| Cardiology Research, ISSN 1923-2829 print, 1923-2837 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, Cardiol Res and Elmer Press Inc |
| Journal website https://www.cardiologyres.org |
Review
Volume 14, Number 1, February 2023, pages 22-31
Modern View on the Role of Sex-Specific Levels of High-Sensitive Cardiospecific Troponins T and I in the Diagnosis of Myocardial Infarction
aDepartment of Histology and Embryology, Department of Cardiology and Cardiovascular Surgery, Samara State Medical University, 443099 Samara, Samara Region, Russia
bResearch Institute of Cardiology, Samara State Medical University, 443099 Samara, Samara Region, Russia
cCorresponding Author: Aleksey Chaulin, Department of Histology and Embryology, Department of Cardiology and Cardiovascular Surgery, Samara State Medical University, 443099 Samara, Samara Region, Russia
Manuscript submitted November 15, 2022, accepted January 13, 2023, published online February 25, 2023
Short title: Cardiospecific Troponins T and I in MI
doi: https://doi.org/10.14740/cr1450
- Abstract
- Introduction
- Cardiospecific Troponins: Biochemistry and Physiological Role
- High-Sensitive Cardiospecific Troponins: Characteristics of Detection Methods and Important Analytical Parameters
- Sex Specificities of Cardiospecific Troponin Levels
- Possible Mechanisms for Formation of Sex Specificities of Cardiospecific Troponins
- Conclusion
- References
| Abstract | ▴Top |
It is well known that the molecules of cardiospecific troponins T and I are localized in the troponin-tropomyosin complex of the cytoplasm of cardiac myocytes and, due to the specific localization, these cardiospecific troponins are widely used as diagnostic biomarkers of myocardial infarction. Cardiospecific troponins are released from the cytoplasm of cardiac myocytes as a result of irreversible cell damage (for example, ischemic necrosis of cardiomyocytes in myocardial infarction or apoptosis of cardiac myocytes in cardiomyopathies and heart failure) or reversible damage (for example, intense physical exertion, hypertension, the influence of stress factors, etc.). Current immunochemical methods for determining cardiospecific troponins T and I have extremely high sensitivity to subclinical (minor) damage to myocardial cells and, thanks to modern high-sensitive methods, it is possible to detect damage to cardiac myocytes in the early (subclinical) stages of a number of cardiovascular pathologies, including myocardial infarction. So, recently, leading cardiological communities (the European Society of Cardiology, the American Heart Association, the American College of Cardiology, etc.) have approved algorithms for early diagnosis of myocardial infarction based on the assessment of serum levels of cardiospecific troponins in the first 1 - 3 h after the onset of pain syndrome. An important factor that may affect early diagnostic algorithms of myocardial infarction are sex-specific features of serum levels of cardiospecific troponins T and I. This manuscript presents a modern view on the role of sex-specific serum levels of cardiospecific troponins T and I in the diagnosis of myocardial infarction and the mechanisms of formation of sex-specific serum levels of troponins.
Keywords: Cardiovascular diseases; Myocardial infarction; Cardiospecific troponins; Cardiac myocytes; Troponin T; Troponin I; Sex-specific levels
| Introduction | ▴Top |
Deaths from non-communicable diseases continue to grow steadily, which indicates the insufficient quality of current clinical strategies (preventive and therapeutic measures) for managing patients with these diseases [1-3]. Thus, according to a recent major study of the global burden of disease (GBD), the largest number of deaths from non-infectious diseases were estimated for cardiovascular diseases (17.8 million (95% confidence interval (CI): 17.5 - 18.0) deaths), followed by neoplasms (9.56 million (95% CI: 9.4 - 9.69) deaths) and chronic respiratory diseases (3.91 million (95% CI: 3.79 - 4.04) deaths. At a global level, total deaths from cardiovascular diseases increased by 21.1% (95% CI: 19.7 - 22.6) between 2007 and 2017. Deaths from coronary heart disease and its main clinical forms, including myocardial infarction, increased from 7.3 (7.22 - 7.46) million deaths to 8.93 (8.79 - 9.14) million deaths between 2007 and 2017 [1]. According to the Russian cardiological communities (Eurasian Association of Cardiologists, Russian Society of Cardiologists), the highest mortality rates of patients from acute coronary syndrome among European countries are recorded in Russia, Ukraine, Belarus, Bulgaria and Lithuania. Among the European countries, the hospital mortality rate ranges from 6% to 14%, while in Russia the mortality rate was 18.6% and 17.7% in 2015 and 2016, respectively [4, 5]. Prevalence of acute coronary syndrome is lower among women than among men. Thus, the proportion of women among patients with acute coronary syndrome, according to the Russian RECORD-3 register for 2015, was 39%. Among patients with myocardial infarction with and without ST elevation, women also constituted a minority of 32% and 44%, respectively [5].
Since chest pain may be the first clinical sign of acute coronary syndrome, its early determination is associated with the improved clinical outcomes. At the same time, quick exclusion of the diagnosis of myocardial infarction can reduce costly hospitalizations and prevent unnecessary, expensive and potentially dangerous procedures [6, 7].
Current Russian (Russian Society of Cardiology) [8, 9] and foreign (European Society of Cardiology, American Heart Association, American College of Cardiology) guidelines [6, 10] recommend the use of cardiospecific troponin tests as the “gold standard” for diagnosing myocardial infarction. This is due to their high cardiospecificity (localization only in cardiac myocytes) [11, 12], diagnostic and prognostic value in forecasting myocardial infarction in case of acute conditions and the risk of all-cause mortality and cardiovascular events in the general population [13, 14].
Due to differences in the prevalence of acute coronary syndrome and in the degree of increase in cardiospecific troponin levels in men and women at the early stages of diagnostics, several authors propose the sex-based approach to the early diagnostics of acute coronary syndrome [15, 16]. However, to date, this approach is not sufficiently covered in a number of guidelines and there are no specific recommendations for the diagnosis of acute coronary syndrome depending on the sex identity. This is largely due to the inconsistency of the results of clinical studies performed in this regard. In addition, the specific physiological mechanisms underlying the formation of sex-based variations in serum levels of cardiospecific troponins have not been established.
