| Cardiology Research, ISSN 1923-2829 print, 1923-2837 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, Cardiol Res and Elmer Press Inc |
| Journal website http://www.cardiologyres.org |
Original Article
Volume 7, Number 2, April 2016, pages 59-65
Interesting Correlation Between the Circulating Pentraxin 3 and Cardiac Rehabilitation Program Outcomes in Coronary Artery Bypass Grafting Patients
Habib Haybara, Babak Payamia, Isa Khaheshib, Yasaman Ghotbia, Seyed Mahmoud Latific, Ahmadreza Assareha, d
aAhvaz Jundishapur University of Medical Sciences, Ahvaz, Iran
bCardiovascular Research Center, Modarres Hospital, Shahid Beheshti University of Medical Sciences, Tehran, Iran
cHealth Research Institute, Diabetes Research Center, Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran
dCorresponding Author: Ahmadreza Assareh, Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Khouzestan Province, Iran
Manuscript accepted for publication April 05, 2016
Short title: Circulating PTX3 and CR Outcomes
doi: http://dx.doi.org/10.14740/cr462w
| Abstract | ▴Top |
Background: Pentraxin 3 (PTX3) is an inflammatory mediator, reaches to the high levels after ischemic heart diseases (IHD) and could be a helpful tool to predict cardiac rehabilitation (CR) outcomes. The aim of this study was to investigate the possibility of the circulating levels of PTX3 in prediction of CR outcomes in patients with IHD who had undergone coronary artery bypass grafting (CABG).
Methods: One hundred patients who had undergone CABG were included in this study. The CR plan was started 6 weeks after CABG and then PTX3 level, high-sensitivity C-reactive protein (hs-CRP), ejection fraction (EF) and metabolic equivalent (MET) were assessed before and after the CR program. Finally, all gathered data were analyzed using SPSS version 22.
Results: After a 3-month course of CR program, EF, MET, PTX3 and hs-CRP values changed. Statistically significant changes were observed in EF, MET and PTX3 values (P < 0.05) after the CR program and no statistically significant changes were seen in hs-CRP value (P = 0.546) at the end of CR program. Correlations between EF levels and MET with pre-PTX3 levels were also assessed and most changes were observed in the group with pre-PTX3 level more than 0.40 ng/dL.
Conclusion: Our study showed that a regular sufficient CR program based on exercises in IHD patients after CABG increases EF and MET levels, particularly in those patients with pre-PTX3 levels more than 0.40 ng/dL.
Keywords: Pentraxin 3; CABG patients; Cardiac rehabilitation; Ejection fraction; Metabolic equivalent test
| Introduction | ▴Top |
Coronary artery disease (CAD) is one of the most important and frequent agents of morbidity, mortality as well as physical disability, particularly in elderly patients, in developing and even developed countries [1, 2]. It is estimated that almost 50% of all deaths per year in Iran have been attributed to the CAD events [3]. The subsequent CAD events, such as physical dysfunctions, enumerate as a major challenge and thus, the rehabilitation programs could be efficacious in these patients. Cardiac rehabilitation (CR) should be considered as a preventive plan in treatment of CAD patients [4]. Although benefits of CR program based on physical exercises are noteworthy and the program reduces mortality and morbidity due to the CAD phenomena [5], this course almost is expensive, time consuming and non-effective in some cases. However, the eventual inflammatory circulating indicators could be a helpful predicting tool to determine the prognosis of CAD patients. New findings in atherosclerosis inflammation show that long pentraxin 3 (PTX3) is an inflammatory mediator that reaches to high levels after atherosclerosis, occlusion of coronary artery and myocardial infarction (MI) [6-8].
