| Cardiology Research, ISSN 1923-2829 print, 1923-2837 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, Cardiol Res and Elmer Press Inc |
| Journal website https://www.cardiologyres.org |
Original Article
Volume 12, Number 3, June 2021, pages 156-160
Review of Referrals Sent to the Emergency Department for Management of Hypertension
Andre Emmanuel Richarda, c, Marie-Helene Chomienneb
aDepartment of Family Medicine, University of Ottawa, 713 Montreal Road, Ottawa, ON H2Z OA2, Canada
bDepartment of Family Medicine, University of Ottawa, 713 Montreal Road, Ottawa, ON K1K 0T2, Canda
cCorresponding Author: Andre Emmanuel Richard, Department of Family Medicine, University of Ottawa, 713 Montreal Road, Ottawa, ON H2Z OA2, Canada
Manuscript submitted February 23, 2021, accepted March 9, 2021, published online May 14, 2021
Short title: Referrals for Hypertensive Emergencies
doi: https://doi.org/10.14740/cr1233
| Abstract | ▴Top |
Background: Hypertensive urgencies, unlike hypertensive emergencies, are severe episodes of hypertension without evidence of end-organ damage. Most recent guidelines advise against referring patients with hypertensive urgencies to the emergency department (ED) for treatment. There is a lack of Canadian data surrounding whether referrals to the ED regarding hypertension are appropriate. We analyzed referrals to the Montfort Hospital ED due to hypertension and assessed if they met the criteria for hypertensive emergencies.
Methods: This was a retrospective chart study of all ED visits at Montfort Hospital from the 2016 fiscal year with a final diagnosis/chief complaint of hypertension. Charts were assessed to determine if these patients met the criteria for having true hypertensive emergencies.
Results: Out of the 54,000 visits to the Montfort ED, 254 reported hypertension as a final diagnosis/chief complaint. Of those, 67 patients had been referred by a healthcare practitioner, while 187 were self-referred. None of the referred patients met the criteria for hypertensive emergency; however, eight of these patients did have symptoms indicating a possibility of hypertensive emergency. Six of the self-referred patients met criteria for hypertensive emergency. The majority (71.6%) of patients referred did not require on-site antihypertensive treatment, and 37.3% of patients were sent home with new outpatient prescriptions.
Conclusion: All the cases referred to the Montfort ED for hypertension were considered hypertensive urgencies and none of them required ED hypertensive treatment. Further investigation is required to help optimize appropriate patient referral to the ED for true hypertensive emergencies and improve management of hypertensive urgencies in the community.
Keywords: Hypertension; Hypertensive urgency; Hypertensive emergency; Referral
| Introduction | ▴Top |
Hypertension is an ubiquitous disease and the lifetime incidence of developing high blood pressure is estimated to be 90% for Canadians [1]. Untreated, chronically elevated blood pressure drastically increases a patient’s risk for adverse cardiovascular events (e.g. stroke, myocardial infarction). While the number of visits to the emergency department (ED) for this condition is high (approximately 2.1%), only two in 1,000 adult ED visits overall qualify as true hypertensive emergencies [2] (blood pressure > 180/120 mm Hg, with impending or progressive end-organ damage) [3]. In Ottawa, Ontario, the Montfort Hospital, an urban community hospital that sees approximately 54,000 patients per year [4], the number of visits for hypertension more than doubled between 2003 and 2018 [5].
For hypertensive urgencies (asymptomatic blood pressure > 180/120 mm Hg, or diastolic blood pressure > 130 mm Hg, with no impending or progressive end-organ damage) [3], it is recommended that patients optimize their oral antihypertensive regimen with appropriate follow-up care, rather than with aggressive treatment through transfer to an acute care facility [6]. Despite those recommendations, many patients with hypertensive urgencies are referred to already overcrowded emergency rooms for unrequired acute care [7]. There is currently a lack of specific data from Canadian institutions regarding the incidence of true hypertensive emergencies.
This paper offers a cross-sectional assessment of ED visits to the Montfort Hospital relating to hypertension to determine the proportion of referrals meeting criteria for hypertensive emergencies and explores the differences between referred and self-referred patients.
| Materials and Methods | ▴Top |
The study population was limited to patients above 18 years of age presenting to the ED for reasons regarding uncontrolled hypertension from April 2016 to March 2017. We identified 254 visits with a diagnosis of hypertension, from which there were 237 unique patients (Fig. 1).