This manuscript presents a modern view on the role of sex-specific serum levels of cardiospecific troponins T and I in the diagnosis of myocardial infarction and the mechanisms of formation of sex-specific serum levels of troponins.
| Cardiospecific Troponins: Biochemistry and Physiological Role | ▴Top |
The cardiospecific troponin complex regulates striated muscle contraction and consists of three subunits: troponin C, T, and I, which are designated according to their functional significance. Troponin C (the calcium-binding subunit) binds to calcium ions, which initiates conformational changes in the cardiospecific troponin complex and tropomyosin, leading to the opening of myosin-binding sites on the actin molecule. Subsequently, the myosin head interacts with the myosin-binding sites, resulting in the formation of transverse (actin-myosin) bridges. Troponin T binds to tropomyosin, attaching the cardiospecific troponin complex to the thin (actin) sarcomere filaments. Cardiospecific troponin I binds to actin and reduces the affinity of troponin C for calcium, thereby inhibiting actin-myosin interactions [17, 18].
The most part of the cardiospecific troponins (approximately 90-95%) is associated with myofilaments, and a small concentration (5-10%) is in a free state in the cytosol (Fig. 1). After the loss of membrane integrity of cardiac myocytes, cardiospecific troponin is initially released from the cytosol into the cardiac interstitium and then into the peripheral blood. Troponins T and I are present in cardiac and skeletal muscles and are encoded by different genes in each muscle type, resulting in two immunochemical different products. Laboratory diagnostic studies are based on the use of high-affinity antibodies that are specific for cardiospecific troponin T and cardiospecific troponin I, and not for troponin C, since it is identical in both muscles [18-20].
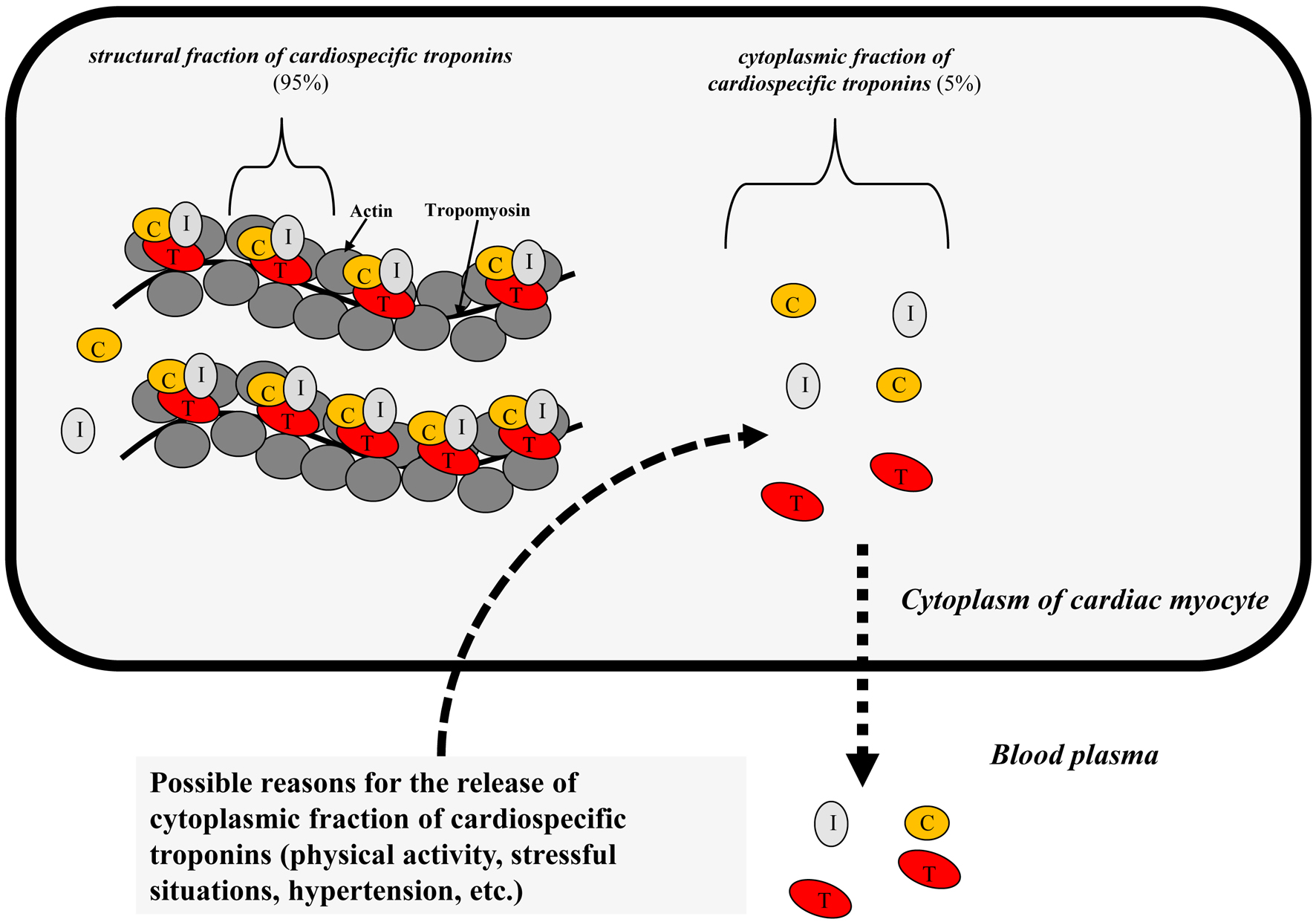 Click for large image | Figure 1. Distribution of cardiospecific troponins in the cytoplasm of cardiac myocytes. |
| High-Sensitive Cardiospecific Troponins: Characteristics of Detection Methods and Important Analytical Parameters | ▴Top |
Since Katus et al described the first test to measure cardiospecific troponin in 1991 [21], an extremely long journey has been made from the development to the introduction of high-sensitive troponin tests into clinical practice and the emergency care department [22, 23].
The use of high-sensitive cardiospecific troponin laboratory diagnostic tests is an important step forward due to their high sensitivity to cardiac myocytes necrosis, as they are able to determine cardiospecific troponin concentrations approximately 10 - 100 times lower than conventional tests, leading to more accurate and timely diagnostics [24, 25].
According to the International Federation of Clinical Chemistry (IFCC) guidelines, two criteria are used to define this new generation of (high-sensitive) cardiospecific troponin tests: 1) the coefficient of variation at the 99th percentile value should be 10% or less (the most optimal immunoassays), although tests with the error of more than 10% and 20% or less are still considered clinically acceptable; 2) the concentration of cardiospecific troponins should be above the minimum determinable concentration (limit of detection (LoD)) in more than 50% of healthy individuals [22, 26, 27].
