| Cardiology Research, ISSN 1923-2829 print, 1923-2837 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, Cardiol Res and Elmer Press Inc |
| Journal website http://www.cardiologyres.org |
Case Report
Volume 10, Number 5, October 2019, pages 312-317
Very Early Coronary Artery Aneurysm After Primary Percutaneous Coronary Intervention in Patient With HIV and Thrombophilia
Dinaldo C. Oliveiraa, b, c, Carolina G.C. Oliveiraa, Vitor N. Mirandaa, Maria Isabel Gadelhaa, Jose Breno S. Filhob
aFederal University of Pernambuco, UFPE, Recife, Brazil
bUniversity of Pernambuco, UPE, Recife, Brazil
cCorresponding Author: Dinaldo C. Oliveira, Rua Dr. Joao Asfora, 35. Ilha do Leite, CEP: Recife, Pernambuco, Brazil
Manuscript submitted June 22, 2019, accepted July 24, 2019
Short title: CCA After PCI in HIV and Thrombophilia
doi: https://doi.org/10.14740/cr907
| Abstract | ▴Top |
The incidence of coronary artery aneurysms ranges from 0.2% to 10.5%. Aneurysms have been described after percutaneous coronary interventions (PCIs) and hypersensitivity to polymers, nickel, cobalt, inflammatory reaction rich in eosinophils, drug released by the stent, fracture and malapposition of the stent, stent endothelialization delay, high pressures used in the procedures, oversizing of balloons and stents, unhealed dissections, atheroablative techniques, and trauma of the arterial wall are related to appearance of coronary artery aneurysms. In this case report, we described a patient with human immunodeficiency virus and thrombophilia who underwent primary PCI and at the end of the procedure had thrombi in the coronary artery. It was decided by triple therapy and new angiographic study 2 days later. This new angiography revealed thrombi resolution but the appearance of an aneurysm in the middle portion of the drug-eluting stent. The anticoagulant was stopped and we performed watchful waiting strategy with new serial angiograms that revealed progressive reduction and disappearance of the aneurysm. Subsequently triple therapy with warfarin, aspirin and clopidogrel was restarted and the patient progressed asymptomatic and performed his daily activities normally. At 6 months of clinical follow-up, we advised the patient to suspend aspirin and to continue secondary prevention of cardiovascular events.
Keywords: Coronary artery aneurysm; Percutaneous coronary intervention; Drug-eluting stent; Human immunodeficiency virus; Thrombophilia
| Introduction | ▴Top |
The prevalence of coronary artery aneurysms ranges from 0.2% to 10.5%. The most common etiologies are congenital or acquired, such as atherosclerosis, Kawasaki disease, Takayasu disease, infection, connective tissue disease, trauma and after percutaneous coronary intervention (PCI) [1].
The estimated prevalence of coronary events in patients with coronary artery aneurysms (CAAs) not related to percutaneous intervention ranges from 1.5% to 5%, but some authors argue that this prevalence does not correspond to real world data owing to the lack of large studies on the subject [2].
Aneurysms have been described after PCIs. This fact has gained great notoriety in the era of first-generation drug-eluting stents (DESs) because of the high rate of major cardiovascular events [1-3].
The following report describes a case of CAA that developed after PCI performed as a primary reperfusion technique in a patient with acute myocardial infarction with ST-segment elevation diagnosed by electrocardiography.
| Case Report | ▴Top |
The patient was a 36-year-old man who had human immunodeficiency virus (HIV), taking antiretroviral drugs, and antiphospholipid syndrome (stopped using warfarin by his own decision 6 months before).
He had chest pain with retrosternal discomfort radiating to the left arm, associated with nausea and dizziness, which motivated him to go to the emergency department of a local hospital but with a delay of 2 h.
On physical examination, the only abnormality observed was a blood pressure of 140/100 mm Hg. However, electrocardiography revealed ST-segment elevation in the V1 to V4 leads.
As a diagnosis of acute coronary syndrome with ST-segment elevation was established, the hemodynamic team was contacted, and the patient was taken to the catheterization laboratory. The following drugs were administered in the emergency department: aspirin, 300 mg; ticagrelor, 180 mg; metoprolol, 50 mg; simvastatin, 40 mg; and intravenous nitroglycerin. Moreover, laboratory tests were performed, and chest radiography was performed at bedside.
After 45 min of hospital delay, coronary angiography showed no significant stenosis in the right coronary, main left coronary and circumflex arteries. However, the anterior descending artery was occluded in the mid portion (Fig. 1).
