| Cardiology Research, ISSN 1923-2829 print, 1923-2837 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, Cardiol Res and Elmer Press Inc |
| Journal website https://www.cardiologyres.org |
Original Article
Volume 13, Number 4, August 2022, pages 218-227
Soccer and Risk of Cardiovascular Events
Juan Enrique Puche
Cardiology Department, “Puerta del Mar” University Hospital, Cadiz, Spain
Manuscript submitted May 23, 2022, accepted July 7, 2022, published online August 15, 2022
Short title: Soccer and Infarction
doi: https://doi.org/10.14740/cr1398
| Abstract | ▴Top |
Background: Physical and emotional stress have been associated with an increased incidence of acute coronary syndrome (ACS). Sporting events such as soccer matches can cause spectators to experience cardiovascular events. The objective of the present study was to determine whether an association of this type existed during a Spanish league competition.
Methods: We recorded data from patients who were admitted with ACS during 2018 - 2020. Patients were divided into two groups: those who were admitted on the day the local team played and those who were admitted on nonmatch days. We determined various cardiovascular risk factors, including the degree of hostility and anxiety.
Results: Away wins reduced the number of admissions with ACS by 30%, whereas a local loss increased hospitalizations by more than 30%. The profile of patient admitted on match days was a > 65 years old man, smoker (current or past), obese, with worse control of his hypertension, diabetes, and dyslipidemia, poor pharmacological adherence and high anxiety and hostility scores.
Conclusions: A loss by the local team increases the number of admissions with ACS in males with a high burden of cardiovascular risk factors. Primary prevention measures should be taken to reduce the frequency of these events.
Keywords: Anxiety; Cardiovascular risk factors; Soccer; Hostility; Acute coronary syndrome
| Introduction | ▴Top |
Cardiovascular disease continues to be the leading cause of death worldwide. A wide variety of factors have been reported to be determinants of acute coronary syndrome (ACS), such as rupture/erosion of an atheromatous plaque, substance use, and physical/emotional stress [1, 2]. Competitive sports, as soccer, have frequently been suggested to increase the risk of cardiovascular events in predisposed players (e.g., those with coronary artery disease, hypertrophic cardiomyopathy, arrhythmogenic cardiomyopathy) [3]. However, the effect on fans of a team has not been widely studied, even though the association between negative emotions (especially hostility, anxiety, and depression) and cardiovascular disease has been demonstrated [4].
Ad hoc studies coinciding with world championships [5, 6] revealed an increase in the frequency of ACS on days when the local team lost and a decrease when it won [7]. Two meta-analyses [8, 9] concluded that watching soccer matches was associated with a greater risk of fatal and nonfatal infarction, especially in men. Furthermore, the result of the match was related to mortality, with higher rates reported when the team lost and lower rates when it won.
None of these findings have been verified beyond specific matches. Consequently, the results cannot be extrapolated to national league competitions. For this reason, we have designed a study including three soccer seasons, with three primary objectives: 1) To establish the probable correlation between the local incidence of ACS and the day the home soccer team played; 2) To determine the prevalence of cardiovascular risk factors in patients admitted on match days (compared with nonmatch days); and 3) To evaluate anxiety and hostility in this population.
Finally, as an exploratory secondary objective, we sought to probe whether these results were affected by the mandatory severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) lockdown, which prevented fans from attending matches at the stadiums.
| Materials and Methods | ▴Top |
Participants
We performed an observational study based on data from patients who visited the emergency department of a tertiary teaching hospital with chest pain (or equivalent) during 2018 - 2020 (from January 1, 2018, to December 31, 2020). Of the 10,356 patients seen, 1,639 were admitted to various departments, including cardiology (1,027), intensive care (409), internal medicine (191), and others (12) with a diagnosis of acute ST-elevation myocardial infarction (STEMI), non-ST-elevation myocardial infarction (NSTEMI), and unstable angina. We recorded the following epidemiological variables: sex, age, cardiovascular risk factors (arterial hypertension, diabetes mellitus, dyslipidemia, body mass index (BMI), smoking, and chronic kidney disease), and history of ischemic heart disease (IHD). The reference values to determine the degree of control of the different cardiovascular risk factors were based on the current clinical practice guidelines for hypertension, diabetes, and dyslipidemia [10-12].
In addition, the pharmacological treatments of the patients at the time of admission and their degree of compliance were registered to evaluate therapeutic adherence (defined by the World Health Organization (WHO) as “the degree to which the behavior of a patient, in relation to with taking medication, following a diet or modifying life habits, correspond to the recommendations agreed with the health professional” [13]). Good adherence was defined as withdrawal from the pharmacy of more than 80% of the prescriptions.
We also recorded the number of coronary catheterizations the patient underwent, the need (or not) for a stent during the hospital stay, and the in-hospital mortality rate.
Patients were subsequently divided into two groups: those who visited the emergency department or who were admitted with ACS on the days when the local team was playing and patients from days when no match was played. The city where the study was performed had fewer than 120,000 inhabitants and a single first division team (more than 16,000 season ticket holders, i.e., one of the highest ratios of inhabitants to ticket holders in Spain). Our hospital was the only reference hospital for invasive treatment of acute myocardial infarction.
This project fulfilled the requirements of the Declaration of Helsinki and was approved by the local hospital ethics committee (registry number 85.21).
Instruments
The psychological parameters of anxiety and hostility were assessed via postdischarge contact with 109 patients who had ACS on a match day. Of these, 70 agreed to participate in the study and signed an informed consent. In order to avoid comparative bias, we used propensity score matching to select a sample of those patients who were admitted with ACS on days when there was no match (n = 70), contacted them and signed the same informed consent.
We used two self-completed psychological tests that had previously been validated for evaluation of hostility and/or anxiety: 1) the Cook-Medley hostility scale (Ho) [14]: a short form of the Minnesota Multiphasic Personality Inventory (MMPI) with 50 items answered in true/false format; and 2) the Symptom Assessment 45 (SA-45) of Sandin [15], a short form of the Symptom Checklist-90 (SCL-90), which comprises 45 items answered on a Likert scale (0 to 4). The SCL-90 contains a series of nine scales that evaluate nine basic psychopathologic domains: somatization, obsessive-compulsive disorder, interpersonal sensitivity, depression, anxiety, hostility, phobic anxiety, paranoid ideation, and psychoticism.