New laboratory diagnostic tests allow to conduct earlier diagnostics and to quickly exclude myocardial infarction due to high sensitivity [28]; however, the second key immunoassay criterion, specificity, is affected significantly. Clinically, this is expressed by the presence of a wide range of other troponin-positive non-cardiac and cardiac conditions other than myocardial infarction [29, 30]. Although not all mechanisms of elevation of cardiospecific troponin levels are known, in some conditions, this may be due to a decrease in oxygen supply to the myocardium, and it is not clear whether the damage is always irreversible, which inevitably leads to cardiac myocytes necrosis, or whether some diseases can cause reversible damage [31-34]. The main conditions (physiological and pathological) that cause an increase in the levels of cardiospecific troponins are shown in Table 1 [29-34].
 Click to view | Table 1. Main Causes of Cardiac Myocytes Damage (Physiological and Pathological) and Increased Concentration of Cardiospecific Troponins [29-34] |
Currently, all available high-sensitive methods for determining cardiospecific troponins have a single diagnostic threshold value for acute coronary syndrome diagnostics, based on the value of the 99th percentile, which is calculated for a healthy population [27, 35]. However, this threshold value can vary significantly depending on the methodology for determining (manufacturer) cardiospecific troponins [35, 36]. According to the IFCC, the main manufacturers of high-sensitive immunochemical reagent kits for determining cardiospecific troponins are: Abbot (USA), Beckman Coulter (USA), bioMerieux (France), ET Healthcare (China), LSI Medience (Japan), Fujirebio (Japan), Ortho Clinical Diagnostics (USA), Quidel/Alere (USA), Roche (Switzerland), Siemens (Germany), etc. (Table 2 [35]).
 Click to view | Table 2. Main Analytical Characteristics, Including Sex Specifications, of Modern High-Sensitive Cardiospecific Troponin Immunotests [35] |
The additional important diagnostic advantage of high-sensitive tests for immunochemical determination of cardiospecific troponins is the ability to determine cardiac myocytes damage at the subclinical level, which can be used to monitor and assess the prognosis of patients suffering from a number of chronic pathologies, including coronary heart disease [37], during the treatment of oncological diseases by using chemotherapeutic compounds, which are characterized by cardiotoxicity [38-40], as well as chronic obstructive pulmonary disease [41, 42], chronic kidney disease [43, 44], diabetes mellitus [45], arterial hypertension [46], etc.
An important advantage of modern high-sensitive cardiospecific troponin immunotests is the ability to detect cardiospecific troponin molecules in noninvasively obtained biological material (oral fluid, urine, sweat) [47-51]. When receiving these biomaterials, a number of advantages can be noted: non-invasiveness, atraumatic, painless, no specially trained medical personnel is required, the ability to conduct preliminary diagnostics at home (test strips). Therefore, this method will allow for the diagnosis of diseases in a non-invasive way. However, to date, this is a little-studied and controversial area that requires further research to confirm these possibilities [52, 53].
| Sex Specificities of Cardiospecific Troponin Levels | ▴Top |
Sex specificities of levels are characteristic of a number of laboratory analytes (red blood cell (RBC) count, hemoglobin, creatinine levels, etc.), which is widely used in modern clinical practice. As for cardiac markers, for the first time information about the sex specificities of laboratory tests was found during the study of creatine phosphokinase activity, the test for determining which was used to diagnose myocardial infarction in the 60-70s of the 20th century. Healthy men had significantly higher creatine phosphokinase activity than women, and dark-skinned people had higher creatine phosphokinase activity than Caucasians [54]. This was also characteristic of the MB-fraction of creatine phosphokinase, both for activity (U/L) and for the concentration of creatine phosphokinase-MB (creatine phosphokinase-MB mass), measured in ng/mL. The mechanism of these differences, according to academic specialists, was largely due to the differences in skeletal muscle mass in men compared to women [54]. Later, sex differences were noted for natriuretic peptides, and, according to the authors, they were due to the different influence of male and female sex hormones on the production of natriuretic peptides in the myocardium [55]. However, with the introduction of the first tests for immunochemical determination of cardiospecific troponins, sex features ceased to be determined, which was probably due to the low sensitivity of these test systems, because they determined troponin concentrations in only 5% of healthy subjects [24-26]. Therefore, at that time, the prevailing opinion was that cardiospecific troponins are strictly intracellular molecules that appear in the blood serum only in case of serious pathologies of the myocardium, and certain positive levels of cardiospecific troponins in patients with unconfirmed myocardial infarction were most often interpreted as false positive results. This opinion was also supported by the studies reporting a high prevalence of false positive results of cardiospecific troponins in patients with rhabdomyolysis in case of skeletal muscle pathologies [56, 57]. As the sensitivity of laboratory methods increased, cardiospecific troponin levels began to be determined in the blood of a larger number of healthy individuals (which allowed to regard cardiospecific troponin as the metabolic products of cardiac myocytes) and the first reports of possible sex-based variations in cardiospecific troponin levels appeared. Thus, Apple et al, studying the reference limits of cardiospecific troponin levels in a large sample of patients (n = 686) using eight immunochemical determination tests, found the presence of sex variations in two methods of immunochemical determination of cardiospecific troponin I. At the same time, the average level of cardiospecific troponin I in men was 1.2 - 2.5 times higher than in women, according to the nonparametric statistical analysis of the results [58]. However, this study is actually the only one that reported any sex variations for the moderately sensitive research methods, and therefore this was not reflected in practical medicine. With the introduction of high-sensitive immunochemical tests, it has been shown that in 80% of healthy individuals, determinable cardiospecific troponin concentrations exceed the determination limit [59], and the rates are significantly higher in men than in women, leading to a more detailed study of the potential sex-specific 99th percentile. In a large study including 524 healthy subjects (272 males, 252 females), 99th percentile levels were calculated for 19 cardiospecific troponin tests: one cardiospecific troponin T test by Roche and 18 cardiospecific troponin I tests by Abbott, Alere, Beckman, bioMerieux, Instrumentation Laboratory, Ortho-Clinical Diagnostics, Singulex, Siemens and Roche, of which five were analytically classified as high-sensitive. The study found that 99th percentile levels exceeded the determination limit in 80% of people in case of high-sensitive immunochemical determination tests, while moderately sensitive tests determined measurable cardiospecific troponin levels in about 25% to 30% of patients. Sex specificities of the 99th percentile were typical of all high-sensitive test systems for determining cardiospecific troponin I, the values of which in men were 1.2 - 2.4 times higher than in women. Approximately similar values were demonstrated by the high-sensitive analysis for cardiospecific troponin T: the 99th percentile for men was 20 ng/L, and for women it was 13 ng/L, while the overall (regardless of sex) calculated 99th percentile was 15 ng/L. Besides, the sex-specific 99th percentile was characteristic of some moderately sensitive test systems, according to which cardiospecific troponin levels were 1.3 - 5 times higher in men than in women [59].
