| Cardiology Research, ISSN 1923-2829 print, 1923-2837 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, Cardiol Res and Elmer Press Inc |
| Journal website https://www.cardiologyres.org |
Original Article
Volume 13, Number 3, June 2022, pages 128-134
Comparison of Tricuspid Regurgitation Severity Between Cardiac Resynchronization Therapy Versus Right Ventricular Pacing in Patients With Chronic Obstructive Pulmonary Disease
James Livesaya, Benjamin Fogelsona, Hassan Tahira, Raj Baljepallya, b, c
aDepartment of Medicine, University of Tennessee Graduate School of Medicine, Knoxville, TN, USA
bHeart Lung Vascular Institute, University of Tennessee Medical Center, Knoxville, TN, USA
cCorresponding Author: Raj Baljepally, Division of Cardiology, Heart Lung Vascular Institute, University of Tennessee Medical Center, Knoxville, TN 37920, USA
Manuscript submitted February 9, 2022, accepted April 28, 2022, published online June 16, 2022
Short title: TR in COPD Patients With CRT vs. Non-CRT
doi: https://doi.org/10.14740/cr1365
| Abstract | ▴Top |
Background: Right ventricular (RV) lead placement can worsen tricuspid regurgitation (TR). TR is known to be associated with lower survival irrespective of left ventricular ejection fraction (LVEF) or pulmonary hypertension (PH). Patients with chronic obstructive pulmonary disease (COPD) often have PH and pre-existent TR with higher morbidity and mortality from worsening TR. Prior studies are lacking to indicate if cardiac resynchronization therapy (CRT) may be more beneficial in lessening TR in COPD patients. Therefore, we sought to study if patients with COPD will have less TR with CRT versus non-CRT devices.
Methods: We performed a retrospective, single-center analysis on 154 COPD patients (mean age = 71.69 ± 10.58, males = 54.14%) that required single-chamber (n = 27), dual-chamber (n = 90), or CRT (n = 37) devices. TR severity, LVEF and right ventricular systolic pressure (RVSP) were evaluated by two cardiologists in a blinded fashion. Analysis of variance (ANOVA) and Chi-square tests were applied for continuous and categorical variables respectively. The primary endpoint was a change in the severity of TR comparing pre-device versus post-device echocardiogram. Secondary endpoints included changes in LVEF and RVSP.
Results: COPD patients, who underwent a CRT device had a significantly lower incidence of worsening TR (16%) when compared to single- (37%) (P = 0.001) and dual-chamber devices (30%) (P = 0.02). The increase in RVSP was similar between the groups. There was an expected improvement in LVEF in the CRT group.
Conclusions: COPD patients receiving a CRT device were least likely to have worsening TR, compared to single- or dual-chamber devices. Since both COPD and progression in TR may result in poor outcomes, our study may suggest that an upfront strategy of CRT rather than a single- or dual-chamber device may be more beneficial in COPD patients, especially with pre-existent TR.
Keywords: Tricuspid regurgitation; Chronic obstructive pulmonary disease; Cardiovascular implantable electronic device; Cardiac resynchronization therapy; Right ventricular pacing
| Introduction | ▴Top |
Chronic obstructive pulmonary disease (COPD) is a prevalent, complex respiratory disease that can affect many organ systems in the body, including the cardiovascular system [1]. Patients with severe and non-severe COPD have been shown to have structural changes of the right heart, which can ultimately lead to the development of pulmonary hypertension (PH) [1]. Increasing COPD severity and hyperinflation of the lungs have also been associated with worsening tricuspid regurgitation (TR) severity [2]. Regardless of left ventricular (LV) function or pulmonary artery pressure, patients with TR are known to have a lower survival and higher mortality rates compared to those with a normal functioning tricuspid valve [3-5]. However, long-term prognosis and mortality rates can be further worsened in patients with diseases predisposed to elevated pulmonary artery pressures and TR, such as COPD. In addition to chronic lung disease, studies have also shown that the placement of cardiac device leads within the right ventricle can cause or worsen preexisting TR [6, 7].
Cardiovascular implantable electronic device (CIED)-mediated TR remains a growing concern as the number of cardiac device procedures continues to increase every year. According to Addetia et al, the prevalence of cardiac device-related TR has been reported to be as high as 45% [8]. Consequently, the incidence of CIED-mediated TR is expected to rise with the increasing rate of cardiac device implantations. The development of TR following permanent pacemaker (PPM) and implantable cardioverter-defibrillator (ICD) placement has been well established in the literature [8-14]. In extreme cases, patients can develop severe TR leading to right ventricle failure that requires surgical treatment of the tricuspid valve [8, 10]. Despite its rising prevalence, the exact mechanism for CIED-mediated TR is unknown. While some experts argue that device leads within the right ventricle cause physical damage and deformity of the tricuspid valve, others believe it is due to functional valve abnormalities caused by pacing of the right ventricle. Despite this controversy, most experts agree that patients who develop or have worsening preexisting TR following right ventricular (RV) lead placement have worse outcomes and increased mortality [6, 7].
