| Cardiology Research, ISSN 1923-2829 print, 1923-2837 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, Cardiol Res and Elmer Press Inc |
| Journal website http://www.cardiologyres.org |
Original Article
Volume 9, Number 1, February 2018, pages 11-16
The Severity of Coronary Arterial Stenosis in Patients With Acute ST-Elevated Myocardial Infarction: A Thrombolytic Therapy Study
Salih Kilica, d, Umut Kocabasb, Levent Hurkan Canc, Oguz Yavuzgilc, Mehdi Zoghic
aDepartment of Cardiology, Doctor Ersin Arslan Research and Training Hospital, Gaziantep, Turkey
bDepartment of Cardiology, Soma State Hospital, Manisa, Turkey
cDepartment of Cardiology, Ege University Faculty of Medicine, Izmir, Turkey
dCorresponding Author: Salih Kilic, Department of Cardiology, Doctor Ersin Arslan Research and Training Hospital, Gaziantep, Turkey
Manuscript submitted November 23, 2017, accepted December 1, 2017
Short title: Coronary Stenosis in STEMI
doi: https://doi.org/10.14740/cr639w
| Abstract | ▴Top |
Background: It is widely believed that ST-elevated myocardial infarction (STEMI) generally occurs at the site of mild to moderate coronary stenosis. The aim of this study was to determine the degree of stenosis of infarct-related artery (IRA) in STEMI patients who underwent coronary angiography (CAG) after successful reperfusion with thrombolytic therapy (TT).
Methods: A total of 463 consecutive patients between January 2008 and December 2013 with acute STEMI treated with TT were evaluated retrospectively. The patients in whom reperfusion failed (n = 120), death occurred before CAG (n = 12), IRA cannot be determined (n = 10), and CAG was not performed in index hospitalization (n = 54) were excluded from the study. To determine the severity of stenosis of IRA, two experienced cardiologists who were unaware of each other used quantitative CAG analysis. Significant stenosis was defined as a ≥ 50% stenosis in the coronary artery lumen. A total of 267 patients who were successfully reperfused with TT and in whom CAG was performed during hospitalization with median 8 (1 - 17) days after myocardial infarction were included in the study.
Results: The mean age of patients was 55.7 ± 10.8 years (85.5% male). Most of the patients had a significant stenosis in IRA ( ≥ 50%, n = 236, group 1) after successful TT; whereas only 11.6% had stenosis < 50% (n = 31, group 2). In addition, majority of the patients had ≥ 70.4% (n = 188, 70.4%) stenosis in IRA. Average of stenosis in IRA was 74±16%.
Conclusions: In contrast to the general opinion, we detected that majority of STEMI patients had a significant stenosis in IRA.
Keywords: Severity coronary artery; STEMI; Thrombolytic therapy
| Introduction | ▴Top |
Major components of acute coronary artery occlusion causing ST-elevated myocardial infarction (STEMI) are thrombus and an underlying atherosclerotic plaque. The underlying stenosis degree of atherosclerotic plaque has been a subject of curiosity for a long time and been examined in several studies, but discussions are still ongoing. In the earlier stages, retrospective angiographic and post-mortem studies have shown that the majority of patients with STEMI had mild to moderate degree of stenosis in the infarct-related artery (IRA) and was emphasized that acute event was secondary to thrombosis, more often occurring after plaque rupture [1-4]. However, in some post-mortem studies, it is shown that the severe stenosis was the cause in many patients [5, 6]. Unlike the retrospective studies in the early stages, Coronary Artery Surgery Study (CASS) has shown that new vessel occlusions resulted from severe stenosis in a majority of patients who underwent coronary angiography (CAG) in the follow-up [7]. Similarly, in studies evaluating mechanical thrombectomy or thrombolytic therapy (TT) it was seen that IRA had severe stenosis [8, 9]. However, it is also shown that the residual thrombus may occur after thrombectomy or TT, and the degree of stenosis at IRA stenosis could be detected more than its actual occurrence [10-12]. More thrombus can be removed from lesion by the more aggressive antiplatelet therapy together with TT, and the degree of stenosis on angiography can be estimated more clearly. With this hypothesis we have designed this study.