Dendritic cells, macrophages, leukocytes and endothelial cells, especially in heart tissue and vascular system, are the most common sources of PTX3 in the response to the primary inflammation signals [8, 9]. Although some studies have revealed correlations between the levels of PTX3 and CAD [10] and more recently SYNTAX score [11], the association between severity and complexity of CAD and PTX3 levels has not been clearly known yet [6, 12]. Homology in both structure and function of PTX3 with high-sensitivity C-reactive protein (hs-CRP) [13] has led to measurement of PTX3 levels in CAD patients, which is considered as a diagnostic tool. Moreover, the non-specific role of hs-CRP as a diagnostic marker in coronary artery diseases leads to PTX3, which is a specific marker in vascular damages and CAD events, and has attracted more interests recently [14, 15].
However, although studies have shown that habitual aerobic as well as high-intensity exercises could increase the plasma level of PTX3 in healthy subjects [16, 17], a scheduled CR plan based on aerobic exercises can reduce plasma levels of PTX3 in patients with cardiovascular diseases [18].
According to the above subjects, we hypothesized that PTX3 levels may play a predictive role at the beginning of an exercise based CR program to include or exclude patients in the course. To our knowledge, predictive role of the circulating levels of PTX3 as inclusion/exclusion criteria at an exercise based CR program has not been considered so far. Therefore, we aimed to study the levels of PTX3 in patients with ischemic heart disease (IHD), who had undergone coronary artery bypass grafting (CABG) and were enrolled in an exercise based CR program.
| Materials and Methods | ▴Top |
Study population
This study was carried out on the patients seeking care from a referral cardiology hospital, Ahwaz, Iran, from 2012 to 2014. All patients who suffered from IHD and had undergone CABG were enrolled in our study. Inclusion criteria were CABG as well as ability for performing exercise based CR program. High blood pressure, physical disability, ventricular arrhythmia, and the age of patients (elder patients were excluded from study) were considered as exclusion criteria. Blood pressure monitoring and a 12-lead electrocardiogram (ECG) were performed for all patients during physical exercises. A trained interviewer also filled questionnaires consisting of demographic data, smoking status and history of medical situation, using a face-to-face model. Based on pre- and post-PTX3, metabolic equivalent (MET) and EF values, patients were divided into different groups.
Blood samples
All patients who were included in the study rested for 15 min in the sitting position and then blood pressure was taken using a standardized mercury sphygmomanometer. A trained nurse also took two blood samples from all enrolled patients, before and after the scheduled exercise based CR plan. Since a previous study showed that the peripheral levels of PTX3 reflected the sinusoid levels [19], the peripheral blood samples, which were taken from the enrolled patients via the peripheral vain, were placed in the tubes containing EDTA, and were sent to the laboratory for more analyses. All procedures were done in aseptic condition.
Blood analysis
Collected blood samples were centrifuged immediately and stored in -70 °C until use. The PTX3 measurement in plasma was performed using commercial human pentraxin 3 ELISA kit (Cusabio Biotech Co., Japan) according to the previous study [19]. Briefly, standards or samples were added to the microtiter plate well, which were already precoated by specific anti-human PTX3 antibody. Biotin-conjugated specific antibody for PTX3 and avidin conjugated to horseradish peroxidase were added to the wells and then incubated. Finally, substrate solution (3, 3’, 5, 5’tetramethylbenzidine) was added and substrate-enzyme reaction was then terminated by adding sulfuric acid solution. Color changes were measured at a wavelength of 450 nm spectrophotometrically.
Other blood indicators consisting of HDL-C, LDL and hs-CRP were also obtained from the laboratory analysis.
Evaluation of exercises capacity
All enrolled patients in the study started the CR plan 6 weeks after CABG. In the initiate stage, pre-EF and PTX3 for each patient were assessed. As mentioned above, all patients with the dangerous risk factors such as hypotension, ventricular arrhythmias and other risk factors mentioned elsewhere [20] were excluded from the assessment. A fellowship of eco measured EF of patients based on Simpson method.
CR
At the equipped cardiac rehabilitation center, both functional capacity and MET of enrolled patients were evaluated using Duke Activity Status Index (DASI) based on the formula shown in Table 1. Therefore, based on MET of patients, specific exercise plan consisting of treadmill, arm and bicycle was prescribed for each patient. During exercise plan, general conditions of all patients, blood pressure, and pulse rate were monitored precisely.