Saenger et al [60] showed that statistically significant differences were observed in high-sensitivity cardiospecific troponin T concentrations in men and women, with the 99th percentile limit for men (15.5 ng/L) approximately 1.7 times higher than for women (9.0 ng/L).
In another large study, Gore et al reported similar results of the three large independent patient cohorts in which high-sensitive cardiospecific troponin T concentrations were analyzed based on the age, sex, and race stratification. It is important to note that more than 10% of men aged 65 to 74 years without cardiovascular disease had high-sensitivity cardiospecific troponin T values above the threshold value (99th percentile) (> 14 ng/L). In each cohort studied, the value of the 99th percentile increased with age over 60 and was higher in men than in women. The academic specialists also found significant differences in the threshold levels of high-sensitive cardiospecific troponin T depending on age and sex specificities: men (disregarding age) = 23 ng/L, men 50 - 64 years old = 28 ng/mL, men under 50 years old = 19 ng/L; women (disregarding age) = 9 ng/mL, women 50 - 64 years old = 14 ng/mL, women under 50 years old = 9 ng/mL [61]. Thus, sex and age must be taken into account when calculating the 99th percentile levels of high-sensitive cardiospecific troponins. Whereas the use of the single threshold value (14 ng/L) for high-sensitive cardiospecific troponin T analysis can lead to overdiagnosis of myocardial infarction, especially in men and the elderly, since their normal (baseline) level significantly exceeds the 99th percentile recommended by the immunotests manufacturer. The studies presented are indicative of the need for a close study of the sex-age specificities of cardiospecific troponins for clinical validation.
In the current European Society of Cardiology guidelines for the diagnostics and treatment of myocardial infarction without ST-segment elevation [62], the diagnosis of myocardial infarction is based not on the single value of the cardiospecific troponin, but on two main algorithms based on the dynamic changes in cTn at the 0 moment (on admission to the emergency care department and first blood test) and after 3 h or after 1 h. Only validated, high-sensitive cardiospecific troponin immunotests with confirmed threshold levels or cutoff values should be used to apply these algorithms. Notably, the 0/3 h algorithm makes a clear reference to the upper control limit of the 99th percentile, and this is also specified in the fourth universal definition of myocardial infarction [10], while the 0/1 h algorithm uses cutoffs below the 99th percentile, calculated for specific cardiospecific troponin tests of immunochemical determination. The most important role in these diagnostic algorithms is played by the kinetics of the increase in cardiospecific troponin levels during the first hours from the moment of chest pain/admission to the emergency care department. The positive predictive value of these algorithms for patients with myocardial infarction, i.e., those who meet the “rule-in” criteria, is 75-80%. Some patients that meet the “rule-in” criterion with diagnoses other than myocardial infarction may have conditions (e.g., takotsubo cardiomyopathy, myocarditis, etc.) that usually require hospitalization and coronary angiography for accurate diagnosis [62]. As the upper control limit of the 99th percentile is not always sex-specific, and the 0/1 h algorithm does not use sex-based cutoffs, the absence of specificity and relatively low positive predictive value of cardiospecific troponins in patients with myocardial infarction may be partly explained by the inadequate threshold value, which is equal for both men and women.
There is ongoing debate regarding the appropriateness of using the sex-specific 99th percentile as the diagnostic threshold [26, 62-66]. Its use can lead to an excess of patients with the elevated cardiospecific troponins level which is not associated with myocardial infarction [63, 64]. On the other hand, the use of common cutoffs may lead to underestimation of myocardial infarction, especially in women [65, 66]. Novack et al [67] showed that women form a high-risk group which receives less of the treatment methods for myocardial infarction recommended by the guidelines, including less frequent cardiac catheterization and use of secondary prevention methods. That is why determination of the threshold level of cardiospecific troponin in women is critical, since an incorrect decision limit can lead to incorrect interpretation of the result and further management of these patients.
In a retrospective study by Trambas et al [68], switching from a moderately sensitive method for determination cardiospecific troponin I to a high-sensitive cardiospecific troponin I test significantly increased the number of patients with elevated cardiospecific troponin I concentrations, while no statistically significant changes were found in men. Introduction of sex-specific threshold reference values did not lead to an increase in the number of cases of myocardial infarction among the female population. On the other hand, the introduction of sex-specific reference intervals has identified those women who are at increased risk of future cardiovascular events. Similar results were demonstrated in case of use of high-sensitivity cardiospecific troponin T in the study (study of bypass angiopasty revascularization in case of type 2 diabetes) [69]. Within this study they observed 684 women and 1,601 men with type 2 diabetes mellitus and stable coronary artery disease for 5 years. The results showed that among patients with type 2 diabetes mellitus and stable coronary artery disease, women with circulating levels of high-sensitivity cardiospecific troponin T that are within the “normal” range (the commonly used 99th percentile disregarding sex) are at increased risk of serious cardiovascular events, which exceeds the rates observed among men with similar concentrations of high-sensitive cardiospecific troponin T [69]. Thus, this study also shows the need to revise the 99th percentile with account taken of the sex.
| Possible Mechanisms for Formation of Sex Specificities of Cardiospecific Troponins | ▴Top |
Under physiological conditions, the most common causes of elevated cardiospecific troponins are physical activity and psychoemotional stress [70-72]. These physiological conditions can lead to myocardial overload, small-scale processes of cardiac myocytes apoptosis due to increased activity of the sympathoadrenal system, increased activity of prooxidant mechanisms, reversible damage to cardiac myocyte membranes, which is accompanied by the release of cytosolic cardiospecific troponin molecules, and a slight increase in serum concentrations of cardiospecific troponins [73-75]. Thus, elevated levels of cardiospecific troponins in healthy individuals may reflect the response of cardiac myocytes to the influence of stress factors. However, in men and women, the activity of protective mechanisms of different cells, including the cardiac myocytes, against stress factors differs, which may be a possible explanation for sex differences in serum levels of cardiospecific troponins. Thus, the recent study [76] demonstrated that the levels of cardiospecific troponin T after the same physical activity in male athletes were significantly higher than in female athletes, which is indicative of the different response of cardiac myocytes to physical activity in men and women.