The purpose of this study was to determine the degree of stenosis of IRA in STEMI patients who underwent CAG after reperfusion with TT.
| Methods | ▴Top |
A total of 463 consecutive patients between January 2008 and December 2013 with STEMI treated primarily with TT were evaluated retrospectively. In our clinic primary percutaneous intervention can only be performed during working hours between January 2008 and December 2013. Thus, patients that have been hospitalized with STEMI after working hours received therapy. The study was approved by institutional ethics committee. The patients in whom reperfusion failed and rescue percutaneous coronary intervention was performed (n = 120), death occurred before CAG (n = 12), IRA cannot be determined according to the electrocardiographic (ECG), echocardiographic (ECHO) or CAG (n = 10), and CAG was not performed in index hospitalization (n = 54) were excluded from the study. There were no further exclusion criteria. A total of 267 patients who were successfully reperfused with TT and in whom CAG was performed during hospitalization with median 8 (1 - 17) days after myocardial infarction were included in the study. Figure 1 depicts flow chart of the study. Clinical and demographic characteristics including age, gender, diabetes mellitus (DM), hypertension (HT), hyperlipidemia (HPL), current cigarette smoking, and family history of premature coronary artery disease (CAD), were obtained by hospital records. The diagnosis of STEMI was based on typical symptoms onset of ≥ 30 min and ≤ 12 h before admission to the hospital and new ST-segment elevation at the J point in more than two contiguous leads ( > 0.2 mV in V1 through V3 and > 0.1 mV in other leads) or new left branch bundle block [13]. The IRA was clearly defined on the basis of the combination of ECG, ECHO, and CAG findings. Failed reperfusion was defined according to the following criteria: < 50% ST resolution-related ECG leads within 90 min from initiation of the thrombolytic treatment and lack of symptom relief or in-hospital mortality.
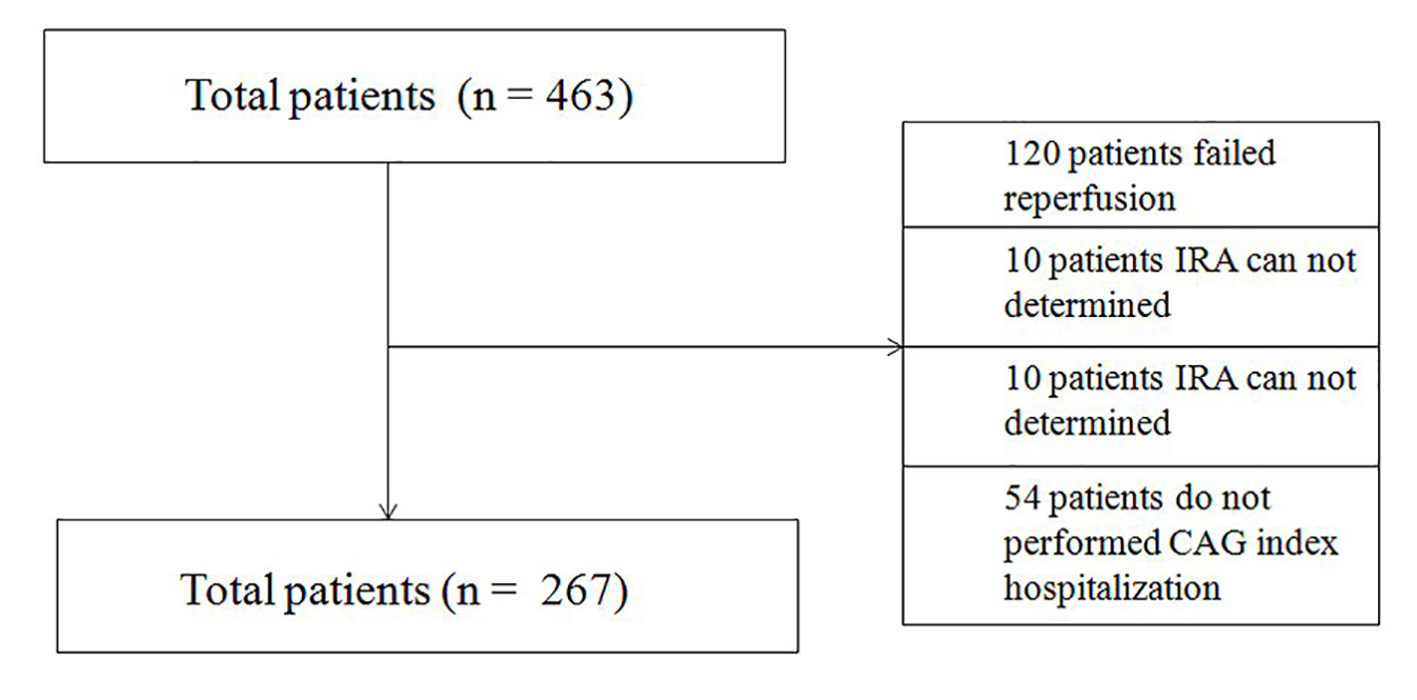 Click for large image | Figure 1. Flow chart of the study. |
The thrombolytic agent administered was a recombinant tissue-type plasminogen activator (rt-PA, alteplase), tenectoplase or reteplase. All patients received unfractionated heparin or enoxaparin, aspirin, and clopidogrel at recommended doses in relevant guidelines [14]. Two experienced cardiologists, who were unaware of each other to determine the degree of stenosis in the IRA, assessed CAG of the patients. Compliance between data taken by two doctors was detected at very high levels (ICC = 0.888, 95% CI: 0.805 - 0.930, P = 0.001). The computer-based ACOM PC 5.01 (Siemens Medical Systems, Inc., Erlangen, Germany) was used for off-line quantitative CAG analysis. Measurements were performed in end-diastole in the projection that best showed the diseased segment with as little foreshortening as possible. Minimal lumen diameter (mm), were measured. Thrombolysis in myocardial infarction (TIMI) grade 2 or 3 flow was detected on all CAG. Hypertension was defined as repeated measurements of systolic blood pressure > 140 mm Hg, diastolic > 90 mm Hg, or treatment with antihypertensive medications. DM was defined as a prior diagnosis and/or fasting blood glucose > 126 mg/dL or use of antidiabetic medications. Hyperlipidemia was considered as a total cholesterol level above 200 mg/dL or the use of lipid-lowering medications. Cigarette smoking was defined as smoking 1 or more cigarettes a day for more than 1 year without a quit attempt.