Data analysis
Data were analyzed using SPSS, Version 23.0. Statistical significance was set at P < 0.05. Continuous variables were expressed as mean ± standard deviation; qualitative variables were expressed as frequency and percentage. Hypotheses were analyzed using the t-test (for quantitative variables, after confirmation of normality using the Kolmogorov-Smirnov test) or the Chi-square test (qualitative variables). More than two cohorts were compared using analysis of variance with subanalyses when applicable.
| Results | ▴Top |
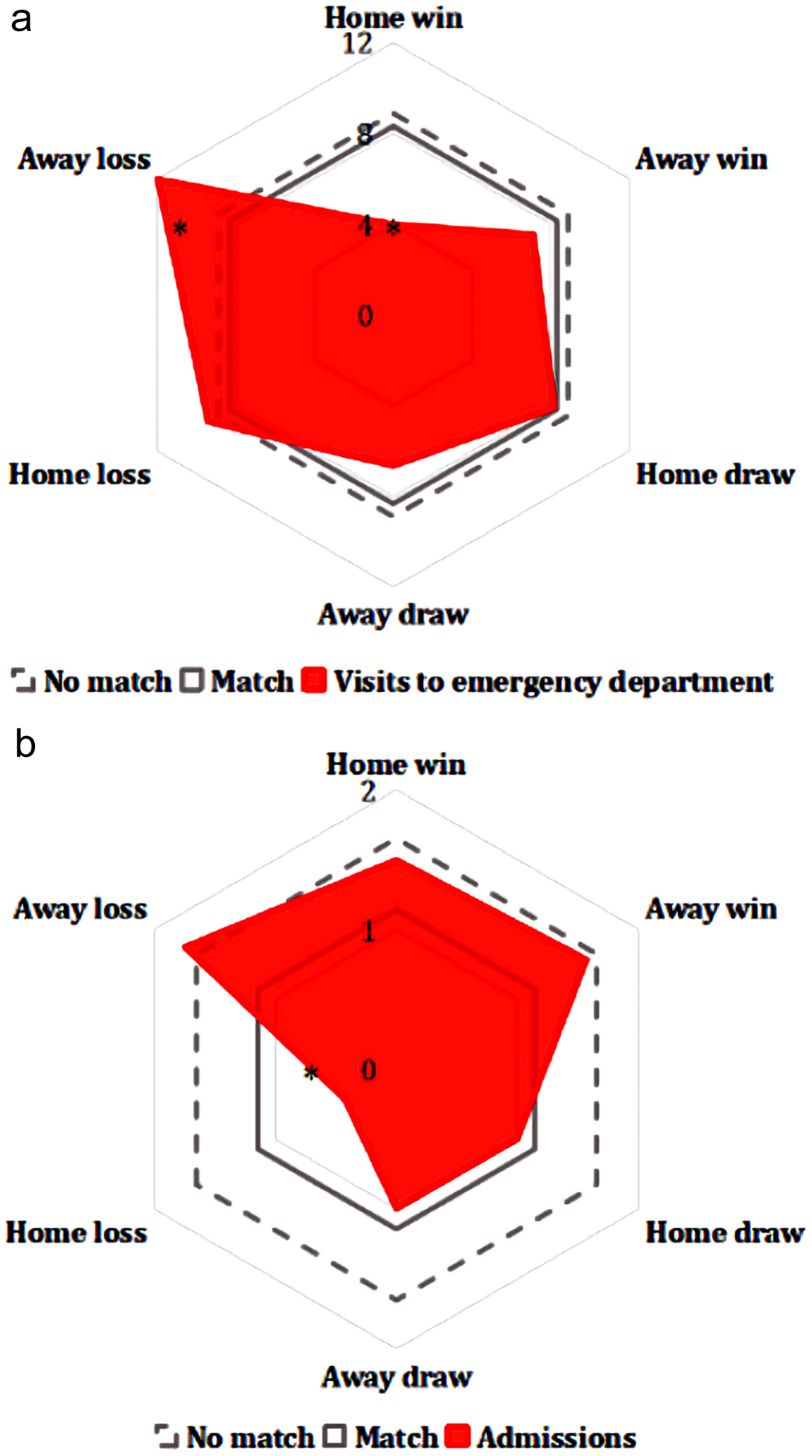
During the years 2018 - 2020 (from January 1, 2018, to March 1, 2020, before the SARS-CoV-2 pandemic), the mean daily number of visits to the emergency department with chest pain was 10.1 ± 1.2 on nonmatch days (Fig. 1a, broken black line), whereas on match days this fell by 20% (8.0 ± 1.1 visits per day, P < 0.05) (Fig. 1a, continuous black line). However, when we break data down by score, we found that the number of visits increased by 15% on the days the local team lost at home (Fig. 1a, green line) (P < 0.05).