In addition to this, the study by Tiller et al also showed more pronounced disorders of physiology of the cardiovascular system in men than in women after an ultramarathon [77]. Potentially, these negative effects could lead to a greater release of cardiospecific troponins in men than in women.
The fact that men are less protected from myocardial injury was also demonstrated by the study which observed that, after heart surgery, men had a greater increase in blood serum cardiospecific troponin levels than women [78].
That said, the groups of men and women were formed in accordance with the same characteristics (same body mass index, duration of artificial circulation, duration of aortic compression during surgery, etc.), which could potentially affect the degree of myocardial damage and the release of cardiospecific troponins. Thus, variations in damage and release of cardiospecific troponins, apparently, are due to the sex-based differences in the degree of ischemia-reperfusion injury of cardiac myocytes.
Sex differences in the degree of cardiac myocytes damage can be explained by sex specificities in the levels of a number of biologically active molecules, and in particular sex steroids. Thus, in women, estrogen levels are significantly higher than in men, in whom the predominant steroid is testosterone. That said, estrogens, unlike testosterone, are characterized by numerous cardioprotective effects. Thus, it has been shown that estrogens can have a protective effect against oxidative damage to cardiac myocytes by reducing the oxidative damage and stimulating the expression of antioxidant enzymes [79, 80]. In addition, estrogens increase the expression of endothelial nitric oxide synthase, which leads to an increase in the formation of one of the most powerful vasodilators - nitric oxide, and this, in its turn, contributes to greater resistance of the cardiovascular system to coronary vessel spasms (and, accordingly, to a decrease in myocardial blood content), occurring against the background of psycho-emotional stress. Since estrogen production decreases with age in women, cardioprotective effects also decrease, which is expressed by higher levels of cardiospecific troponins in elderly women [61], as reported above in the previous section. Thus, the cardioprotective effects of estrogens can neutralize the degree of damage to cardiac myocytes both under physiological conditions (under stress conditions) and in case of pathological conditions.
Metabolism and renewal of cardiac myocytes [17, 81-83], which is responsible for the formation of basic serum levels of cardiospecific troponins is regarded as another physiological mechanism for the release of cardiospecific troponins. Taking into account the fact that cardiac myocytes hypertrophy is associated with cardiospecific troponin levels in healthy individuals [13, 84], and in men the myocardial mass (physiological hypertrophy) is bigger than in women [61, 66], the metabolism and renewal of cardiac myocytes can also be considered as a possible mechanism that explains the sex-based variations in the serum levels of cardiospecific troponins. Besides, this mechanism can also explain the sex-based differences in creatine phosphokinase and creatine phosphokinase-MB levels demonstrated in clinical studies [85-87].
| Conclusion | ▴Top |
Thus, introduction of high-sensitive immunochemical tests for determining cardiospecific troponins into clinical practice requires consideration of a number of biological factors of individuals, including sex and age-related characteristics. The optimal level of the 99th percentile is of great importance for the timely diagnostics of acute coronary syndrome and at the same time prevents overdiagnosis of myocardial infarction. Thus, a number of studies have shown that the use of the common 99th percentile can lead to underdiagnosis of acute coronary syndrome in women, since their physiological levels of cardiospecific troponins are much lower. At the same time, the use of the 99th percentile without taking into account the sex factor leads to overdiagnosis of acute coronary syndrome in men, which is due to higher physiological levels of cardiospecific troponins in the blood. According to the IFCC, sex specificities of the 99th percentile are characteristic of most of the existing high-sensitive cardiospecific troponin laboratory tests. Possible mechanisms underlying the sex-based variations in cardiospecific troponin levels are the effects of sex hormones and differences in the myocardial mass. Thus, estrogens have cardioprotective effects, due to which they cause expansion of the coronary vessels, which increases the resistance of cardiac myocytes to physical activities and stressful situations. In addition to the above, estrogens reduce oxidative stress, and thanks to this the damage to cardiac myocytes membranes is limited and the apoptotic mechanisms are suppressed. Apparently, the complex cardioprotective effects of estrogens limit the release of cytoplasmic cardiospecific troponin molecules from the cardiac myocytes into the bloodstream. Further research is needed on the sex specificities of cardiospecific troponin levels: both of clinical (to clarify their significance in the algorithms for diagnosing the acute coronary syndrome) and fundamental nature (to clarify the molecular mechanisms underlying the sex-based variations in the “serum” cardiospecific troponin levels).
Acknowledgments
None to declare.
Financial Disclosure
This research received no external funding.
Conflict of Interest
The author declares no conflict of interest.
Data Availability
The author declares that data supporting the findings of this study are available within the article.
Abbreviations
IFCC: International Federation of Clinical Chemistry; LoD: limit of detection; CV: coefficient of variation; M: men; W: women; EDTA: ethylenediaminetetraacetate
| References | ▴Top |
- Collaborators GBDCoD. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392(10159):1736-1788.
doi pubmed - Chaulin AM, Duplyakov DV. Environmental factors and cardiovascular diseases. Hygiene and Sanitation. 2021;100(3):223-228. (In Russ).
doi - Chaulin AM, Sergeev AK. The role of fine particles (PM 2.5) in the genesis of atherosclerosis and myocardial damage: emphasis on clinical and epidemiological data, and pathophysiological mechanisms. Cardiol Res. 2022;13(5):268-282.
doi pubmed - Staroverov II, Shakhnovich RM, Gilyarov MYu, et al. Eurasian clinical guidelines on diagnosis and treatment of acute coronary syndrome with ST segment elevation (STEMI). Eurasian Heart Journal. 2020;(1):4-77. (In Russ).
doi - Erlikh AD, Gratsiansky On Behalf Of Record-Participants NA. [Registry of acute coronary syndromes RECORD-3. Characteristics of patients and treatment during initial hospitalization]. Kardiologiia. 2016;56(4):16-24.
doi pubmed - Collet JP, Thiele H, Barbato E, Barthelemy O, Bauersachs J, Bhatt DL, Dendale P, et al. 2020 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. Eur Heart J. 2021;42(14):1289-1367.