Statistical analysis
All the data were analyzed with SPSS (Statistical Package for the Social Sciences) software for Windows Version 20.0. Categorical variables were expressed as percentages, and using Chi-square or Fisher’s exact test as appropriate compared their frequencies. Continuous variables with a normal distribution were expressed as mean ± standard deviation, and were compared using a Student’s t-test. The continuous variable without a normal distribution was expressed as median (maximum - minimum) and was compared using the Mann-Whitney U test. The normality of data distribution was verified by Kolmogorov-Smirnov test. Homogeneity of variance was assessed by Levene’s test. P values of < 0.05 were considered statistically significant.
| Results | ▴Top |
The mean age of the patients was 55.7 ± 10.8 years and 85.5% were male. Most of patients had a significant stenosis in IRA ( ≥ 50%, n = 236, group 1) after successful TT; whereas only 11.6% had stenosis < 50% (n = 31, group 2). The main clinical characteristic features of the patients are summarized in Table 1. The majority of patients (76.8%) were smokers. Hypertension (40.1%) was the most frequent comorbidity followed by DM (27.7%), and HPL (25.8%). No significant differences in terms of characteristics and laboratory values between the groups were detected except that the group 1 patients had high obesity rate. Left anterior descending coronary artery (44.9%, n = 120) was the most frequent IRA, followed by right coronary artery (38.2%, n = 102), left circumflex artery (9.7%, n = 26) and other arteries (7.2%, n = 19). There was no difference in distribution of IRA between groups (Table 2). Average of stenosis in IRA was 74±16%. The stenosis of IRA was > 50% in 88.4% (n = 236) and was > 70% in 70.4% (n = 188) patients. There were no significant differences between groups in term of elapsed time, between the onset of pain and admission hospital (Table 1). More than two-thirds of the patients had been admitted to hospital < 3 h from pain onset. Elapsed median time from myocardial infarction to CAG was 8 (1 - 17) days and there were no significant differences between groups. Table 3 summarizes the treatment of the patients on admission and during hospitalization. All patients received aspirin, clopidogrel and unfractionated heparin (UFH) or low molecular weight heparin (LMWH) on admission to hospital and until CAG was performed. In addition, most of the patients have received statin (97%), β-blocker (94%) and angiotensin converting enzyme inhibitors (ACEIs) or angiotensin receptor blocker (ARB) (92%). Differences were not observed between the groups in terms of drug usage.