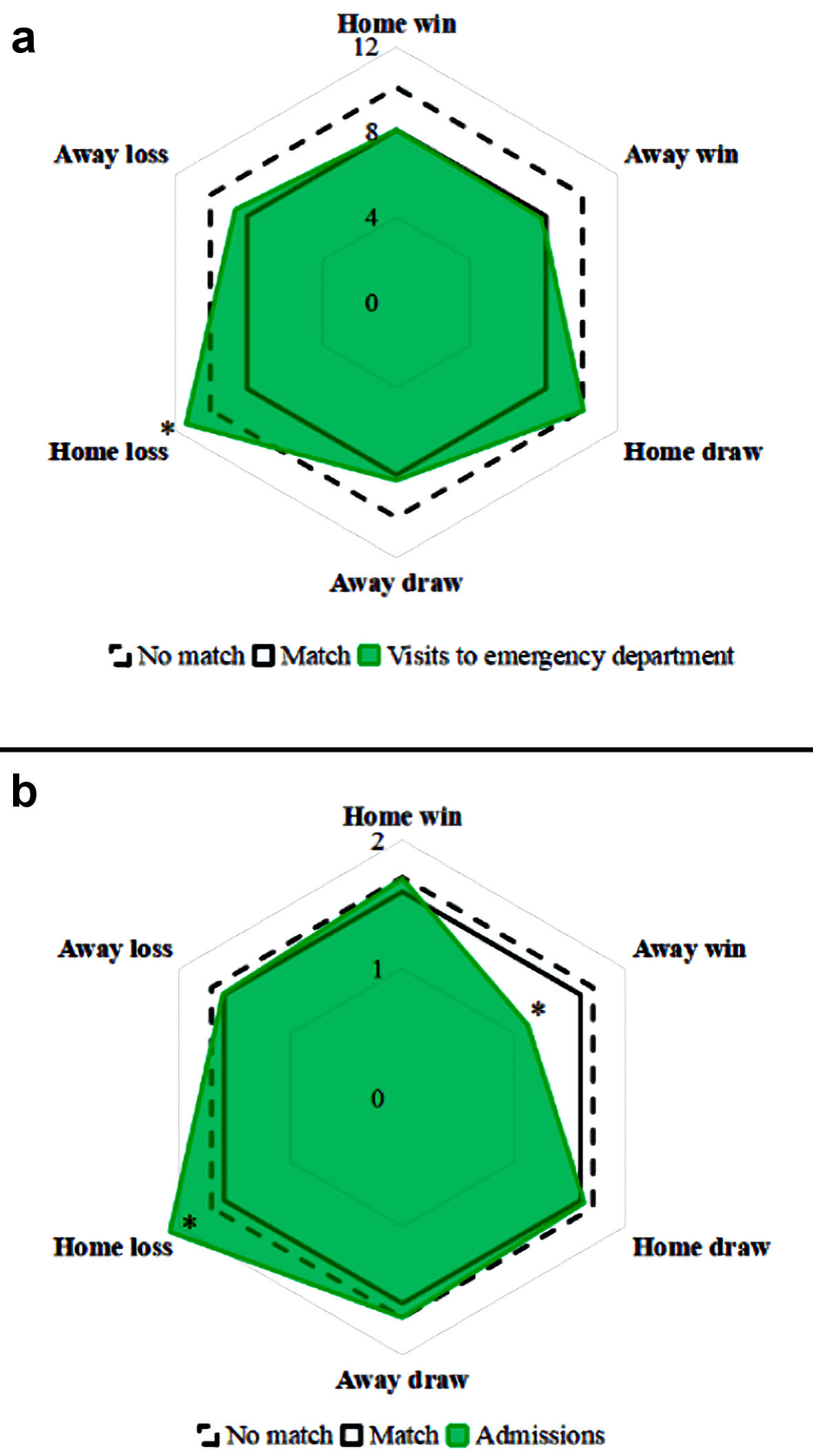 Click for large image | Figure 1. Visits to the emergency department with chest pain (a) and admissions with acute coronary syndrome (b). *P < 0.05 vs. mean admissions on match day. |
As for daily admissions with ACS (STEMI, NSTEMI, and unstable angina), we recorded mean of 1.7 ± 0.3 hospitalizations/day when the team was not playing, that is, very similar to the 1.6 ± 0.2 hospitalizations/day on the days the team was playing (irrespective of the score) (Fig. 1b, black lines, P = nonsignificant (NS)). However, on those days that the team had an away win, admissions fell by 30% (1.1 ± 0.2, P < 0.05), with a rebound on the days the team lost at home (2.1 ± 0.2, P < 0.05) (Fig. 1b, green line).
When the data were analyzed by sex, we found the following results (Fig. 2a): 1) The incidence of ACS was higher among males, both on match days and on nonmatch days (two- to three-fold more, P < 0.05); and 2) Both the increase in the number of hospitalizations with ACS on days the home team lost and the decrease in the number of admissions on the days they won were observed mainly for males (P < 0.05).
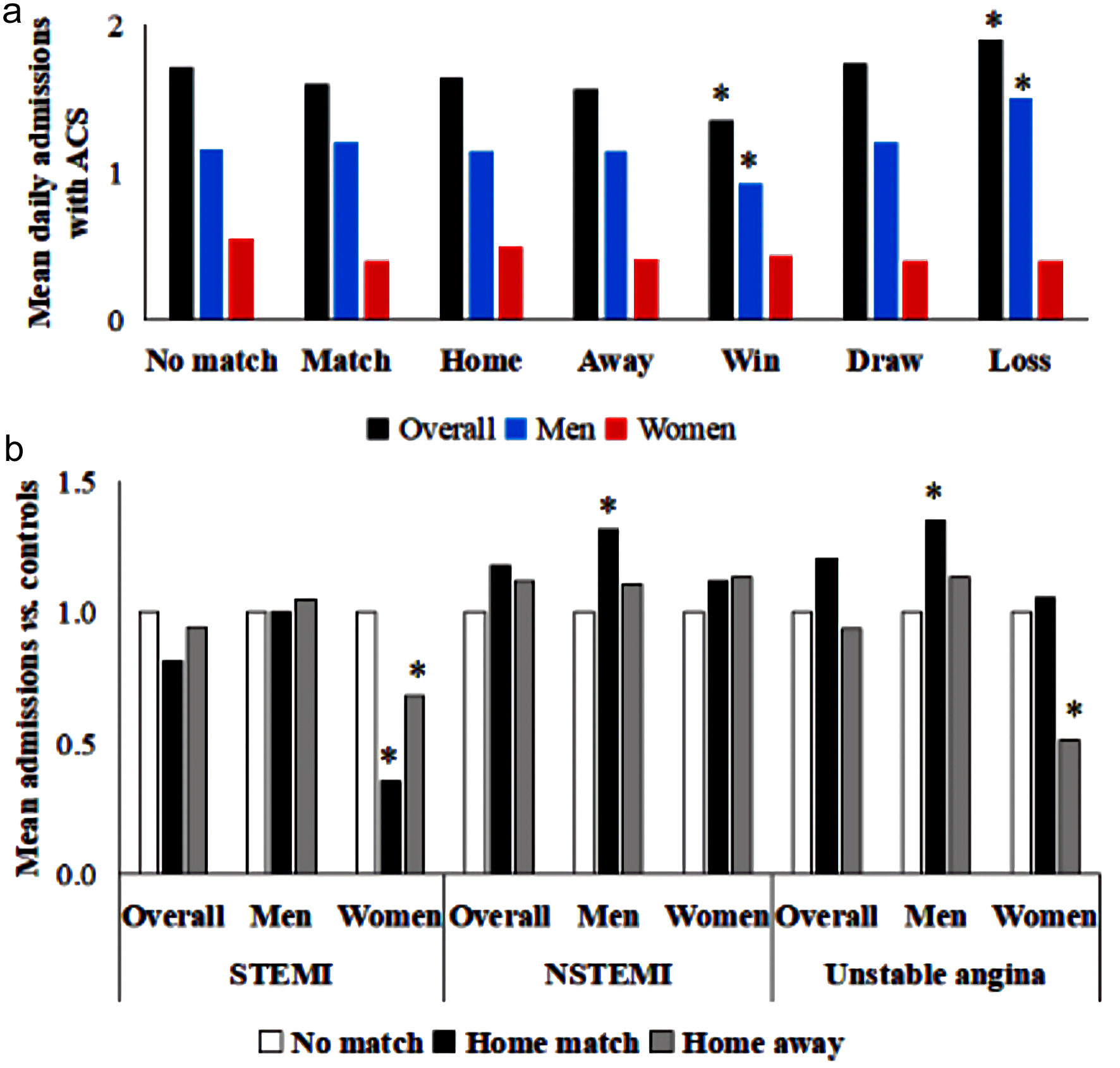 Click for large image | Figure 2. Mean admissions by sex and result of match (a) and type of acute coronary syndrome (b). *P < 0.05 vs. nonmatch days. ACS: acute coronary syndrome; NSTEMI: non-ST-elevation myocardial infarction; STEMI: ST-elevation myocardial infarction. |
Furthermore, when we studied the different types of ACS, we found that the increase in hospitalizations was for non-ST-segment elevation ACS (NSTEMI and unstable angina) among males when the team played at home (Fig. 2b, P < 0.05). Curiously, the number of admissions with STEMI fell among females on match days (P < 0.05). In addition, in an attempt to elucidate the pathophysiology underlying the NSTEMI (type 1 vs. type 2), we analyzed the number of catheterizations that required any stent implantation after finding a culprit lesion. In non-match days, a culprit lesion was found in 77.5% of catheterizations. Interestingly, on match days stent implantation was needed in 89.3% of cases, reaching statistical significance (P < 0.05) and meaning a higher proportion of type 1 NSTEMI on these match days.