doi pubmed - Chaulin AM, Grigorieva YuV, Pavlova TV, Duplyakov DV. Diagnostic significance of complete blood count in cardiovascular patients. Russian Journal of Cardiology. 2020;25(12):3923.
doi - Clinical practice guidelines for Acute ST-segment elevation myocardial infarction. Russian Journal of Cardiology. 2020;25(11):4103. (In Russ).
doi - Barbarash OL, Duplyakov DV, Zateischikov DA, et al. 2020 Clinical practice guidelines for Acute coronary syndrome without ST segment elevation. Russian Journal of Cardiology. 2021;26(4):4449. (In Russ).
doi - Thygesen K, Alpert JS, Jaffe AS, Chaitman BR, Bax JJ, Morrow DA, White HD, et al. Fourth universal definition of myocardial infarction (2018). Circulation. 2018;138(20):e618-e651.
doi pubmed - Chaulin AM. Cardiac troponins metabolism: from biochemical mechanisms to clinical practice (Literature Review). Int J Mol Sci. 2021;22(20):10928.
doi pubmed - Chaulin A. Cardiac Troponins: Contemporary Biological Data and New Methods of Determination. Vasc Health Risk Manag. 2021;17:299-316.
doi pubmed - de Lemos JA, Drazner MH, Omland T, Ayers CR, Khera A, Rohatgi A, Hashim I, et al. Association of troponin T detected with a highly sensitive assay and cardiac structure and mortality risk in the general population. JAMA. 2010;304(22):2503-2512.
doi pubmed - Zeller T, Tunstall-Pedoe H, Saarela O, Ojeda F, Schnabel RB, Tuovinen T, Woodward M, et al. High population prevalence of cardiac troponin I measured by a high-sensitivity assay and cardiovascular risk estimation: the MORGAM Biomarker Project Scottish Cohort. Eur Heart J. 2014;35(5):271-281.
doi pubmed - Lobo R, De Michieli L, Jaffe AS. Sex-specific 99th percentile URLs for cardiac troponin assays-their time has come. Clin Chem. 2021;67(1):197-200.
doi pubmed - Peacock WF, Baumann BM, Rivers EJ, Davis TE, Handy B, Jones CW, Hollander JE, et al. Using sex-specific cutoffs for high-sensitivity cardiac troponin T to diagnose acute myocardial infarction. Acad Emerg Med. 2021;28(4):463-466.
doi pubmed - Chaulin AM, Duplyakov DV. Analytical review of modern information on the physiological and pathochemical mechanisms of the release of cardiospecific proteins from muscle tissue, methodology and technologies of their research, interpretation of the results. Laboratory Diagnostics. Eastern Europe. 2022;11(1):78-97. (In Russian).
doi - Conrad MJ, Jarolim P. Cardiac troponins and high-sensitivity cardiac troponin assays. Clin Lab Med. 2014;34(1):59-73.
doi pubmed - Xu RY, Zhu XF, Yang Y, Ye P. High-sensitive cardiac troponin T. J Geriatr Cardiol. 2013;10(1):102-109.
- Chaulin AM. Cardiac troponins: current information on the main analytical characteristics of determination methods and new diagnostic possibilities. Medwave. 2021;21(11):e8498.
doi pubmed - Katus HA, Remppis A, Neumann FJ, Scheffold T, Diederich KW, Vinar G, Noe A, et al. Diagnostic efficiency of troponin T measurements in acute myocardial infarction. Circulation. 1991;83(3):902-912.
doi pubmed - Chaulin AM, Abashina OE, Duplyakov DV. High-sensitivity cardiac troponins: detection and central analytical characteristics. Cardiovascular Therapy and Prevention. 2021;20(2):2590. (In Russ).
doi - Galvani M, Bachetti C. High-sensitivity troponin in emergency room practice: pros and cons. J Cardiovasc Med (Hagerstown). 2018;19(Suppl 1):e68-e71.
doi pubmed - Jaffe AS. The 10 commandments of troponin, with special reference to high sensitivity assays. Heart. 2011;97(11):940-946.
doi pubmed - Chaulin AM, Karslyan LS, Bazyuk EV, Nurbaltaeva DA, Duplyakov DV. [Clinical and Diagnostic Value of Cardiac Markers in Human Biological Fluids]. Kardiologiia. 2019;59(11):66-75.
doi pubmed - Apple FS, Collinson PO, Biomarkers ITFoCAoC. Analytical characteristics of high-sensitivity cardiac troponin assays. Clin Chem. 2012;58(1):54-61.
doi pubmed - Apple FS, Jaffe AS, Collinson P, Mockel M, Ordonez-Llanos J, Lindahl B, Hollander J, et al. IFCC educational materials on selected analytical and clinical applications of high sensitivity cardiac troponin assays. Clin Biochem. 2015;48(4-5):201-203.
doi pubmed - Reichlin T, Hochholzer W, Bassetti S, Steuer S, Stelzig C, Hartwiger S, Biedert S, et al. Early diagnosis of myocardial infarction with sensitive cardiac troponin assays. N Engl J Med. 2009;361(9):858-867.
doi pubmed - Chaulin AM. Elevation mechanisms and diagnostic consideration of cardiac troponins under conditions not associated with myocardial infarction. Part 1. Life (Basel). 2021;11(9):914.
doi pubmed - Chaulin AM. Elevation mechanisms and diagnostic consideration of cardiac troponins under conditions not associated with myocardial infarction. Part 2. Life (Basel). 2021;11(11):1175.
doi pubmed - Park KC, Gaze DC, Collinson PO, Marber MS. Cardiac troponins: from myocardial infarction to chronic disease. Cardiovasc Res. 2017;113(14):1708-1718.
doi pubmed - Chaulin AM. Hypertension as one of the main non-myocardial infarction-related causes of increased cardiospecific troponins: from mechanisms to significance in current medical practice. J Clin Med Res. 2022;14(11):448-457.
doi pubmed - Masri W, Le Guillou E, Hamdi E, Ghazal K, Lebigot E, Cosson C, Cynober FB, et al. Troponin elevation in other conditions than acute coronary syndromes. Ann Biol Clin (Paris). 2017;75(4):411-419.
doi pubmed - Chaulin A, Duplyakov D. The main causes and mechanisms of the formation of false positive results of troponin immunotests. Laboratory Diagnostics Eastern Europe. 2022;11:132-147.
doi - URL: https://www.ifcc.org/media/478962/high-sensitivity-cardiac-troponin-i-and-t-assay-analytical-characteristics-designated-by-manufacturer-v042021.pdf.