 Click to view | Table 1. Basal Characteristic Features and Laboratory Values of the Patients |
 Click to view | Table 2. Angiographic Data After Successful Thrombolytic Therapy |
 Click to view | Table 3. Medical Treatment in Admission and During Hospitalization |
| Discussion | ▴Top |
In present study, angiographic assessment of lesion severity was objectively quantified in patient with STEMI after successful TT. Our results suggested that STEMI predominantly occurred at sites with angiographic stenosis ≥ 50% and a minority of patients with STEMI had IRA stenosis with < 50%. In contrast to our study, earlier angiographic studies had suggested that IRA lesions typically had ≤ 50% diameter stenosis before the acute coronary events [1, 2, 15-17]. However, in these small retrospective studies, the interval between the index angiogram and acute coronary syndrome was often very long. The time intervals between the index event and previous angiography ranged from 6 weeks to 11 years, with an average of 3.3 years in those studies. Little et al in a study enrolling 42 patients demonstrated that in 66% of patients the artery that subsequently occluded had < 50% stenosis and 97% of patients had < 70% stenosis on the initial angiography. Of note, the first angiography was performed 706 ± 685 days before acute myocardial infarction [1]. Ambrose et al reported the similar observation that the time interval between the initial angiogram and infarction varied from 1 month to 7 years (median 18 months) [2]. Indeed, Dacanay et al showed that among patients with Q-wave infarction and the first angiogram < 18 months before acute myocardial infarction (AMI), 82% had a stenosis severity of > 50% as compared with only 33% when the first angiogram was < 18 months from AMI [3]. Similarly, Zaman et al with a population of 42 STEMI patients with angiography before STEMI showed that lesions leading to STEMI ≤ 3 months after evaluation were more severe than those leading to STEMI > 3 months before AMI [18]. This relatively long time interval and sometimes rapid progression of coronary artery disease in many patients make such extrapolations questionable. Besides, other important issues that can be discussed are that these studies had small samples and were retrospective. On the other hand, there are many studies that evaluated the degree of IRA had shown that majority of patients with STEMI had critical angiographically stenosis in IRA [7, 8, 19]. In their study Frobert et al investigated 250 consecutive STEMI patients referred for primary PCI. Upon flow restoration (spontaneously or after “wiring” of the vessel), the investigators found that angiographically the degree of IRA stenosis > 50% in 96% of the patients while it was > 70% in 66% of the patients [19]. Similarly, Manoharan et al detected that the degree of IRA stenosis in patients with STEMI after thrombus aspiration restored normal antegrade coronary blood flow. The study has shown that STEMI predominantly occurred at sites with angiographic diameter stenosis > 50%. Only 11% of patients with STEMI had IRA with diameter stenosis < 50% after aspiration of thrombus material [8]. However, in both studies, persistent thrombus may have led to overestimation of the severity of the underlying stenosis in IRA. The CASS registry has shown that the most important predictor of the new segment stenosis was the degree of stenosis at the initial lesion and the occlusion rate at follow-up of 5 years was 20-fold higher in the lesions having initial critical stenosis compare to the lesions without initial critical stenosis [7]. Intravascular ultrasound (IVUS) and fractional flow reserve (FFR) has been used in several studies to determine the degree of stenosis in challenging lesions. Abizaid et al showed that the possibility of myocardial infarction was positively correlated with the degree of stenosis in IVUS in a prospective study [20]. The increase of the degree of stenosis in the basal angiography was associated with major cardiovascular events for the following 3-year period in the PROSPECT study (Providing Regional Observations to Study Predictors of Events in the Coronary Tree) [21]. The results of both studies were supported by prospective DEFER study, where the patients without significant coronary stenosis (fractional flow reserve > 0.75) were randomized to medical treatment or PCI [22]. While the annual death rate and acute coronary syndrome of the patients with non-critical stenosis during the 5-year follow-up was < 1%, this rate was found to be five times higher in the cohort whose stenosis was critical. Mathey et al have shown in their study that artery was re-canalized in 48 patients with an AMI diagnosis following catheter-mediated intracoronary streptokinase infusion. But a high degree of stenosis was found, and all patients had coronary artery bypass graft (CABG) surgery. This should be taken into account as the presence of residual thrombus may overestimate lesion severity by angiography [23]. Van Lierde et al have examined the residual stenosis in STEMI patients, where 49 patients were given TT and 42 patients were given placebo. Almost 75% of patients had > 50% residual stenosis in IRA, and no difference were observed between the groups. Heparin was given as anti-thrombotic and aspirin as antiplatelet therapy [9]. Llevadot et al detected < 50% residual stenosis in 8.9% of 2,119 patients who participated in the TIMI 4, 10A, 10B and 14 studies and angiography performed 90 min after TT [12]. In this large study, measuring the degree of stenosis in an earlier time such as the 90 min after TT may have caused overestimation of residual stenosis. The importance of thrombolytic agent used for superimposed to mild-moderate stenosis is undeniable. In TIMI 14, patients who received combination therapy with a potent platelet inhibitor (abciximab) plus half-dose rt-PA (recombinant tissue plasminogen activator) were more likely to have a mild residual stenosis than those who received rt-PA alone, supporting that more complete thrombolysis results in less residual stenosis [12]. Our study’s results are consistent with IVUS, FFR and TT studies. The main problem after TT or thrombus aspiration is persistent thrombus that may lead to overestimation of the severity of the underlying stenosis in IRA. In our study CAGs were performed at a median 8 (1 - 17) days after successful TT and all patients receive the optimal therapy that recommended relevant guidelines (i.e. dual antiplatelet, anticoagulant and statin) until the time of CAG performed. While all patients in our study received dual antiplatelet therapy, in earlier studies patients received only aspirin. Dual antiplatelet therapy is likely to have made a contribution to decline in the amount of residual thrombus and may contributed to more accurate estimation of the degree of stenosis.