Unlike standard PPMs and ICDs, the effects of cardiac resynchronization therapy (CRT) devices on the tricuspid valve are not well understood. The cardiovascular benefits of CRT are well known and supported by multiple large clinical studies, including the MIRCALE ICD and MADIT-CRT trials [15, 16]. CRT has been shown to have significant positive effects on right ventricle function and improvement of mitral regurgitation (MR) after upgrading from RV pacing devices [17-19]. However, the effects of CRT on TR in patients with COPD are inconsistent based on the limited data currently available [7, 20, 21]. Despite the benefits of CRT on LV dyssynchrony, MR, and right ventricle function, there are no prior studies to indicate if CRT may be more beneficial in lessening TR in patient with COPD. Therefore, the main objective of this study was to determine if patients with COPD have less CIED-mediated TR with CRT versus non-CRT devices.
| Materials and Methods | ▴Top |
This is a single-center retrospective observational study performed at the University of Tennessee Medical Center, Knoxville. The study was approved by the Institutional Review Board (IRB) at the University of Tennessee Graduate School of Medicine, Knoxville, TN with IRB number 4326. The study was conducted in compliance with the ethical standards of the responsible institution on human subjects as well as the Helsinki Declaration.
The study included patients between July 2013 and September 2018 with the diagnosis of COPD that required either single-chamber, dual-chamber, or biventricular implantable subcutaneous pacemakers or defibrillators as clinically indicated by the International Classification of Diseases, 10th Revision (ICD-10) codes. Patients had to have a pre-implantation transthoracic echocardiogram (TTE) and greater than 1-year post-implantation TTE. Each TTE was retrospectively reviewed for TR severity, left ventricular ejection fraction (LVEF), and right ventricular systolic pressure (RVSP). TR severity was determined using a combination color and continuous wave Doppler (CWD). Mild TR is defined with a small color jet, narrow vena contracta, and faint TR jet on CWD. While severe TR is defined by a large color jet, wide vena contracta, and dense parabolic jet on CWD.
A total of 445 patients with COPD and subcutaneous implantable devices were reviewed during this study. Of the 445 patients, 154 had both a pre and post echocardiograms meeting inclusion criteria for this study. Basic demographics, TR severity, LVEF, and RVSP were collected and analyzed for each patient. One-way analysis of variance (ANOVA) test was used for continuous variables and Chi-square test was used for categorical variables. The primary endpoint was to access for change in severity of TR following device implantation. Secondary endpoints include change in LVEF and RVSP. Statistical analysis was performed using GraphPad Prism, Version 9.
| Results | ▴Top |
A total of 154 patients with COPD, subcutaneous implantable devices, and both a pre-device TTE and post-device TTE were included in this study (Table 1). Patients were divided into three groups based on the type of device that was implanted. Patients were placed in either single-chamber (n = 27), dual-chamber (n = 90), or biventricular/CRT groups (n = 37). Of the patients undergoing a single-chamber device implantation, 23 had mild TR and four had moderate TR at baseline. Of the patient undergoing dual-chamber device implantation, 81 had mild TR and nine had moderate TR at baseline. Of the patients undergoing CRT device implantation, 28 had mild TR, eight had moderate TR, and one had severe TR at baseline (Table 2).
 Click to view | Table 1. Baseline Characteristics of Patients |
 Click to view | Table 2. Baseline Tricuspid Regurgitation |
The mean age of our study population was 71. Eighty-five (55%) were male and 69 (45%) were female. The average pre and post LVEF in the CRT, single-chamber, and dual-chamber groups were 33.5% and 46.5%, 45.5% and 49.2%, and 51.2% and 50.6% respectively. The average pre and post RVSP in the CRT, single-chamber, and dual-chamber groups were 31.8 mm Hg and 40.5 mm Hg, 34.6 mm Hg and 46.4 mm Hg, and 35.7 mm Hg and 39.0 mm Hg respectively.
There was no statistically significant change in TR severity following CRT implantation with similar degrees of TR in both the pre- and post-implantation groups (Fig. 1). However, in both the single-chamber and dual-chamber groups, statistically significant change in TR severity was noted following device implantation. In both the single- and dual-chamber device group there was significantly more patients with moderate and severe TR post-implantation (Figs. 2, 3). Also, patients with mild TR at baseline were more impacted than those with moderate TR in the single- and dual-chamber device groups. Patients that underwent CRT implantation had a significantly lower risk of worsening TR, from baseline, of 16.2% when compared to single-chamber (37.04%) and dual-chamber (30%) (Fig. 4).