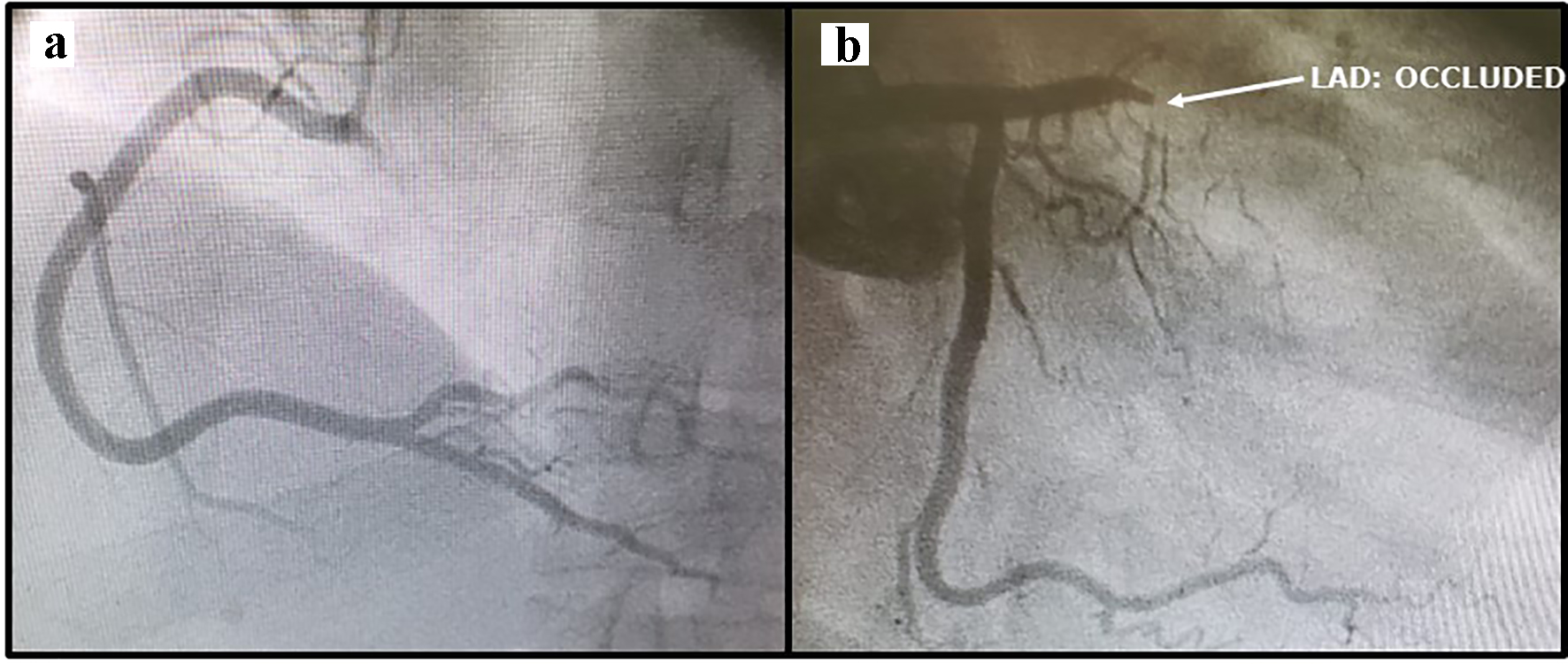 Click for large image | Figure 1. (a) Right coronary artery without stenosis. (b) Left main and left circumflex artery without stenosis, but left anterior descending (LAD) artery occluded. |
Primary PCI was chosen as a reperfusion strategy. Intravenous unfractionated heparin (100 unit/kg) was administered. A 0.014” floppy guidewire was positioned in the distal portion of the left anterior descending (LAD) artery through the occlusion. Then, pre-dilation was performed with a 2.5 × 20 mm balloon catheter inflated to 12 atm and a 3.0 × 24 mm DES deployed at 12 atm. Subsequently, intra-stent post-dilations were performed using a 3.5 × 10 mm balloon catheter inflated to 10 atm. Although a good result of the implanted stent was observed on the control coronary angiography, images also suggested the presence of thrombi in the mid portion of the LAD in areas distant from that manipulated with balloons and stent (Fig. 2).