- Chaulin AM, Duplyakov DV. Cardiac troponins: Current data on the diagnostic value and analytical characteristics of new determination methods. Cor Vasa. 2021;63:486-493.
doi - Mohebi R, Jackson L, McCarthy CP, Murtagh G, Murphy SP, Abboud A, Miksenas H, et al. Relation of high-sensitivity cardiac troponin I and obstructive coronary artery disease in patients without acute myocardial infarction. Am J Cardiol. 2022;173:16-24.
doi pubmed - Chaulin AM, Duplyakov DV. Arrhythmogenic effects of doxorubicin. Complex Issues of Cardiovascular Diseases. 2020;9(3):69-80. (In Russ).
doi - Chaulin AM. Review of recent laboratory and experimental data on cardiotoxicity of statins. J Cardiovasc Dev Dis. 2022;9(11):403.
doi pubmed - Chaulin AM, Abashina OE, Duplyakov DV. Pathophysiological mechanisms of cardiotoxicity in chemotherapeutic agents. Russ Open Med J. 2020;9(3):e0305.
doi - Mk A, Gn N. Cardiac troponin I in acute exacerbation of chronic obstructive pulmonary disease. J Assoc Physicians India. 2022;70(4):11-12.
- Chaulin AM, Duplyakov DV. Comorbidity in chronic obstructive pulmonary disease and cardiovascular disease. Cardiovascular Therapy and Prevention. 2021;20(3):2539. (In Russ).
doi - Hti Lar Seng NS, Zeratsion G, Pena O, Tufail MU, Jim B. Utility of cardiac troponins in patients with chronic kidney disease. Cardiol Rev. 2022.
doi pubmed - Chaulin AM. Biology of Cardiac Troponins: Emphasis on Metabolism. Biology (Basel). 2022;11(3):429.
doi pubmed - Bellia C, Lombardo M, Della-Morte D. Use of Troponin as a predictor for cardiovascular diseases in patients with type 2 Diabetes Mellitus. Clin Chim Acta. 2020;507:54-61.
doi pubmed - Chaulin A. Clinical and diagnostic value of highly sensitive cardiac troponins in arterial hypertension. Vasc Health Risk Manag. 2021;17:431-443.
doi pubmed - Foley JD, 3rd, Sneed JD, Steinhubl SR, Kolasa J, Ebersole JL, Lin Y, Kryscio RJ, et al. Oral fluids that detect cardiovascular disease biomarkers. Oral Surg Oral Med Oral Pathol Oral Radiol. 2012;114(2):207-214.
doi pubmed - Mirzaii-Dizgah I, Riahi E. Salivary troponin I as an indicator of myocardial infarction. Indian J Med Res. 2013;138(6):861-865.
- Chaulin AM, Duplyakova PD, Bikbaeva GR, Tukhbatova AA, Grigorieva EV, Duplyakov DV. Concentration of high-sensitivity cardiac troponin I in the oral fluid in patients with acute myocardial infarction: a pilot study. Russian Journal of Cardiology. 2020;25(12):3814.
doi - Chen JY, Lee SY, Li YH, Lin CY, Shieh MD, Ciou DS. Urine high-sensitivity troponin I predict incident cardiovascular events in patients with diabetes mellitus. J Clin Med. 2020;9(12):3917.
doi pubmed - Chaulin AM. Diagnostic value of highly sensitive cardiac troponins and mechanisms of their increase in serum and urine in arterial hypertension. Riv Ital Med Lab. 2021;17:99-107.
doi - Bahbah EI, Noehammer C, Pulverer W, Jung M, Weinhaeusel A. Salivary biomarkers in cardiovascular disease: An insight into the current evidence. FEBS J. 2021;288(22):6392-6405.
doi pubmed - Chaulin AM. The Importance of Cardiac Troponin Metabolism in the Laboratory Diagnosis of Myocardial Infarction (Comprehensive Review). Biomed Res Int. 2022;2022:6454467.
doi pubmed - Apple FS, Jaffe AS. Men are different than women: it's true for cardiac troponin too. Clin Biochem. 2014;47(10-11):867-868.
doi pubmed - Apple FS, Panteghini M, Ravkilde J, Mair J, Wu AH, Tate J, Pagani F, et al. Quality specifications for B-type natriuretic peptide assays. Clin Chem. 2005;51(3):486-493.
doi pubmed - Punukollu G, Gowda RM, Khan IA, Mehta NJ, Navarro V, Vasavada BC, Sacchi TJ. Elevated serum cardiac troponin I in rhabdomyolysis. Int J Cardiol. 2004;96(1):35-40.
doi pubmed - Li SF, Zapata J, Tillem E. The prevalence of false-positive cardiac troponin I in ED patients with rhabdomyolysis. Am J Emerg Med. 2005;23(7):860-863.
doi pubmed - Apple FS, Quist HE, Doyle PJ, Otto AP, Murakami MM. Plasma 99th percentile reference limits for cardiac troponin and creatine kinase MB mass for use with European Society of Cardiology/American College of Cardiology consensus recommendations. Clin Chem. 2003;49(8):1331-1336.
doi pubmed - Apple FS, Ler R, Murakami MM. Determination of 19 cardiac troponin I and T assay 99th percentile values from a common presumably healthy population. Clin Chem. 2012;58(11):1574-1581.
doi pubmed - Saenger AK, Beyrau R, Braun S, Cooray R, Dolci A, Freidank H, Giannitsis E, et al. Multicenter analytical evaluation of a high-sensitivity troponin T assay. Clin Chim Acta. 2011;412(9-10):748-754.
doi pubmed - Gore MO, Seliger SL, Defilippi CR, Nambi V, Christenson RH, Hashim IA, Hoogeveen RC, et al. Age- and sex-dependent upper reference limits for the high-sensitivity cardiac troponin T assay. J Am Coll Cardiol. 2014;63(14):1441-1448.
doi pubmed - Roffi M, Patrono C, Collet JP, Mueller C, Valgimigli M, Andreotti F, Bax JJ, et al. 2015 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: Task Force for the Management of Acute Coronary Syndromes in Patients Presenting without Persistent ST-Segment Elevation of the European Society of Cardiology (ESC). Eur Heart J. 2016;37(3):267-315.