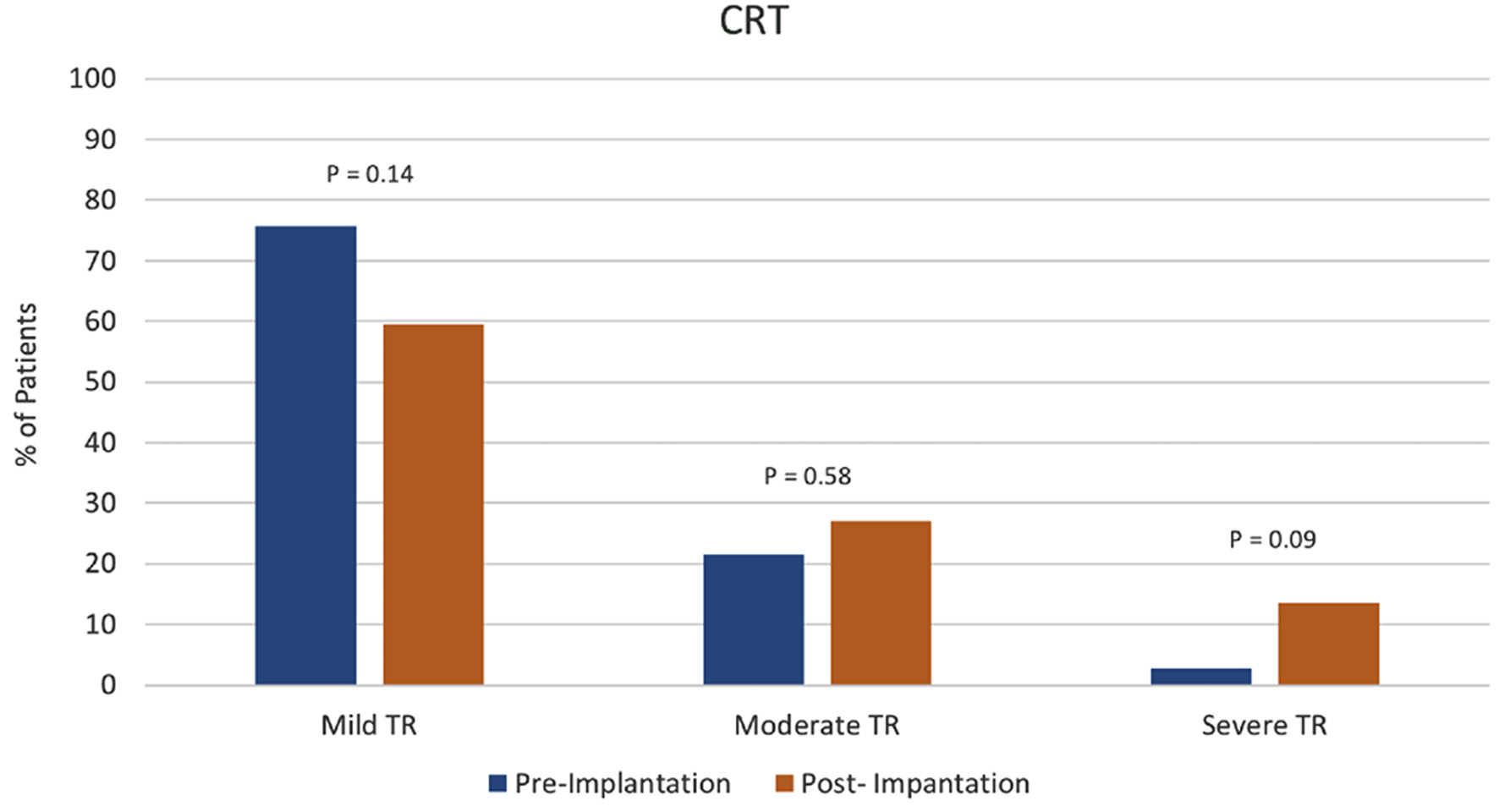 Click for large image | Figure 1. Cardiac resynchronization therapy (CRT) group tricuspid regurgitation (TR) severity pre- vs. post-device implantation. |
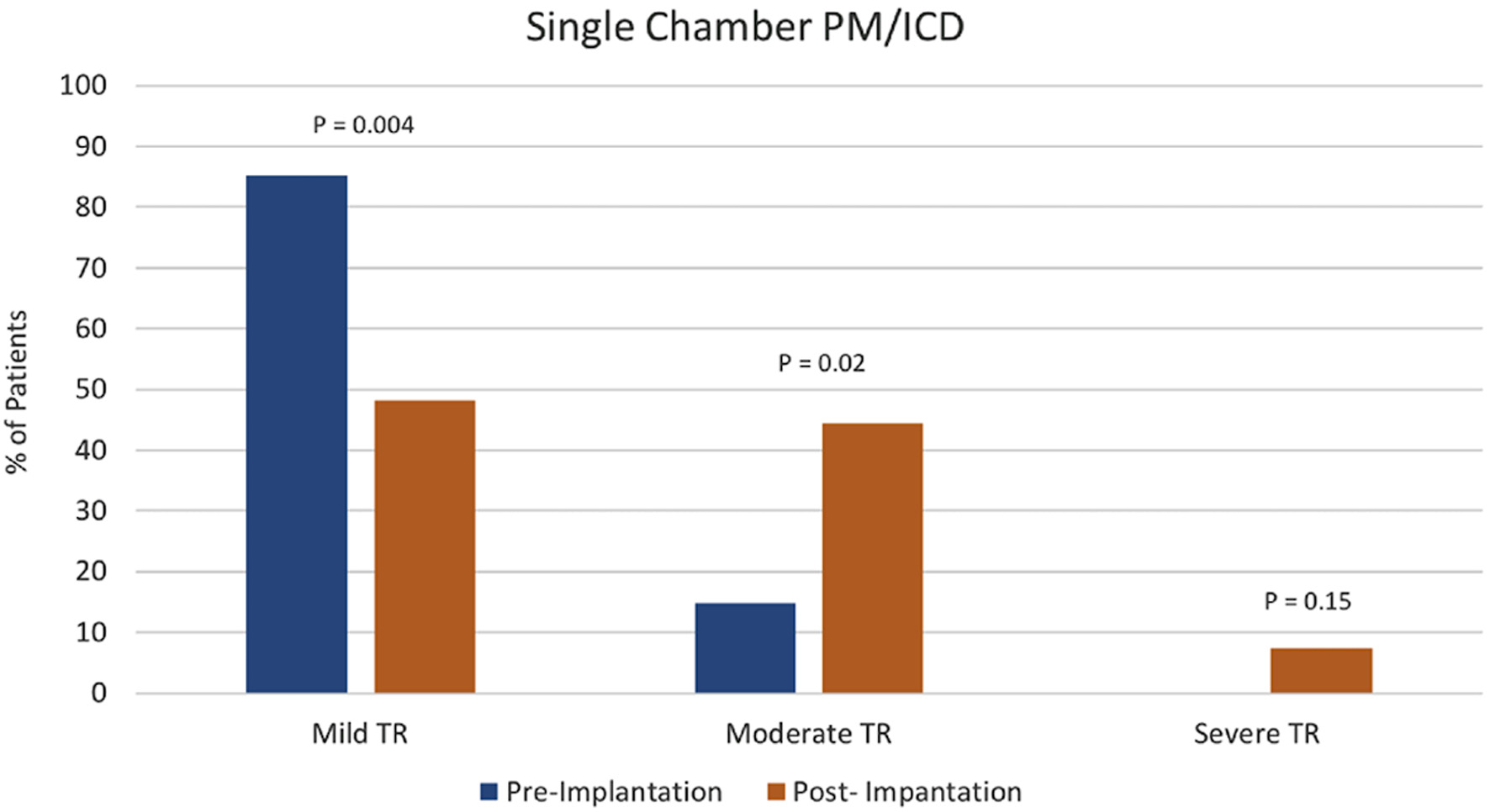 Click for large image | Figure 2. Single-chamber pacemaker (PM) or implantable cardioverter-defibrillator (ICD) group tricuspid regurgitation (TR) severity pre-device vs. post-device implantation. |
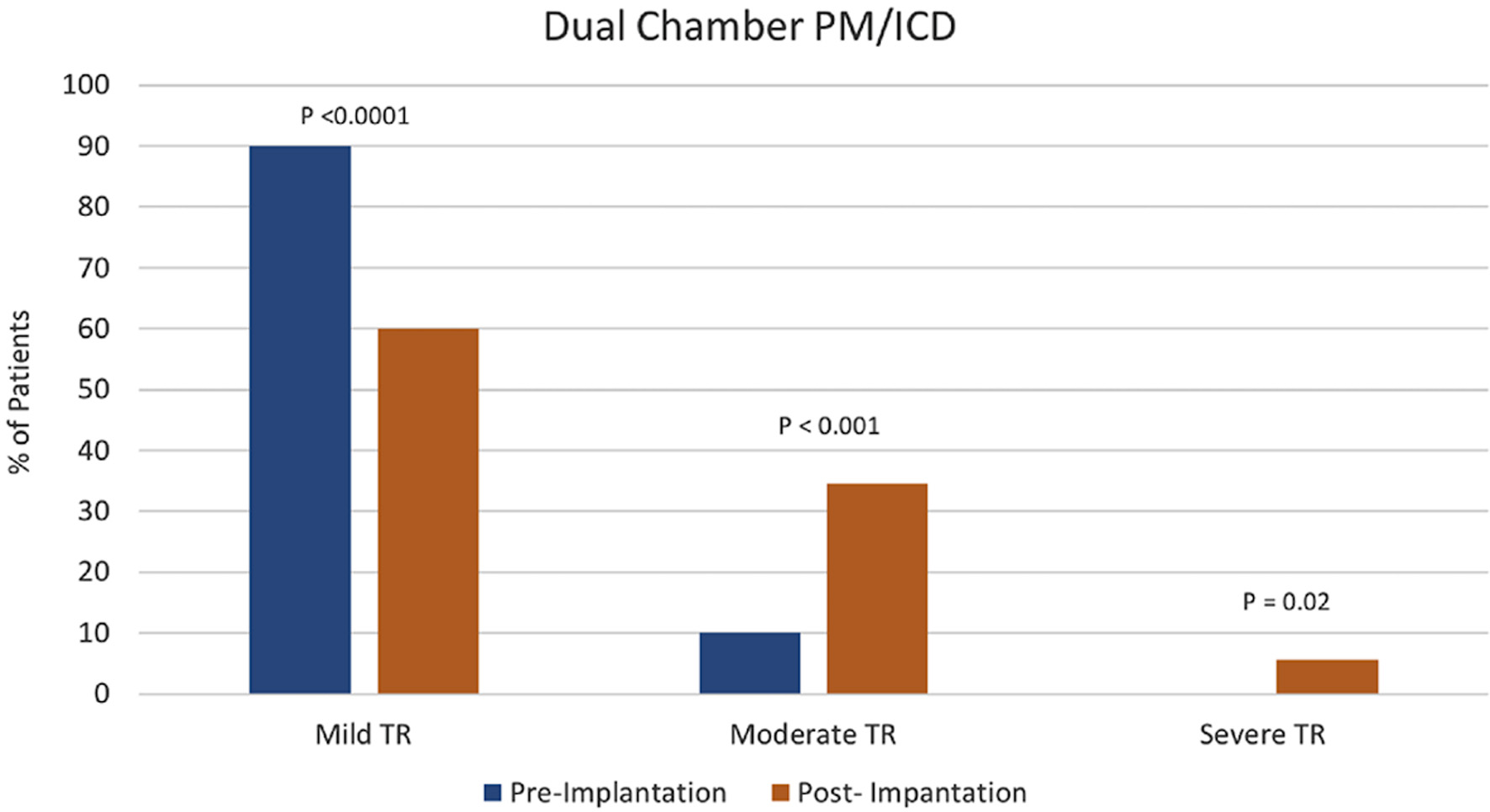 Click for large image | Figure 3. Dual-chamber pacemaker (PM) or implantable cardioverter-defibrillator (ICD) group tricuspid regurgitation (TR) severity pre-device vs. post-device implantation. |