The profile of the patient most likely to experience ACS on match days was that of a male smoker (current or past) aged > 65 years with hypertension, diabetes (around 40%), dyslipidemia (60%), and overweight/obesity (85%), of whom up to one-third had a personal history of IHD (Table 1). When we compared this profile with that of patients admitted on days when no matches were played, we recorded a higher percentage of men with poorer control of cardiovascular risk factors (CVRFs) such as increased glycosylated hemoglobin, low-density lipoprotein cholesterol (LDL-C), and BMI, as well as more frequent smoking (P < 0.05). However, the patients were more likely not to have had previous IHD (P < 0.05). In this case, no statistically significant differences between men and women were observed with respect to arterial hypertension, diabetes mellitus, or dyslipidemia. Women who were hospitalized on match days were more likely to be smokers, whereas the men were more likely to be obese (P < 0.05) (Supplementary Material 1, www.cardiologyres.org).
 Click to view | Table 1. Baseline Clinical Characteristics Before COVID-19 |
Likewise, the degree of adherence to treatment was measured. As it is shown in Figure 3, patients who developed an ACS on days of match had significantly worse pharmacological adherence compared to those who were admitted on days of no match (P < 0.05): 49.6% (95% confidence interval (CI): 41.7 - 57.5) for antihypertensive drugs, 44.2% (95% CI: 36.3 - 52.1) for antidiabetics, and 50.1% (95% CI: 42.2 - 58.0) for lipid-lowering drugs in days of match vs. 65.9% (95% CI: 63.2 - 68.6), 61.0% (95% CI: 58.2 - 63.8), and 68.8% (95% CI: 66.1 - 71.5) on nonmatch days, respectively.