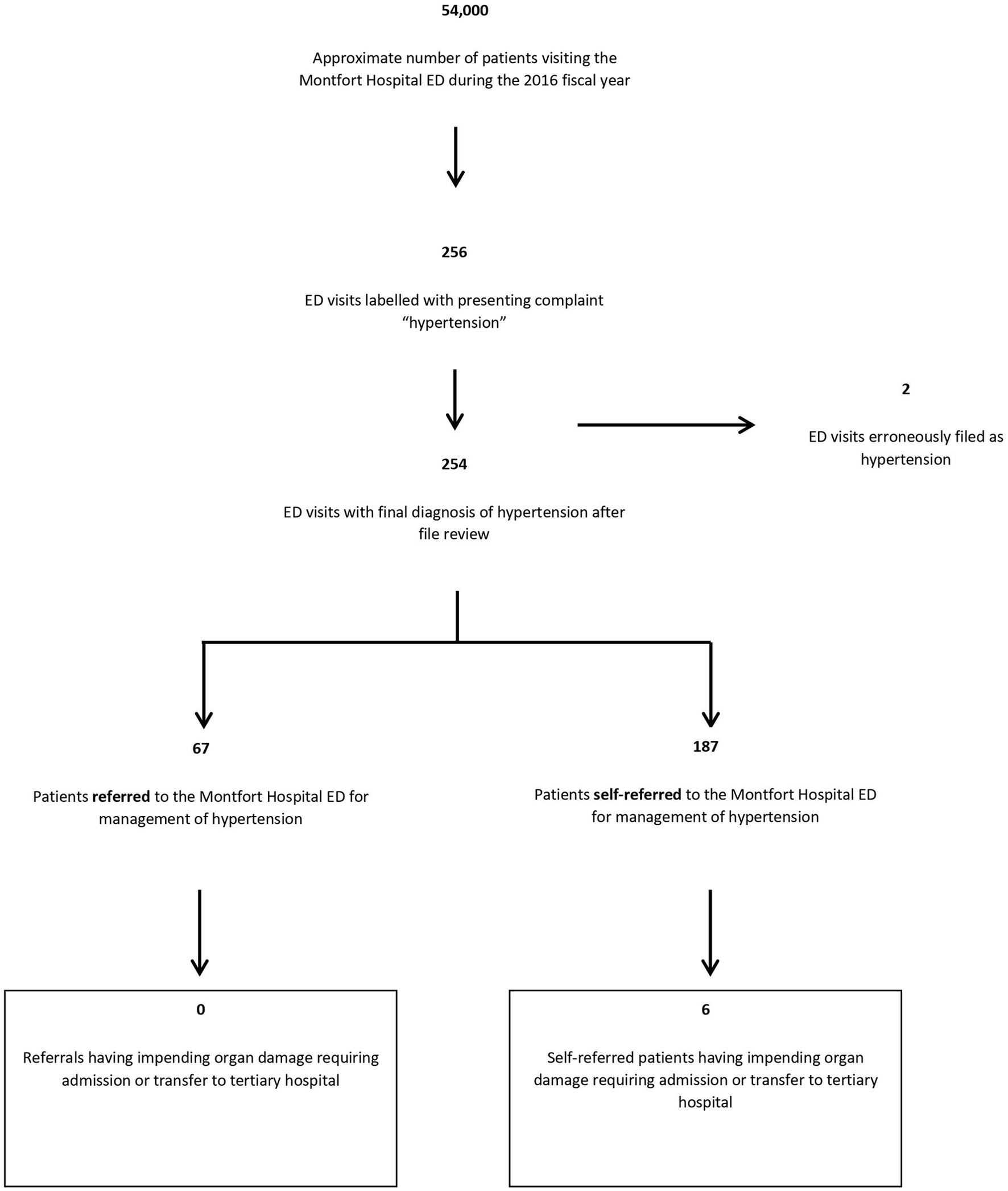 Click for large image | Figure 1. Study population. Acute target end-organ damage was defined as heart failure, myocardial infarction, stroke, increased ICP, hypertensive encephalopathy, ruptured major vessel, intracerebral hemorrhage, transient cerebral ischemia, or retinal hemorrhage. Overall patient volume per year was taken from the Montfort emergency room website [3]. ICP: intracranial pressure. |
Patients’ records were anonymized by the Montfort Hospital Medical Records Department and given a research number, which was encrypted into the hospital’s electronic medical record (EMR) on site. Data collection utilized patient documentation (e.g. triage sheets and MD notes). Sex, age, mode of arrival, referred/self-referred, wait times, symptoms, treatment received in ED or prescribed at discharge were collected. Additional variables collected included the Canadian Triage and Acuity Scale (CTAS) score, whether a consultation or admission was required, and whether a summary note was sent to the patient’s family doctor (if applicable).
We considered ED visits as hypertensive emergencies if the patient had a diagnosis of hypertension, a diagnostic criterion for target end-organ damage, and/or definitive management in terms of disposition (required admission to hospital, transfer to another hospital, or death).