doi pubmed - Mueller-Hennessen M, Lindahl B, Giannitsis E, Biener M, Vafaie M, deFilippi CR, Christ M, et al. Diagnostic and prognostic implications using age- and gender-specific cut-offs for high-sensitivity cardiac troponin T - Sub-analysis from the TRAPID-AMI study. Int J Cardiol. 2016;209:26-33.
doi pubmed - Rubini Gimenez M, Twerenbold R, Boeddinghaus J, Nestelberger T, Puelacher C, Hillinger P, Wildi K, et al. Clinical effect of sex-specific cutoff values of high-sensitivity cardiac troponin T in suspected myocardial infarction. JAMA Cardiol. 2016;1(8):912-920.
doi pubmed - McRae A, Graham M, Abedin T, Ji Y, Yang H, Wang D, Southern D, et al. Sex-specific, high-sensitivity cardiac troponin T cut-off concentrations for ruling out acute myocardial infarction with a single measurement. CJEM. 2019;21(1):26-33.
doi pubmed - Shah AS, Griffiths M, Lee KK, McAllister DA, Hunter AL, Ferry AV, Cruikshank A, et al. High sensitivity cardiac troponin and the under-diagnosis of myocardial infarction in women: prospective cohort study. BMJ. 2015;350:g7873.
doi pubmed - Novack V, Cutlip DE, Jotkowitz A, Lieberman N, Porath A. Reduction in sex-based mortality difference with implementation of new cardiology guidelines. Am J Med. 2008;121(7):597-603.e591.
doi pubmed - Trambas C, Pickering JW, Than M, Bain C, Nie L, Paul E, Dart A, et al. Impact of high-sensitivity troponin i testing with sex-specific cutoffs on the diagnosis of acute myocardial infarction. Clin Chem. 2016;62(6):831-838.
doi pubmed - Everett BM, Brooks MM, Vlachos HE, Chaitman BR, Frye RL, Bhatt DL, BARI 2D Study Group. Sex differences in cardiac troponin and the risk of death or major cardiovascular events. J Am Coll Cardiol. 2016;68(9):978-980.
doi pubmed - Lazzarino AI, Hamer M, Gaze D, Collinson P, Steptoe A. The association between cortisol response to mental stress and high-sensitivity cardiac troponin T plasma concentration in healthy adults. J Am Coll Cardiol. 2013;62(18):1694-1701.
doi pubmed - Aengevaeren VL, Baggish AL, Chung EH, George K, Kleiven O, Mingels AMA, Orn S, et al. Exercise-induced cardiac troponin elevations: from underlying mechanisms to clinical relevance. Circulation. 2021;144(24):1955-1972.
doi pubmed - Chaulin AM, Duplyakova PD, Duplyakov DV. Circadian rhythms of cardiac troponins: mechanisms and clinical significance. Russian Journal of Cardiology. 2020;25(3S):4061.
doi - Jan MI, Khan RA, Fozia, Ahmad I, Khan N, Urooj K, Shah A, et al. C-reactive protein and high-sensitive cardiac troponins correlate with oxidative stress in valvular heart disease patients. Oxid Med Cell Longev. 2022;2022:5029853.
doi pubmed - Chaulin AM. Phosphorylation and fragmentation of the cardiac troponin T: mechanisms, role in pathophysiology and laboratory diagnosis. Int J Biomed. 2021;11:250-259.
doi - Chaulin AM, Duplyakov DV. Arrhythmogenic effects of doxorubicin. Complex Issues of Cardiovascular Diseases. 2020;9(3):69-80. (In Russ).
doi - Kong Z, Nie J, Lin H, George K, Zhao G, Zhang H, Tong TK, et al. Sex differences in release of cardiac troponin T after endurance exercise. Biomarkers. 2017;22(3-4):345-350.
doi pubmed - Tiller NB, Wheatley-Guy CM, Fermoyle CC, Robach P, Ziegler B, Gavet A, Schwartz JC, et al. Sex-specific physiological responses to ultramarathon. Med Sci Sports Exerc. 2022;54(10):1647-1656.
doi pubmed - Schwarzenberger JC, Sun LS, Pesce MA, Heyer EJ, Delphin E, Almeida GM, Wood M. Sex-based differences in serum cardiac troponin I, a specific marker for myocardial injury, after cardiac surgery. Crit Care Med. 2003;31(3):689-693.
doi pubmed - Mendelsohn ME, Karas RH. The protective effects of estrogen on the cardiovascular system. N Engl J Med. 1999;340(23):1801-1811.
doi pubmed - Stearns JD, Davila-Roman VG, Barzilai B, Thompson RE, Grogan KL, Thomas B, Hogue CW, Jr. Prognostic value of troponin I levels for predicting adverse cardiovascular outcomes in postmenopausal women undergoing cardiac surgery. Anesth Analg. 2009;108(3):719-726.
doi pubmed - Bergmann O, Bhardwaj RD, Bernard S, Zdunek S, Barnabe-Heider F, Walsh S, Zupicich J, et al. Evidence for cardiomyocyte renewal in humans. Science. 2009;324(5923):98-102.
doi pubmed - White HD. Pathobiology of troponin elevations: do elevations occur with myocardial ischemia as well as necrosis? J Am Coll Cardiol. 2011;57(24):2406-2408.
doi pubmed - Chaulin AM. [Main analytical characteristics of laboratory methods for the determination of cardiac troponins: a review from the historical and modern points of view]. Orv Hetil. 2022;163(1):12-20.
doi pubmed - Ucar H, Gur M, Kivrak A, Koyunsever NY, Seker T, Akilli RE, Turkoglu C, et al. High-sensitivity cardiac troponin T levels in newly diagnosed hypertensive patients with different left ventricle geometry. Blood Press. 2014;23(4):240-247.
doi pubmed - Neal RC, Ferdinand KC, Ycas J, Miller E. Relationship of ethnic origin, gender, and age to blood creatine kinase levels. Am J Med. 2009;122(1):73-78.
doi pubmed - Clifford SM, Bunker AM, Jacobsen JR, Roberts WL. Age and gender specific pediatric reference intervals for aldolase, amylase, ceruloplasmin, creatine kinase, pancreatic amylase, prealbumin, and uric acid. Clin Chim Acta. 2011;412(9-10):788-790.
doi pubmed - Zaninotto M, Mion MM, Novello E, Delprete E, Moretti M, Plebani M. Creatine-kinase MB mass: age and sex-associated reference limits in two different platforms that use the same method. Clin Chim Acta. 2009;401(1-2):162-164.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cardiology Research is published by Elmer Press Inc.