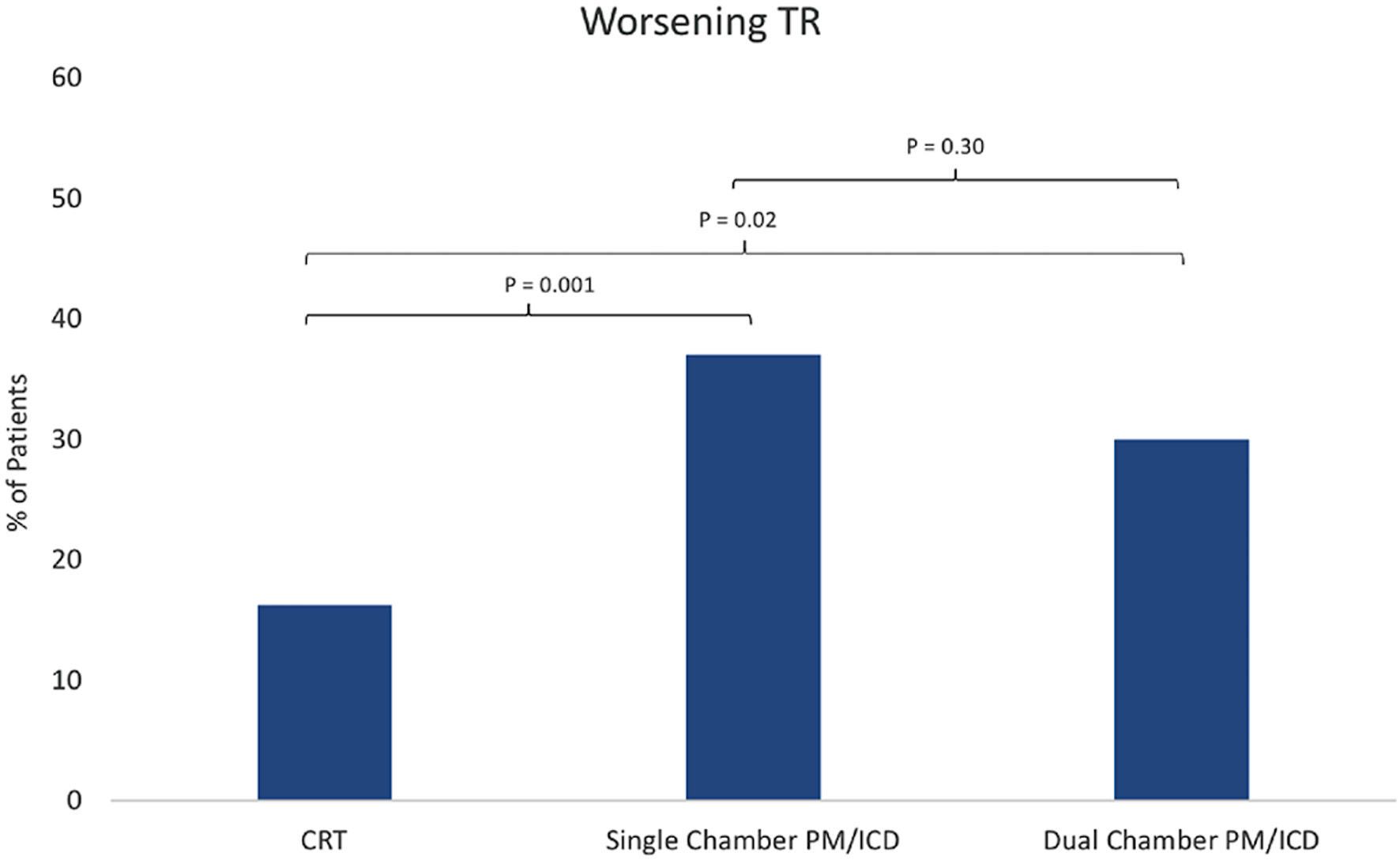 Click for large image | Figure 4. Comparison of worsening tricuspid regurgitation (TR) between the three groups: 1) cardiac resynchronization therapy (CRT); 2) single-chamber pacemaker (PM) or implantable cardioverter-defibrillator (ICD); and 3) dual-chamber PM or ICD. |
| Discussion | ▴Top |
In this single-center retrospective study we sought to determine if COPD patients with CRT devices had less CIED-mediated TR compared to COPD patients with non-CRT devices. In our cohort of 154 patients with COPD, we found that patients with CRT devices had a significantly lower risk of worsening TR when compared to single-chamber and dual-chamber PPM and ICD devices. There was no statistically significant change in the degree of TR in patients who underwent CRT implantation. Patients that underwent single- and dual-chamber device implantation had a statistically significant increase in TR severity. These findings suggest that not only does the presence of the right ventricle lead traversing the tricuspid valve increase and/or worsen TR but right ventricle pacing is a contributing factor.