Out study has some important limitation. First limitation of our study is that it is a retrospective and single-center study. The second limitation of study is that we accessed coronary artery stesnosis only by CAG at median 8 days after reperfusion therapy. If we could access degree of stenosis with IVUS or optical coherence tomography (OCT) it would be a more accurate result about stenosis degree. But, because our study was designed retrospectively it was not possible. The third limitaiton of our study is that even we descirbed less overestimation of residual stenosis by thrombus because all patients were reperfused with TT and treated with dual antithrombotic therapy, the possibility of increased stenosis in CAG by thrombus remains. To clarify this issue, we need further studies. The fourth and most important limitation of this study is that almost half of patients who received TT and were evaluated for study were excluded because of death, failed reperfusion, IRA that cannot be determinated, and CAG that was not performed during hospitalizaiton. This might have led to selection bias because it could be speculated that these patients may have had less pronounced stenosis.
Conclusions
In contrast to the general opinion, we detected that majority of STEMI patients had a significant stenosis in IRA.
Acknowledgments
We would like to thank Dr. Burcu Yagmur and Dr. Hatice Soner Kemal for their kind help of the present study.
| References | ▴Top |
- Little WC, Constantinescu M, Applegate RJ, Kutcher MA, Burrows MT, Kahl FR, Santamore WP. Can coronary angiography predict the site of a subsequent myocardial infarction in patients with mild-to-moderate coronary artery disease? Circulation. 1988;78(5 Pt 1):1157-1166.
doi pubmed - Ambrose JA, Tannenbaum MA, Alexopoulos D, Hjemdahl-Monsen CE, Leavy J, Weiss M, Borrico S, et al. Angiographic progression of coronary artery disease and the development of myocardial infarction. J Am Coll Cardiol. 1988;12(1):56-62.
doi - Dacanay S, Kennedy HL, Uretz E, Parrillo JE, Klein LW. Morphological and quantitative angiographic analyses of progression of coronary stenoses. A comparison of Q-wave and non-Q-wave myocardial infarction. Circulation. 1994;90(4):1739-1746.
doi pubmed - Mann JM, Davies MJ. Vulnerable plaque. Relation of characteristics to degree of stenosis in human coronary arteries. Circulation. 1996;94(5):928-931.
doi - Qiao JH, Fishbein MC. The severity of coronary atherosclerosis at sites of plaque rupture with occlusive thrombosis. J Am Coll Cardiol. 1991;17(5):1138-1142.
doi - Davies MJ, Thomas A. Thrombosis and acute coronary-artery lesions in sudden cardiac ischemic death. N Engl J Med. 1984;310(18):1137-1140.
doi pubmed - Alderman EL, Corley SD, Fisher LD, Chaitman BR, Faxon DP, Foster ED, Killip T, et al. Five-year angiographic follow-up of factors associated with progression of coronary artery disease in the Coronary Artery Surgery Study (CASS). CASS Participating Investigators and Staff. J Am Coll Cardiol. 1993;22(4):1141-1154.
doi - Manoharan G, Ntalianis A, Muller O, Hamilos M, Sarno G, Melikian N, Vanderheyden M, et al. Severity of coronary arterial stenoses responsible for acute coronary syndromes. Am J Cardiol. 2009;103(9):1183-1188.
doi pubmed - Van Lierde J, De Geest H, Verstraete M, Van de Werf F. Angiographic assessment of the infarct-related residual coronary stenosis after spontaneous or therapeutic thrombolysis. J Am Coll Cardiol. 1990;16(7):1545-1549.
