Predicts No-Reflow Phenomenon in ST-Elevation Myocardial Infarction Undergoing Primary Percutaneous Coronary Intervention. J Atheroscler Thromb. 2019;26(11):970-978.
doi pubmed - Borekci A, Gur M, Seker T, Baykan AO, Ozaltun B, Karakoyun S, Karakurt A, et al. Coronary collateral circulation in patients with chronic coronary total occlusion; its relationship with cardiac risk markers and SYNTAX score. Perfusion. 2015;30(6):457-464.
doi pubmed - Samadov F, Yesildag O, Sari I, Atas H, Akhundova A, Basaran Y. Influence of collaterals on the left ventricular end-diastolic pressure and serum NT-proBNP levels in patients with coronary chronic total occlusion. Egypt Heart J. 2017;69(2):127-132.
doi pubmed - Diao Y, Yin M, Zhang B, Sun B. Predictive value of N-terminal pro-B-type natriuretic peptide (NT-pro BNP) combined with D-dimer for no-reflow phenomenon in patients with acute coronary syndrome after emergency of percutaneous coronary intervention. Bioengineered. 2021;12(1):8614-8621.
doi pubmed - Weintraub WS, Spertus JA, Kolm P, Maron DJ, Zhang Z, Jurkovitz C, Zhang W, et al. Effect of PCI on quality of life in patients with stable coronary disease. N Engl J Med. 2008;359(7):677-687.
doi pubmed - Blankenship JC, Marshall JJ, Pinto DS, Lange RA, Bates ER, Holper EM, Grines CL, et al. Effect of percutaneous coronary intervention on quality of life: a consensus statement from the Society for Cardiovascular Angiography and Interventions. Catheter Cardiovasc Interv. 2013;81(2):243-259.
doi pubmed - Krisnasari I, Kurnianingsih N, Rohman MS, Satrijo B, Rahimah AF. Improving quality of life with percutaneous coronary intervention in chronic coronary syndrome patients with SYNTAX score of more than 22. Hear Sci J. 2021;2(March):25-30.
doi
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cardiology Research is published by Elmer Press Inc.