The negative impact of moderate to severe TR on long-term survival has been well described in the literature [4, 5]. In a recent analysis of patients with heart failure with reduced ejection fraction, TR was independently associated with PH, more severe heart failure presentations, and worse survival [22]. Compared to non-CIED-mediated TR, patients with CIED-mediated TR have been found to have similar or worse outcomes [9-12, 23]. These findings have been observed even after adjusting for left-sided heart disease and PH [24]. Single- and dual-chamber PPM and ICD devices are associated with CIED-induced TR, given that both devices have leads that cross the tricuspid valve into the right ventricle. Some studies have concluded that ICD devices are more commonly associated with CIED-mediated TR, when compared to PPM devices due to the greater diameter and thickness of their leads [8, 12]. However, other studies have reported no significant difference between PPM and ICD devices regarding CIED-mediated TR. In comparison to PPM and ICD device-related TR, the current literature for CRT device-mediated TR is inconsistent.
Significant improvements in right ventricle function and pulmonary pressure have been observed following the placement of CRT devices [17, 18, 25]. Additionally, the initiation of CRT has also been shown to improve MR caused by right ventricle pacing-induced ventricular dyssynchrony [19, 26]. Theoretically, an improvement in TR following the placement of a CRT device could be expected, given its positive effects on the right ventricle, LV, and mitral valve as well as a reduction in pulmonary pressure. This theory would be further supported if a component of CIED-mediated TR is in fact due to right ventricle pacing and ventricular dyssynchrony. In patients with severe heart failure, improvement of LV function and thus a reduction of pulmonary congestion with CRT, could potentially reduce elevated right-sided heart pressures and TR. Unfortunately, the current literature has not consistently supported this hypothesis. Grupper et al evaluated CIED-mediated TR and worsening baseline TR after implantation of CRT devices [20]. They concluded that patients who had worsening TR following CRT placement had worse clinical and echocardiographic response but were not associated with an increase in mortality [20]. However, the opposite was found for patients with baseline TR, in that they had a reduced survival despite better clinical and echocardiographic response following CRT device implantation [20]. Abu Sham’a et al reported similar outcomes in patients with baseline TR following CRT device placement [7]. These findings could suggest that any device lead that passes through the tricuspid valve has the potential to worsen TR and thus a patient’s response to CRT. However, while it is well known that patients with preexisting moderate to severe TR have poorer outcomes, they clinically benefit from CRT therapy [7, 20]. Not all previous studies investigating CRT and CIED-induced TR have reported similar findings. Arabi et al found no difference in CIED-mediated TR between patients with CRT devices and patients with PPM or ICD devices [21]. Furthermore, Sadreddini et al concluded that patients did not have an increase in TR following the implantation of a CRT device [27]. Given the discrepancies amongst these studies, there are no clear management guidelines or indications for CRT in CIED-mediated TR.
Conditions that adversely affect the right ventricle and predisposed patients to TR, such as COPD, can be associated with worse outcomes for both CIED and non-CIED related TR. Chronic lung disease has been shown to have many negative effects on the structure and the function of the right heart [28]. Studies have shown that patients with heart failure and COPD are at higher risk for lethal arrythmias and thus, have a higher incidence of ICD defibrillations compared to patients without COPD [29]. Few studies have investigated CIED-mediated TR in patients with COPD; and to our knowledge, no studies have specifically looked at the effects of CRT on TR in COPD patients. In a retrospective analysis of 164 patients undergoing CRT implantation, Kirubakaran and colleagues concluded that COPD was a predictor for lack of clinical response to CRT [30]. However, there are likely multiple confounding factors that need to be considered in this patient population including medication tolerability as well as multifactorial dyspnea [30]. Gazzoni et al concluded that age, COPD, and prior myocardial infarctions were independent predictors for total mortality in patients receiving CRT devices [31]. This finding is likely related to the effects of comorbid conditions on overall heart failure outcomes and mortality [31].
CRT has been shown to provide ventricular synchrony as well as improvement of left and right ventricle function. Based on the findings of this study and the associations between COPD, PH, right ventricle failure, and baseline TR, CRT devices can reduce the risk of TR progression compared to single-chamber and dual-chamber devices. This risk reduction is especially important for patients at high risk for right-sided heart abnormalities, such as those with COPD. However, while LVEF improved with CRT device placement and TR progression was reduced, there was an unexpected increase in post-implantation RSVP in patients with COPD. This increase in RSVP suggests that there was no reduction in pulmonary pressures following the implantation of CRT devices.