doi - Brown BG, Gallery CA, Badger RS, Kennedy JW, Mathey D, Bolson EL, Dodge HT. Incomplete lysis of thrombus in the moderate underlying atherosclerotic lesion during intracoronary infusion of streptokinase for acute myocardial infarction: quantitative angiographic observations. Circulation. 1986;73(4):653-661.
doi pubmed - Hong YJ, Jeong MH, Choi YH, Ma EH, Ko JS, Lee MG, Park KH, et al. Differences in intravascular ultrasound findings in culprit lesions in infarct-related arteries between ST segment elevation myocardial infarction and non-ST segment elevation myocardial infarction. J Cardiol. 2010;56(1):15-22.
doi pubmed - Llevadot J, Giugliano RP, McCabe CH, Cannon CP, Antman EM, Murphy S, Gibson CM. Degree of residual stenosis in the culprit coronary artery after thrombolytic administration (Thrombolysis In Myocardial Infarction [TIMI] trials). Am J Cardiol. 2000;85(12):1409-1413.
doi - Thygesen K, Alpert JS, Jaffe AS, Simoons ML, Chaitman BR, White HD, Joint ESCAAHAWHFTFftUDoMI, et al. Third universal definition of myocardial infarction. Circulation. 2012;126(16):2020-2035.
doi pubmed - Van de Werf F, Bax J, Betriu A, Blomstrom-Lundqvist C, Crea F, Falk V, Filippatos G, et al. Management of acute myocardial infarction in patients presenting with persistent ST-segment elevation: the Task Force on the Management of ST-Segment Elevation Acute Myocardial Infarction of the European Society of Cardiology. Eur Heart J. 2008;29(23):2909-2945.
doi pubmed - Hackett D, Verwilghen J, Davies G, Maseri A. Coronary stenoses before and after acute myocardial infarction. Am J Cardiol. 1989;63(20):1517-1518.
doi - Giroud D, Li JM, Urban P, Meier B, Rutishauer W. Relation of the site of acute myocardial infarction to the most severe coronary arterial stenosis at prior angiography. Am J Cardiol. 1992;69(8):729-732.
doi - Moise A, Lesperance J, Theroux P, Taeymans Y, Goulet C, Bourassa MG. Clinical and angiographic predictors of new total coronary occlusion in coronary artery disease: analysis of 313 nonoperated patients. Am J Cardiol. 1984;54(10):1176-1181.
doi - Zaman T, Agarwal S, Anabtawi AG, Patel NS, Ellis SG, Tuzcu EM, Kapadia SR. Angiographic lesion severity and subsequent myocardial infarction. Am J Cardiol. 2012;110(2):167-172.
doi pubmed - Frobert O, van’t Veer M, Aarnoudse W, Simonsen U, Koolen JJ, Pijls NH. Acute myocardial infarction and underlying stenosis severity. Catheter Cardiovasc Interv. 2007;70(7):958-965.
doi pubmed - Abizaid AS, Mintz GS, Mehran R, Abizaid A, Lansky AJ, Pichard AD, Satler LF, et al. Long-term follow-up after percutaneous transluminal coronary angioplasty was not performed based on intravascular ultrasound findings: importance of lumen dimensions. Circulation. 1999;100(3):256-261.
doi pubmed - Yun KH, Mintz GS, Farhat N, Marso SP, Taglieri N, Verheye S, Foster MC, et al. Relation between angiographic lesion severity, vulnerable plaque morphology and future adverse cardiac events (from the Providing Regional Observations to Study Predictors of Events in the Coronary Tree study). Am J Cardiol. 2012;110(4):471-477.
doi pubmed - Pijls NH, van Schaardenburgh P, Manoharan G, Boersma E, Bech JW, van’t Veer M, Bar F, et al. Percutaneous coronary intervention of functionally nonsignificant stenosis: 5-year follow-up of the DEFER Study. J Am Coll Cardiol. 2007;49(21):2105-2111.
doi pubmed - Mathey DG, Rodewald G, Rentrop P, Leitz K, Merx W, Messmer BJ, Rutsch W, et al. Intracoronary streptokinase thrombolytic recanalization and subsequent surgical bypass of remaining atherosclerotic stenosis in acute myocardial infarction: complementary combined approach effecting reduced infarct size, preventing reinfarction, and improving left ventricular function. Am Heart J. 1981;102(6 Pt 2):1194-1201.
doi
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cardiology Research is published by Elmer Press Inc.