Acute target end-organ damage was defined as heart failure, myocardial infarction, stroke, increased intracranial pressure (ICP), hypertensive encephalopathy, ruptured major vessel, intracerebral hemorrhage, transient cerebral ischemia, or retinal hemorrhage.
We compared referred and self-referred groups using statistical testing with Student’s t-test and Chi-square analysis and frequency analysis. Subgroup analysis was performed to determine which visits qualified as hypertensive emergencies. Analysis was performed with SPSS version 25, with P-values under 0.05 considered statistically significant.
The Montfort Hospital Research Ethics Board (file number 18-19-01-040) approved this study. This study was conducted in compliance with the ethical standards of the responsible institution on human subjects as well as with the Helsinki Declaration.
| Results | ▴Top |
Of the 254 ED visits regarding hypertension, 67 were referred to the ED by a physician or allied health professional. No patients referred to the ED exhibited signs of end-organ damage, and all were accordingly discharged from hospital after assessment. Of the 187 self-referred patients, six showed evidence of end-organ damage and required admission or transfer to another institution. Three patients had evidence of stroke, one of encephalopathy and two demonstrated acute pulmonary edema and/or congestive heart failure from uncontrolled hypertension. A comparison between the demographics and vitals at time of admission of the self-referred and referred patients is shown in Table 1. The majority of referred patients, when including walk-in clinics and urgent care visits, were referred by a family physician (41.8%, n = 28), followed by retirement/nursing homes (20.9%, n = 14) and pharmacists (22.4%, n = 15). The remaining referrals (14.9%, n = 10) came from other sources (e.g. specialists, telehealth services, etc.).
 Click to view | Table 1. Demographic Information, Triage Summary and Visit Overview Statistics for Patients Presenting to the Montfort ED Regarding Hypertension During the 2016 Fiscal Year |
A larger proportion of referred patients (37.3%) presented to the ED without symptoms when compared to the self-referred group (16%) (Table 2); however, this difference was not significant (P = 0.50). Report of symptoms was significantly higher in the self-referred population, with a higher proportion of patients presenting with acute symptoms such as chest pains (13.4% versus 6.0%, P = 0.001) or headaches (44.9% versus 37.3%, P < 0.001).
 Click to view | Table 2. Presenting Complaints for Patients Referred to the Montfort ED Regarding Hypertension During the Fiscal Year of 2016 |
Over a quarter (26%) of patients received antihypertensive medication during their ED stay; 68.7% (n = 46) of referred patients and 76.5% (n = 143) of self-referred patients received no treatment in ED (Table 1). The patients who were referred were sent home with outpatient prescriptions for an antihypertensive 42.4% (n = 28) of the time, and those self-referred received prescriptions 35.8% (n = 67) of the time, with no significant differences between groups.
Of the 254 visits, 86.6% (n = 220) of cases involved individuals with a family doctor (self-referred patients: n = 161, 86.1%; referred patients: n = 59, 88.1%). After the ED visit , 42.4% (n = 25) of the referred patients had an after-visit summary sheet sent back to their family physician. Of the 17 patients sent directly to the ED by a family physician, only 29.4% (n = 5) had an after-visit summary sent back. The self-referred group saw 18.0% (n = 29) of their patients having after-visit summaries sent. There was no significant difference between the groups.
| Discussion | ▴Top |
During the 2016 fiscal year, the Montfort Hospital ED recorded six hypertensive emergencies, all of which were self-referred patients and not patients referred by a health professional. This converts to an estimated incidence for hypertensive emergencies of one in 9,000 patient-visits per year - a figure vastly lower than American studies estimating the incidence of hypertensive emergencies at two in 1,000 [2]. Hypertensive urgencies and other hypertension cases account for a much higher proportion of the Montfort Hospital’s hypertension-related ED visits (one in every 218 patient-visits per year). This is much smaller relative to incidences reported in the literature (e.g. one study found that 25.7% of ED visits were hypertension-related emergencies) [8]. Differences between the findings here and the literature could be due to the data collection method in this study, i.e. a single hospital over a single fiscal year. Most patients presenting to the ED for hypertension were self-referred; also these patients were more symptomatic (Table 2), suggesting that they by-passed primary care providers and directly went to the ED. It is important to note that there was a significant increase in the number of patients with symptoms indicating possible end-organ damage (Table 2), including chest pain, facial droop and other neurological symptoms. For these patients, a prompt visit to the ED was completely appropriate for emergent diagnostic workup. For the remainder of the self-referred group, the higher proportion of ED visits may have been due to physicians in the community being unable to offer same-day visits or telephone consultations.