Since both COPD and the progression of TR have been shown to have poor outcomes, it may be reasonable for providers to consider an upfront strategy of CRT over single- or dual-chamber devices in patients with COPD, especially in those with preexisting TR. We feel that prospective randomized studies are needed to further assess the benefits of CRT in COPD patients and its effects of both CIED and non-CIED mediated TR.
Limitations
The main limitations of our study include a small sample size at a single medical center and performing the study in a retrospective manner. TR presence and severity was diagnosed via TTE, and confirmatory transesophageal echocardiograms were not performed. Another limitation to our study is that the diagnosis of COPD was made by ICD-10 codes and severity was not determined.
Conclusions
Patients with COPD receiving a CRT device were less likely to have worsening TR, compared to single-chamber and dual-chamber devices. Since both COPD and progression of TR may result in poor outcomes, our study suggests that an upfront strategy with CRT rather than a single- or dual-chamber device in this patient population, especially with pre-existent TR.
Acknowledgments
None to declare.
Financial Disclosure
None to declare.
Conflict of Interest
The authors report no conflict of interest regarding the content herein.
Informed Consent
Study was exempt given the retrospective nature.
Author Contributions
James Livesay and Raj Baljepally conceived and designed the study, performed data collection, and wrote the manuscript. Benjamin Fogelson performed data collection and wrote the manuscript. Hassan Tahir performed the statistical analysis and helped in writing the methods and results section of the manuscript.
Data Availability
The data supporting these findings of this study are available from the corresponding author upon reasonable request.
| References | ▴Top |
- Cuttica MJ, Shah SJ, Rosenberg SR, Orr R, Beussink L, Dematte JE, Smith LJ, et al. Right heart structural changes are independently associated with exercise capacity in non-severe COPD. PLoS One. 2011;6(12):e29069.
doi pubmed - Schoos MM, Dalsgaard M, Kjaergaard J, Moesby D, Jensen SG, Steffensen I, Iversen KK. Echocardiographic predictors of exercise capacity and mortality in chronic obstructive pulmonary disease. BMC Cardiovasc Disord. 2013;13:84.
doi pubmed - Wang N, Fulcher J, Abeysuriya N, McGrady M, Wilcox I, Celermajer D, Lal S. Tricuspid regurgitation is associated with increased mortality independent of pulmonary pressures and right heart failure: a systematic review and meta-analysis. Eur Heart J. 2019;40(5):476-484.
doi pubmed - Nath J, Foster E, Heidenreich PA. Impact of tricuspid regurgitation on long-term survival. J Am Coll Cardiol. 2004;43(3):405-409.
doi pubmed - Topilsky Y, Maltais S, Medina Inojosa J, Oguz D, Michelena H, Maalouf J, Mahoney DW, et al. Burden of tricuspid regurgitation in patients diagnosed in the community setting. JACC Cardiovasc Imaging. 2019;12(3):433-442.
doi pubmed - Zhang XX, Wei M, Xiang R, Lu YM, Zhang L, Li YD, Zhang JH, et al. Incidence, risk factors, and prognosis of tricuspid regurgitation after cardiac implantable electronic device implantation: a systematic review and meta-analysis. J Cardiothorac Vasc Anesth. 2022;36(6):1741-1755.
doi pubmed - Abu Sham'a R, Buber J, Grupper A, Nof E, Kuperstein R, Luria D, Feinberg MS, et al. Effects of tricuspid valve regurgitation on clinical and echocardiographic outcome in patients with cardiac resynchronization therapy. Europace. 2013;15(2):266-272.
doi pubmed - Addetia K, Harb SC, Hahn RT, Kapadia S, Lang RM. Cardiac Implantable Electronic Device Lead-Induced Tricuspid Regurgitation. JACC Cardiovasc Imaging. 2019;12(4):622-636.
doi pubmed - Al-Bawardy R, Krishnaswamy A, Rajeswaran J, Bhargava M, Wazni O, Wilkoff B, Tuzcu EM, et al. Tricuspid regurgitation and implantable devices. Pacing Clin Electrophysiol. 2015;38(2):259-266.
doi pubmed - Al-Mohaissen MA, Chan KL. Prevalence and mechanism of tricuspid regurgitation following implantation of endocardial leads for pacemaker or cardioverter-defibrillator. J Am Soc Echocardiogr. 2012;25(3):245-252.
doi pubmed - Ebrille E, Chang JD, Zimetbaum PJ. Tricuspid Valve Dysfunction Caused by Right Ventricular Leads. Card Electrophysiol Clin. 2018;10(3):447-452.
doi pubmed - Kim JB, Spevack DM, Tunick PA, Bullinga JR, Kronzon I, Chinitz LA, Reynolds HR. The effect of transvenous pacemaker and implantable cardioverter defibrillator lead placement on tricuspid valve function: an observational study. J Am Soc Echocardiogr. 2008;21(3):284-287.
doi pubmed - Lin G, Nishimura RA, Connolly HM, Dearani JA, Sundt TM, 3rd, Hayes DL. Severe symptomatic tricuspid valve regurgitation due to permanent pacemaker or implantable cardioverter-defibrillator leads. J Am Coll Cardiol. 2005;45(10):1672-1675.