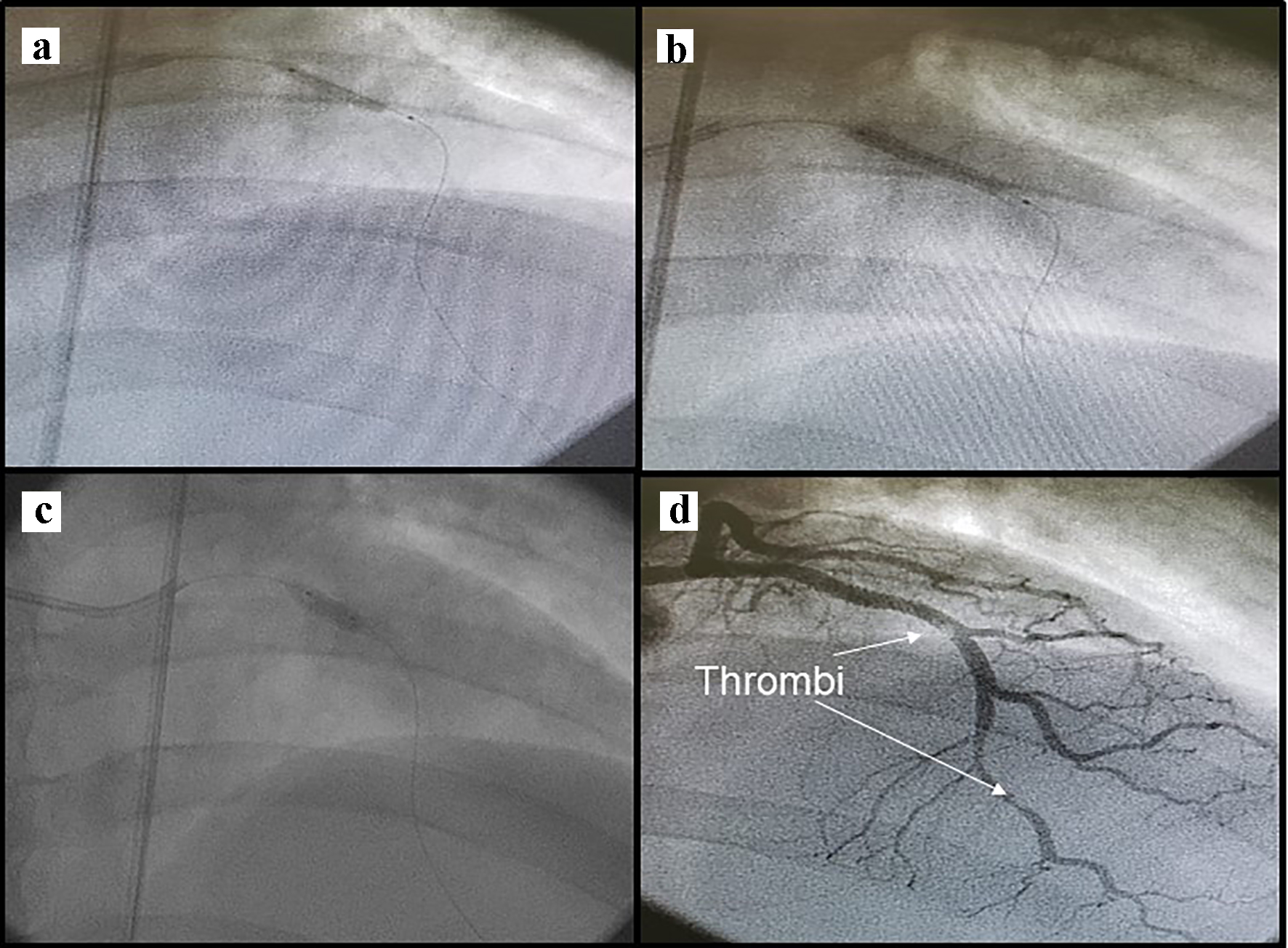 Click for large image | Figure 2. (a) Pre-dilatation (catheter balloon 2.5 × 20 mm). (b) Drug-eluting stent (3 × 24 mm) deployment. (c) Post-dilatation (catheter balloon 3.5 × 10 mm). (d) Thrombi in the left anterior descending artery. |
The activated clotting time was over 300 s. There was no success in attempted thrombi aspiration. However, at that time, the patient was asymptomatic and showed improvement of approximately 80% in the ST-segment elevation.
Given the possibility of red thrombi due to thrombophilia associated with white thrombi, it was decided to continue administering the dual antiplatelet therapy (aspirin and ticagrelor) and enoxaparin (1 mg/kg every 12 h) in the coronary care unit (CCU), and a new coronary angiography was scheduled for 2 days after the index procedure.