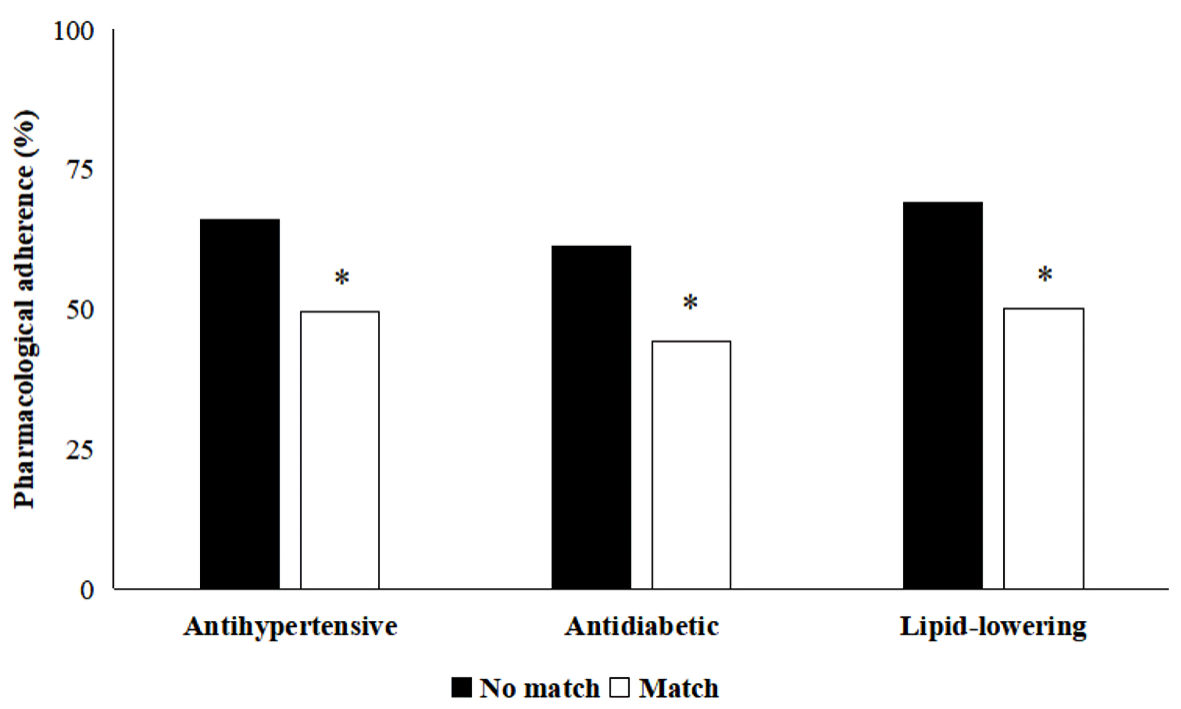 Click for large image | Figure 3. Pharmacological adherence to antihypertensive, antidiabetic, and lipid-lowering drugs. *P < 0.05 vs. nonmatch days. |
Analysis of the characteristics of the admission revealed no statistically significant differences with respect to the mean number of days of hospital stay (5.5 ± 0.6 vs. 5.3 ± 0.9 days, P = NS) or need for percutaneous revascularization (0.7 vs. 0.8 procedures/patient, P = NS). A decrease was observed in the number of in-hospital deaths of patients who were admitted on match days (4.6% vs. 7.5% on nonmatch days, P < 0.05), due to a reduction on the days the team played away (2.6% vs. 6.7% for home matches, P < 0.05).
As for the patient’s psychological profile, higher scores were recorded for anxiety in patients admitted on match days than in patients admitted on nonmatch days (Fig. 4a, P < 0.05). Furthermore, a comparison by sex revealed a greater score for hostility among men, especially in the case of patients who were admitted with ACS on match days (Fig. 4b, P < 0.05). Similarly, significant differences between the sexes were recorded on the depression and interpersonal sensitivity scales using the SA-45 questionnaire (Table 2).
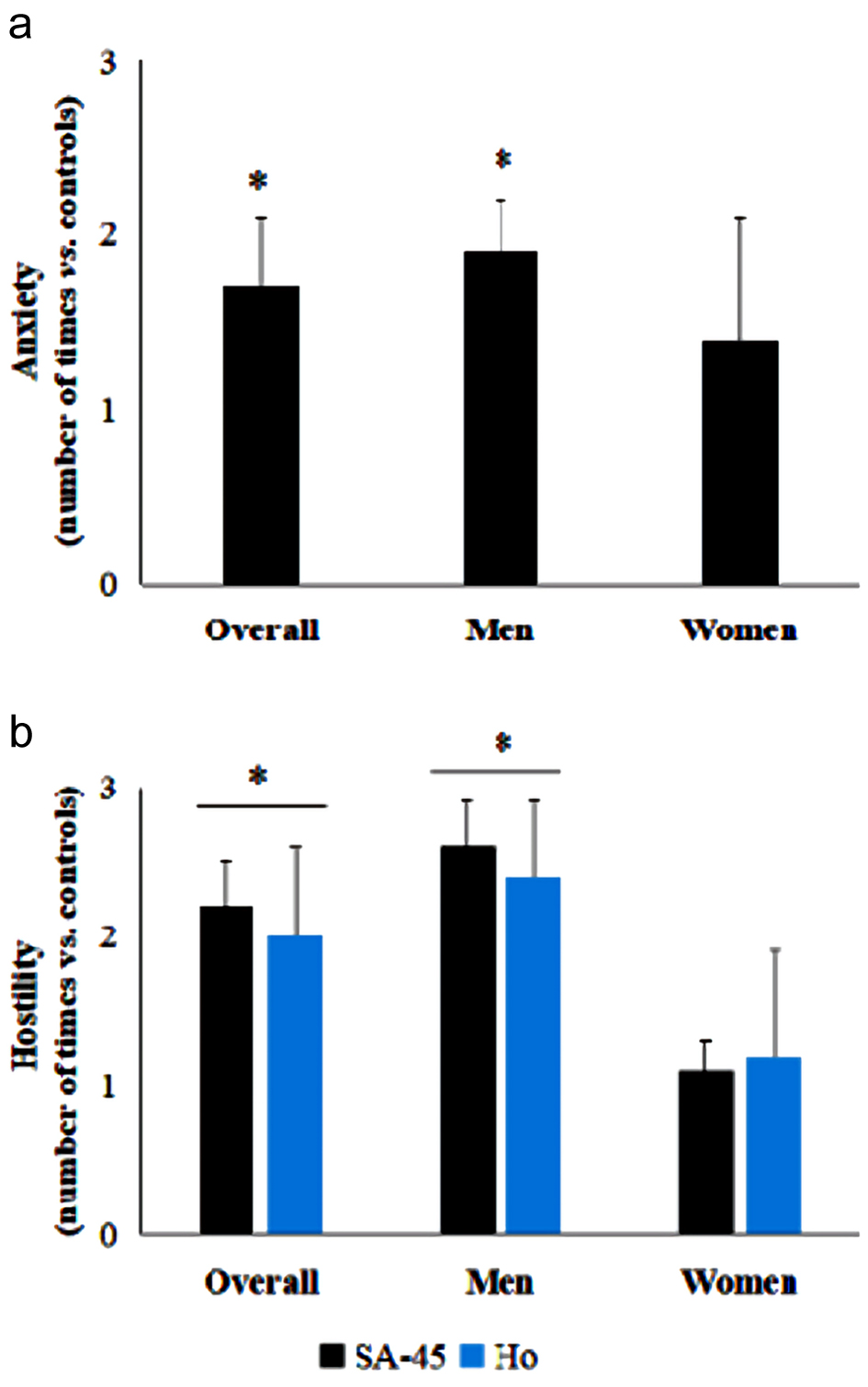 Click for large image | Figure 4. Psychological dimensions of anxiety and hostility among patients admitted with ACS. (a) Values on the anxiety scale obtained with the SA-45 questionnaire. (b) Results for the hostility dimension of the SA-45 and Ho questionnaires. The data shown are the result of comparing with controls (patients admitted on nonmatch days). *P < 0.05 vs. controls. ACS: acute coronary syndrome; Ho: Cook-Medley hostility scale; SA-45: Symptom Assessment 45. |
 Click to view | Table 2. Score on the Remaining Scales of the SA-45 Questionnaire: Somatization, Obsessive-Compulsive Disorder, Interpersonal Sensitivity, Depression, Phobic Anxiety, Paranoid Ideation, and Psychoticism |
Finally, in an attempt to determine whether attending the stadium had an effect on these findings, we performed an independent analysis of data from June 2020 (after the coronavirus disease 2019 (COVID-19) lockdown, when sporting competitions without attendance by the public were restarted). During this period, we found a trend towards a lower number of visits to the emergency department overall on match days (Fig. 5a, continuous grey line, P = NS). A notable decrease was recorded when the team won at home compared with losing at home (Fig. 5a, red line, P < 0.05).