Both referred and self-referred groups received similar treatments while in the ED. The majority of patients did not require any antihypertensives (even with higher-than-average blood pressure) throughout their stay in the ED, and most were sent home without any outpatient prescriptions. This supports that: 1) these cases could be managed in the community; and 2) these ED visits do not significantly benefit the patients and mirror a recent study where only 0.7% of patients required ongoing care and/or referral [9]. Finally, the ED feedback by emergency physicians was found to be inconsistent, with a minority of patients having an after-visit summary sent to the family doctor (the majority of patients in both groups had a family doctor) explaining their course through the ED. The lack of feedback to the referring physicians may contribute to the perpetuation of these patients’ mismanagement, as they could be a mode of knowledge transfer to the community physician.
Limitations of this study include a small sample size. Additionally, due to using one single site, results may not be generalizable to ED visits across Ontario. Additional limitations include the utilization of EMRs for analyses, as it is possible that the number of true hypertensive emergencies was underestimated due to differences in coding or reporting of the most responsible diagnosis (e.g. labelled as acute myocardial infarction). Additional confounds include the variability between referral sources and standards of care among emergency room physicians.
Overall, most patients visiting the ED due to hypertension did not qualify as having a hypertensive emergency, as such, a significant number of patients did not require acute care. Future work should examine how to best inform referring physicians to better manage hypertensive urgencies; timely feedback to primary care physicians upon discharge including a summary of the criteria for hypertension emergencies versus. hypertensive urgencies and treatment guidelines may prove an efficient approach to providing education and guidance to these practitioners for future cases. We would suggest that referring physicians base their decision to send a patient to the ED on symptoms that indicate end-organ damage, rather than arbitrary blood pressure measurements, and to educate their patients about when to seek emergent care. We must also emphasize that clinical judgement should remain paramount and that if the physician is concerned, a referral to an acute care facility should be considered. Finally, physicians may consider handing out clearly structured follow-up and referral guidelines to patients after a diagnosis of hypertension in order to empower self-care.
Acknowledgments
The authors wish to thank the Institut du Savoir Montfort for assisting in gathering patient data and with study designs, Joseph Abdulnour for assistance with data analysis, and Jessika Hammond for assistance with the editing of the manuscript.
Financial Disclosure
None to declare.
Conflict of Interest
None to declare.
Informed Consent
Not applicable.
Author Contributions
AR conceptualized and designed the study, conducted the data analyses and wrote the final manuscript. JA assisted with the data analyses. JH assisted with writing the final manuscript. MC assisted in conceptualizing the study, conducted the data analyses, and writing the final manuscript.
Data Availability
The data supporting the findings of this study are available from the corresponding author upon reasonable request.
| References | ▴Top |
- Leung AA, Bushnik T, Hennessy D, McAlister FA, Manuel DG. Risk factors for hypertension in Canada. Health Rep. 2019;30(2):3-13.
- Janke AT, McNaughton CD, Brody AM, Welch RD, Levy PD. Trends in the incidence of hypertensive emergencies in US emergency departments from 2006 to 2013. J Am Heart Assoc. 2016;5(12):e004511.
doi pubmed - Rabi DM, McBrien KA, Sapir-Pichhadze R, Nakhla M, Ahmed SB, Dumanski SM, Butalia S, et al. Hypertension Canada's 2020 comprehensive guidelines for the prevention, diagnosis, risk assessment, and treatment of hypertension in adults and children. Can J Cardiol. 2020;36(5):596-624.
doi pubmed - Hopital Montfort. Hopital Montfort. [Internet]. Ottawa: Hopital Montfort; 2019 [cited Dec 17, 2019]. Available from: https://hopitalmontfort.com/en/emergency.
- Data provided by the Institut de Savoir Montfort regarding patients receiving primary diagnosis of hypertension during emergency department visits from 2003 to 2018. [cited June 10, 2019].
- Hackett C, Garrison S, Kolber MR. What is urgent about hypertensive urgency? Can Fam Physician. 2017;63(7):543.
- Health Quality Ontario. Under pressure: Emergency department performance in Ontario. [Internet] Toronto: Health Quality Ontario; 2016 [cited Dec 17, 2019]. p.46. Available from: http://www.hqontario.ca/Portals/0/documents/system-performance/under-pressure-report-en.pdf.
- McNaughton CD, Self WH, Zhu Y, Janke AT, Storrow AB, Levy P. Incidence of hypertension-related emergency department visits in the United States, 2006 to 2012. Am J Cardiol. 2015;116(11):1717-1723.
doi pubmed - Heath I. Hypertensive urgency-is this a useful diagnosis? JAMA Intern Med. 2016;176(7):988-989.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cardiology Research is published by Elmer Press Inc.