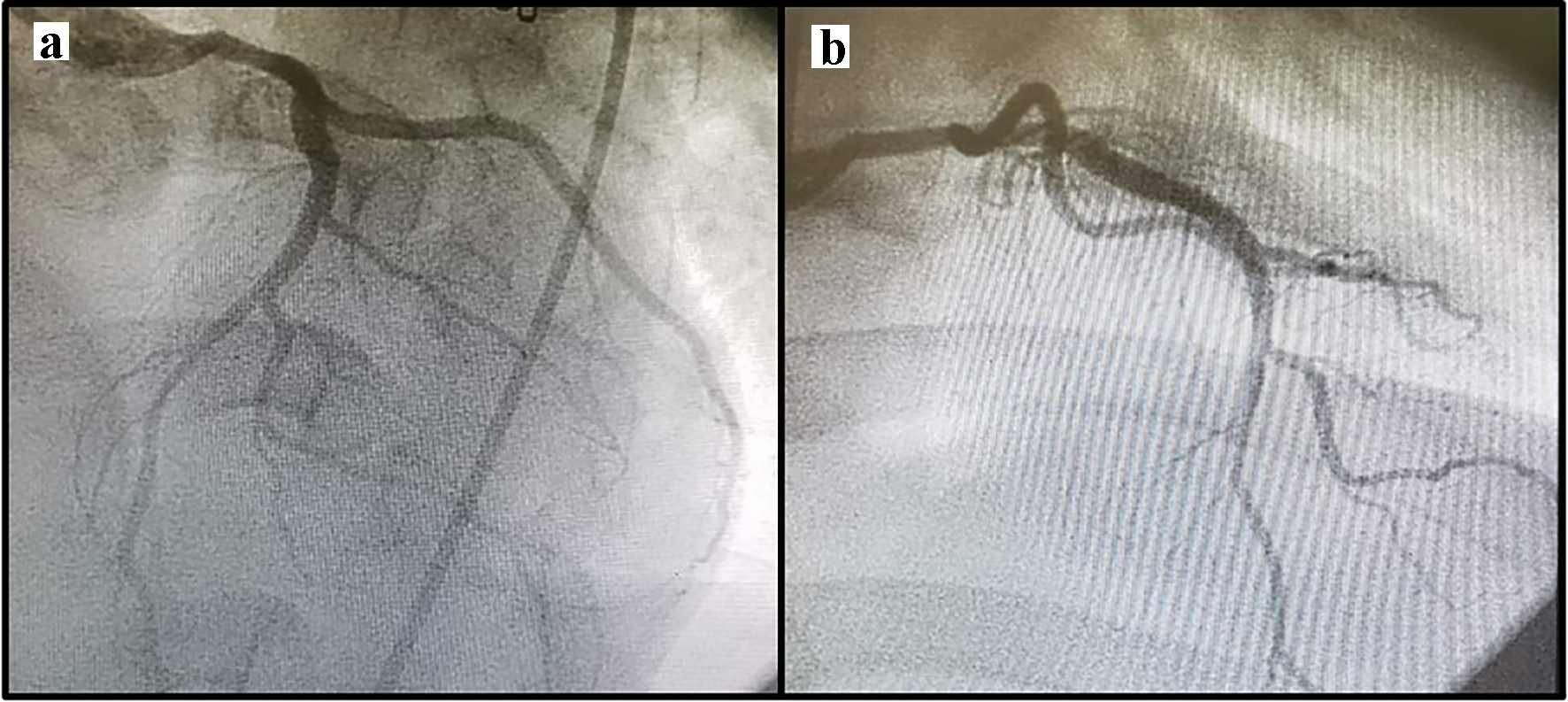
The new coronary angiography revealed complete disappearance of the thrombi, but an imaging finding from the mid portion of the stent was suggestive of aneurysm (Fig. 3). Thus, it was decided to suspend the anticoagulant and proceed with watchful waiting during the patient’s stay in the CCU. A new angiography was scheduled for 4 days later (6 days after the index procedure).