 Click for large image | Figure 5. Visits to the emergency department with chest pain (a) and admissions with acute coronary syndrome (b) after lockdown. *P < 0.05 vs. mean admissions on match days and nonmatch days. |
With respect to admissions, hospitalizations decreased significantly on match days after the start of the COVID-19 pandemic (Fig. 5b, continuous grey line, P < 0.05), as was a marked decrease on days the team lost at home (P < 0.05). Patients admitted on match days during this period were characterized by poorer control of CVRFs (e.g., arterial hypertension, dyslipidemia, diabetes mellitus, and overweight), with fewer than 25% of patients having a history of IHD (vs. 41.9% on days when the local team was not playing) (Table 3).
 Click to view | Table 3. Baseline Clinical Characteristics of Patients After the COVID-19 Lockdown |
| Discussion | ▴Top |
The press’ headlines in the “heart-stopping match” style may be losing its figurative sense, since the results from this study defend that more ACS may be occurring in a city on days when the local team loses.
Our first finding was the lower number of visits to the emergency department with chest pain on days the home team played, thus lending some meaning to the notion of soccer as “the opium of the people”. This trend only varied when the team lost, in which case visits to the emergency department were more frequent.
In addition to visits to the emergency department with chest pain (and its broad differential diagnosis), we found a lower number of admissions with ACS on days the local team won (30% fewer) and a higher number when they lost (by 30% more). These findings are consistent with previously published data in ad hoc studies on world championships, which reported an increased risk of hospitalization with ACS and cardiovascular mortality on days when the local team lost and a decrease on days when they won [3-9]. However, other studies did not find significant differences [16].
The fact that these variations were recorded with respect to non-ST-segment elevation ACS confirms theory on the pathophysiology of the spectrum of ACS, where unstable angina (and, to a lesser extent, NSTEMI) can more easily be triggered in stressful situations, where, among others, platelet activation is increased (as it is seen in our study, where there is an increment of type 1 NSTEMI on match days) [17, 18]. From a more biopsychosocial perspective, it is not in vain that the association between stress and IHD has gradually been reinforced in recent years [4, 19-21]. Specifically, we have seen how negative feelings (e.g., hostility, anger, sadness, indignation, and frustration) can act as triggers of cardiovascular events. In 1996, Williams [22] developed the concept of the hostility syndrome to define a set of signs and symptoms that predispose to cardiovascular disease. Basically, this is characterized by facility for anger with increased sympathetic reactivity in situations that bring out hostility, together with excessive risk behaviors, such as smoking, drinking alcohol, and overeating (associated with overweight/obesity), which are used as coping mechanisms.
Therefore, we can see how, in addition to the excitement of the match itself, the score can increase the risk of hospitalization for ACS, since, when faced with a loss, fans experience more negative feelings. In contrast, the positive feelings generated by a win (e.g., euphoria, admiration, pride, satisfaction, and gratitude) seem to reduce the number of ACS, thus potentially providing a hypothesis for future studies aimed at cardiovascular prevention.
Furthermore, when the results are broken down by sex, we observe an unequal response: whereas men experience an increase in non-ST-segment elevation ACS on match day (especially with a loss by the home team), women seem to have a lower cardiovascular risk on these days (thus leading us to consider soccer as a “cardioprotective factor” in women). One possible explanation is the difference in concentrations of testosterone and cortisol between the sexes and their possible influence on levels of hostility/anger [21-23], which, as commented on above, are associated with disease onset and cardiovascular mortality. Another factor potentially involved could be the burden of CVRFs. International studies [24, 25] have shown that female sex is associated with a higher burden and poorer control of these factors, both in primary and in secondary prevention. However, in the present study, we found no significant differences between the sexes for arterial hypertension, diabetes mellitus, or dyslipidemia, potentially pointing to a relative increase in the frequency of these factors in men (compared with other published series [24, 25]), which would make them more likely to develop ACS on match days. In addition, irrespective of sex, it is important to note that patients admitted on match days have poorer control of their cardiovascular risk factors: worse glycemic and lipidic controls, and higher BMI and smoking rates.