doi pubmed - Trankle CR, Gertz ZM, Koneru JN, Kasirajan V, Nicolato P, Bhardwaj HL, Ellenbogen KA, et al. Severe tricuspid regurgitation due to interactions with right ventricular permanent pacemaker or defibrillator leads. Pacing Clin Electrophysiol. 2018;41(7):845-853.
doi pubmed - Moss AJ, Hall WJ, Cannom DS, Klein H, Brown MW, Daubert JP, Estes NA, 3rd, et al. Cardiac-resynchronization therapy for the prevention of heart-failure events. N Engl J Med. 2009;361(14):1329-1338.
doi pubmed - Young JB, Abraham WT, Smith AL, Leon AR, Lieberman R, Wilkoff B, Canby RC, et al. Combined cardiac resynchronization and implantable cardioversion defibrillation in advanced chronic heart failure: the MIRACLE ICD Trial. JAMA. 2003;289(20):2685-2694.
doi pubmed - Kusiak A, Wilinski J, Wojciechowska W, Jastrzebski M, Sondej T, Bacior B, Kloch-Badelek M, et al. Effects of biventricular pacing on right ventricular function assessed by standard echocardiography. Kardiol Pol. 2012;70(9):883-888.
- Praus R, Haman L, Tauchman M, Pudil R, Blaha V, Parizek P. Echocardiographic changes after cardiac resynchronisation therapy. Kardiol Pol. 2012;70(12):1250-1257.
- Fanari Z, Hammami S, Hammami MB, Hammami S, Shuraih M. The effects of right ventricular apical pacing with transvenous pacemaker and implantable cardioverter defibrillator on mitral and tricuspid regurgitation. J Electrocardiol. 2015;48(5):791-797.
doi pubmed - Grupper A, Killu AM, Friedman PA, Abu Sham'a R, Buber J, Kuperstein R, Rozen G, et al. Effects of tricuspid valve regurgitation on outcome in patients with cardiac resynchronization therapy. Am J Cardiol. 2015;115(6):783-789.
doi pubmed - Arabi P, Ozer N, Ates AH, Yorgun H, Oto A, Aytemir K. Effects of pacemaker and implantable cardioverter defibrillator electrodes on tricuspid regurgitation and right sided heart functions. Cardiol J. 2015;22(6):637-644.
doi pubmed - Benfari G, Antoine C, Miller WL, Thapa P, Topilsky Y, Rossi A, Michelena HI, et al. Excess mortality associated with functional tricuspid regurgitation complicating heart failure with reduced ejection fraction. Circulation. 2019;140(3):196-206.
doi pubmed - Hoke U, Auger D, Thijssen J, Wolterbeek R, van der Velde ET, Holman ER, Schalij MJ, et al. Significant lead-induced tricuspid regurgitation is associated with poor prognosis at long-term follow-up. Heart. 2014;100(12):960-968.
doi pubmed - Delling FN, Hassan ZK, Piatkowski G, Tsao CW, Rajabali A, Markson LJ, Zimetbaum PJ, et al. Tricuspid regurgitation and mortality in patients with transvenous permanent pacemaker leads. Am J Cardiol. 2016;117(6):988-992.
doi pubmed - Martens P, Verbrugge FH, Bertrand PB, Verhaert D, Vandervoort P, Dupont M, Tang WHW, et al. Effect of cardiac resynchronization therapy on exercise-induced pulmonary hypertension and right ventricular-arterial coupling. Circ Cardiovasc Imaging. 2018;11(9):e007813.
doi pubmed - Dilaveris P, Pantazis A, Giannopoulos G, Synetos A, Gialafos J, Stefanadis C. Upgrade to biventricular pacing in patients with pacing-induced heart failure: can resynchronization do the trick? Europace. 2006;8(5):352-357.
doi pubmed - Sadreddini M, Haroun MJ, Buikema L, Morillo C, Ribas S, Divakaramenon S, Connolly SJ, et al. Tricuspid valve regurgitation following temporary or permanent endocardial lead insertion, and the impact of cardiac resynchronization therapy. Open Cardiovasc Med J. 2014;8:113-120.
doi pubmed - Gupta NK, Agrawal RK, Srivastav AB, Ved ML. Echocardiographic evaluation of heart in chronic obstructive pulmonary disease patient and its co-relation with the severity of disease. Lung India. 2011;28(2):105-109.
doi pubmed - Naksuk N, Kunisaki KM, Benditt DG, Tholakanahalli V, Adabag S. Implantable cardioverter-defibrillators in patients with COPD. Chest. 2013;144(3):778-783.
doi pubmed - Kirubakaran S, Ladwiniec A, Arujuna A, Ginks M, McPhail M, Bostock J, Carr-White G, et al. Male gender and chronic obstructive pulmonary disease predict a poor clinical response in patients undergoing cardiac resynchronisation therapy. Int J Clin Pract. 2011;65(3):281-288.
doi pubmed - Gazzoni GF, Fraga MB, Ferrari ADL, Soliz PDC, Borges AP, Bartholomay E, Kalil CAA, et al. Predictors of total mortality and echocardiographic response for cardiac resynchronization therapy: a cohort study. Arq Bras Cardiol. 2017;109(6):569-578.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cardiology Research is published by Elmer Press Inc.