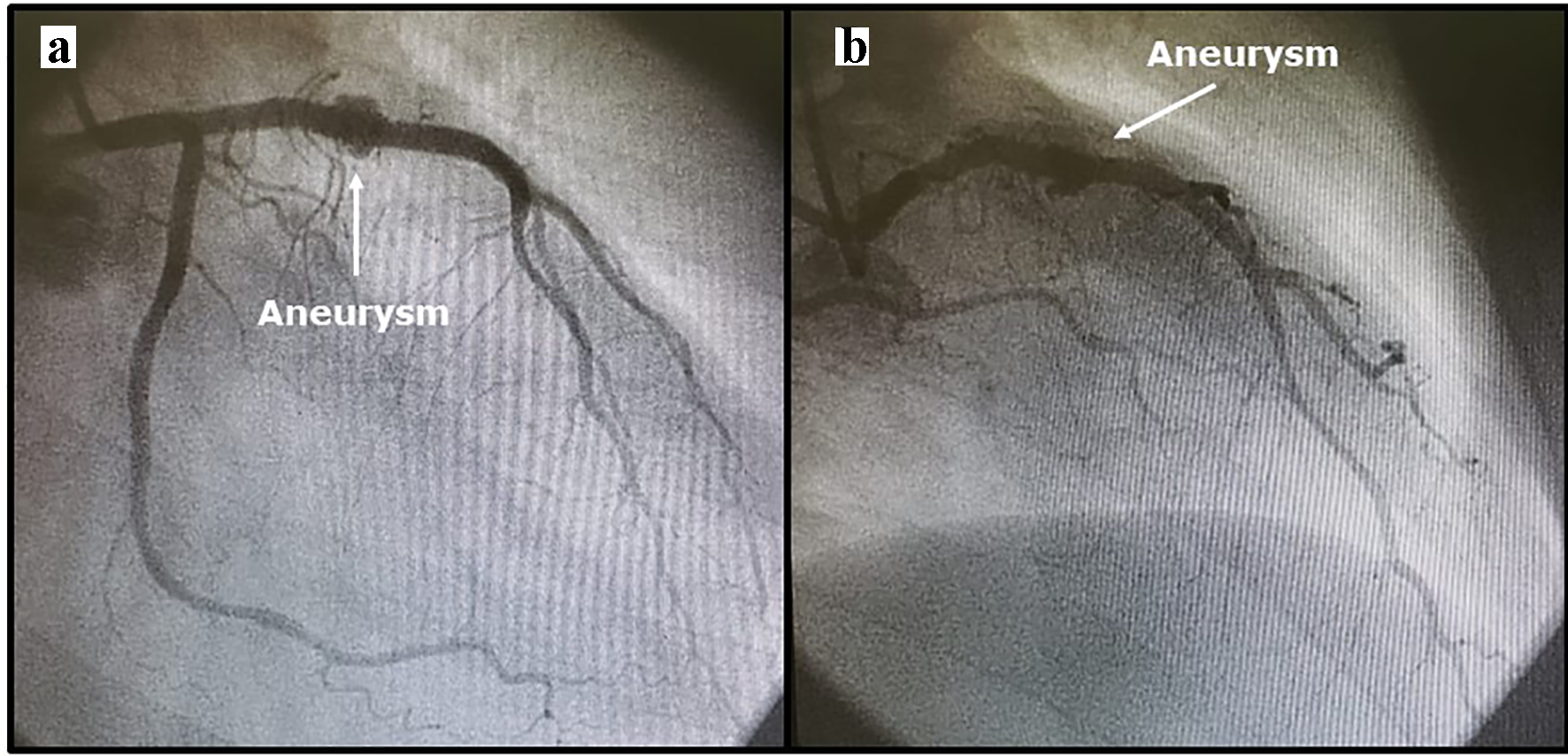 Click for large image | Figure 3. (a, b) Aneurysm 2 days after primary percutaneous coronary intervention. |
After 4 days of disease (aneurysm) diagnosis and after 6 days of PCI, with the patient asymptomatic, the new angiography showed that the aneurysm had not completely disappeared but showed a significant reduction in size (Fig. 4). The strategy was maintained, and another angiography was scheduled for 7 days.
 Click for large image | Figure 4. Aneurysm with significant reduction in size 6 days after percutaneous coronary intervention. |
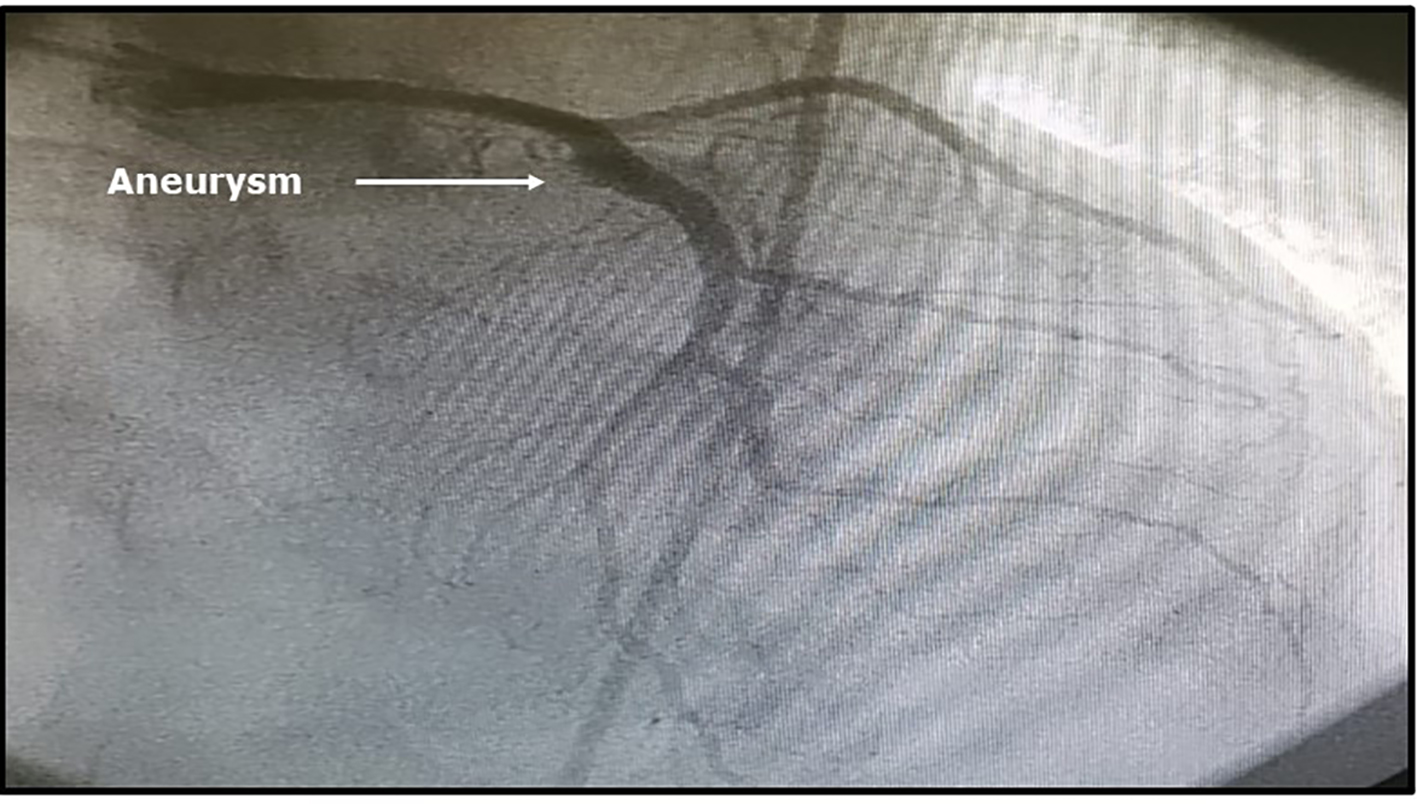
The patient remained asymptomatic, and the new angiography performed 7 days later (i.e. 13 days after the index procedure) revealed total disappearance of the aneurysm and one intermediate stenosis in the mid portion of the LAD (Fig. 5).
 Click for large image | Figure 5. (a, b) Images showing total disappearance of the aneurysm 11 days after very first diagnosis. |
Three days later, the patient started using warfarin, and ticagrelor was replaced with clopidogrel. Subsequently, the warfarin dose was adjusted according to the international normalized ratio, and the patient was discharged, asymptomatic and at Killip I classification. He continued taking aspirin, clopidogrel, warfarin, simvastatin, beta blocker and angiotensin converting enzyme inhibitor and was referred for cardiovascular rehabilitation.
At the 6-month follow-up, he was asymptomatic, performing his activities of daily living normally, and taking the medications prescribed at hospital discharge. In view of the evolution of his condition, it was decided to suspend aspirin and maintain the other medications for up to 1 year, when a new consultation was scheduled.
| Discussion | ▴Top |
In the present case, an imaging finding obtained 2 days after the primary PCI for acute myocardial infarction was suggestive of aneurysm. The definition of true or false aneurysm based on the coronary angiography cannot be done [1-3].
Coronary aneurysms are considered true aneurysms when all the arterial layers are involved and false aneurysms when only one or two layers are involved and, sometimes, only the adventitia is integrated [3].
The formation of a CAA after PCI is related to some factors not present in the context of CAAs not treated percutaneously. The emergence of aneurysms has been described from 3 days up to 4 years [1, 2, 4].
The factors related to PCI that are most commonly associated with the formation of aneurysms are hypersensitivity to polymers, nickel, cobalt, inflammatory reaction rich in eosinophils, drug released by the stent, fracture and malapposition of the stent stems, stent endothelialization delay, high pressures used in the procedures, oversizing of balloons and stents, unhealed dissections, atheroablative techniques and trauma of the arterial wall [1, 2, 5].
Some of these factors are possibly related to later aneurysm formation, such as the type of inflammatory reaction, hypersensitivity, stent fracture and malapposition, released drug and endothelialization delay, while others may be related to earlier formation, such as unhealed dissections, high release pressures, oversizing of balloons and arterial trauma [2-5].