Indeed, in last decades we are witnessing an insufficient degree of control of CVRF in European countries, including in secondary prevention of cardiovascular disease [26, 27], and low compliance with treatment seems to be one of the causal factors [27]. Adherence to prophylactic medications (acetylsalicylic acid, β-blockers, angiotensin-converting enzyme (ACE) inhibitors, statins, etc.) 1 year after discharge is approximately 50% [26, 27]. For this reason, the WHO has classified it as a global problem of great magnitude [13], given that correct adherence has been associated with a 20% reduction in cardiovascular disease risk and a 38% reduction in all-cause mortality [26]. In the series of patients presented in this article, therapeutic adherence among patients admitted in match days was 26.4% worse on average than that of those patients who were admitted on nonmatch days. Some causes for this poor adherence have been described [25, 26]: 1) those related to the drug (side effects, price, dosage, etc.); 2) the disease (asymptomatic, evolution time, comorbidities, etc.); 3) the health environment (ease of access, frequency of consultations, lack of records, etc.); 4) the professional (lack of communication, poor doctor-patient relationship, therapeutic inertia, etc.); and 5) the patient (forgetfulness, lack of patient motivation and/or degree of understanding of the severity of their disease, socio-economic-cultural level, etc.). Regarding the first three factors there is little to be done from our daily performance. However, for the last two aspects (professional and patient) there is a room for improvement, from intensifying preventive treatments (which has been demonstrated to be more successful than the conventional care approach [28]), to promoting a greater degree of involvement on the part of the patient in the prevention of their disease [29].
In this article, we extended the follow-up times of other studies up to 3 years. As a result, we took advantage of the absence of fans in stadiums (after the prohibition implemented because of COVID-19 in 2020) to investigate possible consequences thereof. In this sense, after lockdown, we noticed a paradigm shift when the local team lost at home, with a lower number of admissions because of ACS. Therefore, we hypothesize that, in addition to the score, other variables may play a role in the incidence of IHD, for example, the tense atmosphere in the stadium which could generate stress, anxiety, and hostility in some cases. This idea was consistent with previous report where ACSs among spectators in a soccer stadium were measured [30].
Among the limitations of this study, it should be noted its retrospective and single-center design, and the fact that patients were not questioned about their soccer preferences. However, as stated at Materials and Methods, the soccer team of the city where the study has been performed was the unique at first division and has one of the highest ratios of inhabitants to ticket holders in Spain. This, along with the fact that our hospital is the only reference hospital for invasive treatment of acute myocardial infarction at the city, reduces the likelihood of other important bias.
Since the results described in this study may be extended to different sports (including rugby, baseball, hockey, etc.) [31], our recommendations for fans attending sports events include the following: 1) “There is no such thing as a small rival” where cardiovascular risk is concerned. It is important to control all risk factors, especially on match days, as follows: avoid intake excesses (especially food and alcohol), give up smoking, take the necessary medication for hypertension, diabetes, and high cholesterol; 2) Perform moderate physical exercise daily in order to acquire the habit “match by match”; 3) When the match becomes tense, try to see it in relative terms and practice strategies for managing emotions: your life lasts longer than 90 min and is worth more than three points.
In conclusion, we performed the first study to confirm the association between soccer calendar, ACSs, and patient profile, finding a higher number of ACS when the local team lost at home in a specific subject: a male, aged > 65 years, smoker (current or past), obese, with worse control of his hypertension, diabetes, and dyslipidemia, poor pharmacological adherence and high anxiety and hostility scores.
Therefore, given that our team’s score does not depend on us, it seems necessary to develop future studies in this field (with population from both in and outside stadiums, comparing supporters vs. people who do not like soccer, virtual vs. real soccer, etc.) and to improve measures to promote cardiovascular disease prevention in order to enjoy the spectacle as safely as possible.
| Supplementary Material | ▴Top |
Suppl 1. Differences by sex in baseline characteristics of patients during the pre-COVID period.
Acknowledgments
I would like to thank to the Cardiology and Emergency Services of the Puerta del Mar University Hospital in Cadiz for the great work carried out; it would have been impossible to carry out this study without them.
Financial Disclosure
The author declares that he has not received any funding from public agencies, the commercial sector, or nonprofit organizations
Conflict of Interest
The author declares that he has no conflict of interest with respect to the present publication.
Informed Consent
Informed consent was obtained.
Data Availability
The data supporting the findings of this study are available from the corresponding author upon reasonable request.
Abbreviations
ACE: angiotensin-converting enzyme; ACS: acute coronary syndrome; BMI: body mass index; BP: blood pressure; COVID-19: coronavirus disease 2019; CVRFs: cardiovascular risk factors; Ho: Cook-Medley hostility scale; IHD: ischemic heart disease; LDL-C: low-density lipoprotein cholesterol; MMPI: Minnesota Multiphasic Personality Inventory; NSTEMI: non-ST-elevation myocardial infarction; SA-45: Symptom Assessment 45; SARS-CoV-2: severe acute respiratory syndrome coronavirus 2; SCL-90: Symptom Checklist-90; STEMI: ST-elevation myocardial infarction; UA: unstable angina; WHO: World Health Organization
| References | ▴Top |
- Kivimaki M, Steptoe A. Effects of stress on the development and progression of cardiovascular disease. Nat Rev Cardiol. 2018;15(4):215-229.
doi pubmed - Frishman WH, Del Vecchio A, Sanal S, Ismail A. Cardiovascular manifestations of substance abuse: part 2: alcohol, amphetamines, heroin, cannabis, and caffeine. Heart Dis. 2003;5(4):253-271.
doi pubmed - Egger F, Scharhag J, Kastner A, Dvorak J, Bohm P, Meyer T. FIFA Sudden Death Registry (FIFA-SDR): a prospective, observational study of sudden death in worldwide football from 2014 to 2018. Br J Sports Med. 2022;56(2):80-87.
doi pubmed - Sandin B. Papel de las emociones negativas en el trastorno cardiovascular: un analisis critico. Revista de Psicopatologia y Psicologia Clinica. 2002;7(1):1-18.
doi - Wilbert-Lampen U, Leistner D, Greven S, Pohl T, Sper S, Volker C, Guthlin D, et al. Cardiovascular events during World Cup soccer. N Engl J Med. 2008;358(5):475-483.
doi pubmed - Carroll D, Ebrahim S, Tilling K, Macleod J, Smith GD. Admissions for myocardial infarction and World Cup football: database survey. BMJ. 2002;325(7378):1439-1442.
doi pubmed - Berthier F, Boulay F. Lower myocardial infarction mortality in French men the day France won the 1998 World Cup of football. Heart. 2003;89(5):555-556.