The patient may have had a pseudoaneurysm due to the oversizing of the balloon used and the high inflation pressures. It is noteworthy that at the end of the index procedure, no image suggested aneurysm, but a new angiographic study performed after 48 h, which showed a very early aneurysm.
In addition to atherosclerosis, the patient had ST-segment elevation myocardial infarction (STEMI), HIV and thrombophilia. Therefore, at that time, he already had increased hypercoagulability due to the sum of the factors described.
The treatment of post-PCI aneurysms can be clinical or through new revascularization (percutaneous or surgical intervention). Some series of aneurysms after first-generation DES implantation had a high prevalence of clinical events. Although the treatment of CAAs depends on their location and size, as well as the risk of clinical events, many post-intervention aneurysms are treated with new interventions [1, 2].
Covered (polytetrafluoroethylene (PTFE), saphenous vein or papyrus) stent implantation, new DES or bare metal stent (BMS) placement and spring release inside the aneurysm are the most frequently used percutaneous techniques to treat aneurysm [3, 6-8]. The usefulness of covered stent (PTFE covered stent) implantation should be evaluated considering the risk of thrombosis and high restenosis reported in some studies [3, 6]. The present patient had HIV, STEMI and thrombophilia, and the implantation of this type of stent could be associated with a high risk of thrombosis. In fact, this risk would be impossible to precisely predict, although in view of the aforementioned fact, it is expected to be high.
New DES or BMS placement would mean a double layer of metal within an artery of a patient in an increased prothrombotic state and an increased risk of thrombosis and restenosis. Coil is implanted using a technique that, although aimed only at thrombosis of aneurysms, is technically challenging and associated with risks [1].
The risk of aneurysm thrombosis is low in a patient receiving dual antiplatelet therapy and full anticoagulation. In smaller-diameter arteries with high flow, the trigger of thrombus formation is platelets. However, in vessels of larger diameter and slow flow, the trigger is coagulation factors [1, 2].
The use of antiplatelets and anticoagulants has been recommended in the clinical treatment of coronary aneurysms not related to PCI. Certainly, the rationale for administering vitamin K inhibitors is that the dilated areas of the aneurysm, their irregular surface, and the turbulent and slow flow as compared with that in vessels without aneurysm are associated with the formation of thrombus not only related to platelets but also associated with coagulation factors [1, 2].
On the basis of the aforementioned rationale and the fact that the use of coils is aimed thrombosis for the subsequent healing of aneurysms, we decided to suspend the anticoagulant therapy, aiming to promote thrombosis of the aneurysm for healing, even though we were aware of the risk of stent thrombosis because of the thrombophilia and also due to hypercoagulability status because of HIV [9, 10]. The patient was kept in the coronary unit for risk monitoring.
Kwon et al [11] described a case in which an acute stent thrombosis (patient taking dual antiplatelet therapy) was a consequence of aneurysm thrombosis involved in a lesion treated with a DES. The authors observed a hematoma in the arterial wall. In view of this, we can assume that patients receiving dual antiplatelet therapy can develop thrombosis of aneurysm after undergoing stent implantation. So, we imagined that one aneurysm can be thrombosed and healed in patient taking dual antiplatelet therapy.
Therefore, we predicted that aneurysm thrombosis and healing would occur if the patient continued receiving dual antiplatelet therapy, but it would be necessary to stop anticoagulant to improve this possibility. However, we knew of the risk of stent thrombosis, but we did anticipate the resolution of the problems, in other words, we tried to be ready for intervention and the patient was kept in the CCU. Of note, the standard treatment for antiphospholipid syndrome is warfarin, and the new oral anticoagulants have not been tested or recommended.
The knowledge of coronary atherosclerosis in HIV patients is increasing. The immune system condition and inflammatory response in young HIV patients seem to be similar to those in the elderly, which suggests immune aging with loss of reserve response. Moreover, their atheroma is characterized by a thin fibrous layer, inflammatory cells, and a tendency to rupture before causing significant stenosis [9, 10].
Ayers et al described a case of a 22-year-old patient who had HIV and thrombophilia (positive lupus antiphospholipids) who had acute myocardial infarction due to non-fully occlusive thrombosis of the LAD. His coronary angiography also revealed multiple aneurysms but there were no areas of atherosclerotic stenosis. We believe that the hypercoagulability state in this patient was high and contributed to this clinical event. In a similar way, we believe that our patient also had a high state of hypercoagulability [12].
Three days after the disappearance of the angiographic image of the aneurysm, the anticoagulant was restarted. As warfarin was required, ticagrelor was replaced with clopidogrel (switching), but according to guidelines [13], patient who is taking warfarin and dual antiplatelet therapy should take clopidogrel (not ticagrelor) and aspirin for while. This was done because after the resolution of the aneurysm, the patient needed to be protected from thrombotic phenomena.
Intracoronary ultrasound and/or optical coherence tomography are useful when PCI is performed to treat aneurysms or to obtain information on some anatomical aspects in detail, such as the differences between pseudoaneurysm and true aneurysm, and to guide optimal stent implantation [1-3]. Watchful waiting was the initial strategy used in the present case, without performing imaging techniques but considering it in advance in case intervention was necessary at some point.
This paper presented a case of CAA after very early coronary intervention (2 days). Considering the clinical scenario and the patient’s comorbidities, a strategy for clinical management and rigorous monitoring was chosen, and the pre-established objectives were achieved. Despite the success in this case, no standard treatment for CAAs after PCI has been established. Thus, this clinical scenario should be further investigated. According to our knowledge, this is the case of the earliest coronary aneurysm after PCI described.
Acknowledgments
None to declare.
Financial Disclosure
None to declare.
Conflict of Interest
None to declare.
Informed Consent
Inform consent was obtained from the patient.
Author Contributions
DCO reviewed literature and wrote the paper. CGCO, VNM and MIG reviewed literature. JBS reviewed paper.
| References | ▴Top |
- ElGuindy MS, ElGuindy AM. Aneurysmal coronary artery disease: An overview. Glob Cardiol Sci Pract. 2017;2017(3):e201726.
doi pubmed - Abou Sherif S, Ozden Tok O, Taskoylu O, Goktekin O, Kilic ID. Coronary artery aneurysms: a review of the epidemiology, pathophysiology, diagnosis, and treatment. Front Cardiovasc Med. 2017;4:24.
doi pubmed - Singh G, Khemani H, Singla R, Shaikh S, Patil V, Bansal NO. Intravascular ultrasound-guided management of proximal left anterior descending artery aneurysm with covered stent - a case report. Cardiol Res. 2018;9(5):318-323.
doi pubmed - Gadepalli R, Rayidi G, Pramod G, Srivastava SK, Venkata Balakrishna SN. A case of early development of giant coronary artery aneurysms after drug-eluting stents implantation: An unpredictable menace. Interv Med Appl Sci. 2017;9(1):47-50.
doi pubmed - Saran RK, Dwivedi SK, Puri A, Sethi R, Agarwal SK. Giant coronary artery aneurysm following implantation of Endeavour stent presenting with fever. Indian Heart J. 2012;64(2):198-199.
doi - Bajaj S, Parikh R, Hamdan A, Bikkina M. Covered-stent treatment of coronary aneurysm after drug-eluting stent placement: case report and literature review. Tex Heart Inst J. 2010;37(4):449-454.
- Cotter R, Krantz M, Hogan S, Holland M. Exclusion of a giant coronary artery aneurysm with covered stents using a long drug eluting stent scaffold. Clincal Medicine Insights: Case reports. 2019;12:1-3.
doi pubmed - Hada Y, Fujii H, Shimizu M, Yamawake N, Nishizaki M. Effectiveness of bare metal stent implantation for the treatment of coronary artery aneurysm: a multimodality imaging evaluation. Intern Med. 2017;56(24):3305-3309.
doi pubmed - Sokoya T, Steel HC, Nieuwouldt M, Rossouw TM. HIV as a cause of imune activation and immunosenescence. Mediators Inflamm. 2017;2017:6825493.
doi pubmed - Kearns A, Gordon J, Burdo TH, Qin X. HIV-1-Associated Atherosclerosis: Unraveling the Missing Link. J Am Coll Cardiol. 2017;69(25):3084-3098.
doi pubmed - Kwon TJ, Hwang JY, Kwak CH, Jeong YH, Park YW, Hwang SJ, Park JR, et al. Rupture and spontaneous sealing of a coronary aneurysm after deployment of drug-eluting stent. Korean Circ J. 2012;42(8):558-561.
doi pubmed - Ayers J, Mandell R, Sanghvi K, Aboujaoude R, Hsi DH. Acute coronary thrombosis and multiple coronary aneurysms in a 22-year-old man with the human immunodeficiency virus. Tex Heart Inst J. 2014;41(2):208-211.
doi pubmed - Valgimigli M, Bueno H, Byrne RA, Collet JP, Costa F, Jeppsson A, Juni P, et al. 2017 ESC focused update on dual antiplatelet therapy in coronary artery disease developed in collaboration with EACTS: The Task Force for dual antiplatelet therapy in coronary artery disease of the European Society of Cardiology (ESC) and of the European Association for Cardio-Thoracic Surgery (EACTS). Eur Heart J. 2018;39(3):213-260.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cardiology Research is published by Elmer Press Inc.