doi pubmed - Lin LL, Gu HY, Yao YY, Zhu J, Niu YM, Luo J, Zhang C. The association between watching football matches and the risk of cardiovascular events: A meta-analysis. J Sports Sci. 2019;37(24):2826-2834.
doi pubmed - Wang H, Liang L, Cai P, Zhao J, Guo L, Ma H. Associations of cardiovascular disease morbidity and mortality in the populations watching major football tournaments: A systematic review and meta-analysis of observational studies. Medicine (Baltimore). 2020;99(12):e19534.
doi pubmed - Grant PJ, Cosentino F. The 2019 ESC Guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD: New features and the 'Ten Commandments' of the 2019 Guidelines are discussed by Professor Peter J. Grant and Professor Francesco Cosentino, the Task Force chairmen. Eur Heart J. 2019;40(39):3215-3217.
doi pubmed - Mach F, Baigent C, Catapano AL, Koskinas KC, Casula M, Badimon L, Chapman MJ, et al. 2019 ESC/EAS Guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk. Eur Heart J. 2020;41(1):111-188.
doi pubmed - Verdecchia P, Reboldi G, Angeli F. The 2020 International Society of Hypertension global hypertension practice guidelines - key messages and clinical considerations. Eur J Intern Med. 2020;82:1-6.
doi pubmed - World Health Organization; Geneva: 2003. Adherence to long term therapies: evidence for action. Edited by Eduardo Sabate. World Health Organization. 2003. https://apps.who.int/iris/handle/10665/42682.
- Cook WW, Medley DM. Proposed hostility and pharisaic-virtue for the MMPI. Journal of Applied Psychology. 1954;38:414-418.
doi - Sandin B, Valiente RM, Chorot P, Santed MA, Lostao L. [SA-45: a brief form of the SCL-90]. Psicothema. 2008;20(2):290-296.
- Martins JL, Adrega T, Santos L, Afreixo V, Viana J, Santos J. Are soccer matches dangerous for patients with heart disease? The HeartAtaque trial - a prospective pilot study. Rev Port Cardiol (Engl Ed). 2018;37(8):645-653.
doi pubmed - Roffi M, Patrono C, Collet JP, Mueller C, Valgimigli M, Andreotti F, Bax JJ, et al. 2015 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: Task Force for the Management of Acute Coronary Syndromes in Patients Presenting without Persistent ST-Segment Elevation of the European Society of Cardiology (ESC). Eur Heart J. 2016;37(3):267-315.
doi pubmed - Grignani G, Soffiantino F, Zucchella M, Pacchiarini L, Tacconi F, Bonomi E, Pastoris A, et al. Platelet activation by emotional stress in patients with coronary artery disease. Circulation. 1991;83(4 Suppl):II128-136.
- Steptoe A, Brydon L. Emotional triggering of cardiac events. Neurosci Biobehav Rev. 2009;33(2):63-70.
doi pubmed - Edmondson D, Newman JD, Whang W, Davidson KW. Emotional triggers in myocardial infarction: do they matter? Eur Heart J. 2013;34(4):300-306.
doi pubmed - Davidson KW. Emotional predictors and behavioral triggers of acute coronary syndrome. Cleve Clin J Med. 2008;75(Suppl 2):S15-19.
doi pubmed - Williams RB. Coronary-prone behaviors, hostility, and cardiovascular health: Implications for behavioral and pharmacological interventions. In: Orth-Gomer y K, Schneiderman N (Eds.). Behavioral medicine approaches to cardiovascular disease prevention. Mahwah, NJ: LEA. 1995:161-168.
- Armstrong T, Wells J, Boisvert DL, Lewis RH, Cooke EM, Woeckener M, Kavish N. An exploratory analysis of testosterone, cortisol, and aggressive behavior type in men and women. Biol Psychol. 2021;161:108073.
doi pubmed - De Smedt D, De Bacquer D, De Sutter J, Dallongeville J, Gevaert S, De Backer G, Bruthans J, et al. The gender gap in risk factor control: Effects of age and education on the control of cardiovascular risk factors in male and female coronary patients. The EUROASPIRE IV study by the European Society of Cardiology. Int J Cardiol. 2016;209:284-290.
doi pubmed - Hyun K, Negrone A, Redfern J, Atkins E, Chow C, Kilian J, Rajaratnam R, et al. Gender difference in secondary prevention of cardiovascular disease and outcomes following the survival of acute coronary syndrome. Heart Lung Circ. 2021;30(1):121-127.
doi pubmed - Orozco-Beltran D, Carratala-Munuera C, Gil-Guillen V. Mejorar la adherencia: una de las acciones mas eficientes para aumentar la supervivencia de los pacientes en prevencion secundaria. Rev Esp Cardiol Supl. 2015;15:12-18.
doi - Dilla T, Valladares A, Lizan L, Sacristan JA. [Treatment adherence and persistence: causes, consequences and improvement strategies]. Aten Primaria. 2009;41(6):342-348.
doi pubmed - Vazquez-Garcia R, Puche JE, Mialdea D, Bartolome D, Delgado W. Consulta virtual de lipidos despues de sindrome coronario agudo. Rev Esp Cardiol. 2021;75:91-93.
doi pubmed - Giannopoulos G, Karageorgiou S, Vrachatis D, Kousta M, Tsoukala S, Letsas K, Siasos G, et al. Usefulness of a structured adult education program in modifying markers of cardiovascular risk after acute myocardial infarction. Am J Cardiol. 2020;125(6):845-850.
doi pubmed - Serra Grima R, Carreno MJ, Tomas Abadal L, Brossa V, Ligero C, Pons J. [Acute coronary events among spectators in a soccer stadium]. Rev Esp Cardiol. 2005;58(5):587-591.
doi pubmed - Maturana MA, Glover EA, Raja J, Dornbush SR, Alexander J, Blount C, Khouzam NR, et al. Are die-hard football or other sports fans at risk of cardiovascular events? Curr Probl Cardiol. 2021;46(3):100743.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cardiology Research is published by Elmer Press Inc.