 Click to view | Table 1. Duke Activity Status Index (DASI) |
The CR program based on physical exercise was then performed according to the Bruce protocol. Blood pressure, 12-lead ECGs and resting heartbeat were obtained before initiating the program. The CR program consisted of 24 sessions in 12 weeks and each week two sessions was carried out. Briefly, the participants started the CR program for 3 min at 1.5 mph speed and in three parts, on treadmill. At the beginning, warming up was initiated as a steady stage for 1 min on treadmill with 5° ascent. At 2 and 3 min, slope degree increased to 10 and 13°, respectively. During the exercise, blood pressure, 12-lead ECGs and heartbeat were obtained. MET as a cardiac peak exercise capacity was also calculated for each patient, before and after the CR program. All information and tests including EF value, exercise tests, blood pressure, ECGs and MET were obtained and evaluated by the same cardiologist. Same laboratory and technician also performed all the laboratory tests such as evaluating PTX3 and the blood indicators.
Statistical analysis
The gathered data were analyzed using SPSS software version 22 for windows. Descriptive data were presented as mean (SD) or median (IQR) for continuous variables with normal and non-normal distribution, respectively. Categorically distributed variables were described in terms of frequency (n, %). A paired t-test was applied for comparison of the results, before and after the CR program. Chi-square and Fisher’s exact tests were also employed for studying the relationship between PTX3 and EF, hs-CRP and MET, before and after the CR program. P-value less than 0.05 was considered to be significant in all analyses.
Ethics
All applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during this research. All participants filled an informed consent and the Ethical Committee of Tehran University of Medical Sciences approved this study. The study protocol conforms to the ethical guidelines of the 2008 Declaration of Helsinki.
| Results | ▴Top |
A total of 100 patients achieved our inclusion criteria and finished the scheduled CR based on physical exercises. Age + SD and women/men (%) of the attended patients were 61.76 + 8.22 and 54%/46%, respectively. All demographic data are summarized in Table 2. The MET and EF values improved and the PTX3 level decreased after the exercise based CR program. Paired t-test statistical analysis showed that after a 3-month course of the CR program, EF, MET, PTX3 and hs-CRP values changed from 31.89+7.65% to 33.88+8.73%, 4.47 + 1.32 MET to 5.16 + 1.96 MET, 0.46 + 0.09 ng/dL to 0.38+0.05 ng/dL and 3.85 + 2.78 mg/dL to 3.72 + 2.61 mg/dL, respectively. None statistically significant changes were seen in the hs-CRP value (P = 0.546) at the end of the CR program but statistically significant changes were observed in the EF value, MET and PTX3 (P < 0.05) after CR program. The statistical data are summarized in Table 3.
 Click to view | Table 2. Demographic Data of the Patients Participated in This Study |
 Click to view | Table 3. Echocardiographic and Circulating Indicators Value of the Patients Before and After the Cardiac Rehabilitation Program |
In order to investigate the possibility of PTX3 influence on the CR program outcomes, the relationship between the EF levels and MET with the pre-PTX3 levels (level of PTX3 before CR program) was also assessed. Resulted PTX3 values were divided to the three groups: less than 0.40 ng/dL, 0.40 - 0.55 ng/dL and more than 0.55 ng/dL. Chi-square and Fisher’s exact tests showed that most of changes in EF and also MET values were observed in the group with pre-PTX3 level more than 0.40 ng/dL while the group with pre-PTX3 less than 0.40 ng/dL incurred few changes compared with other two groups. Most of the beneficial changes were seen in the group with pre-PTX3 between 0.40 and 0.55 ng/dL (Figs. 1 and 2). Changes in the numbers of patients in each EF and MET group based on pre-PTX3 level before and after the exercise based CR program are summarized in Tables 4 and 5.
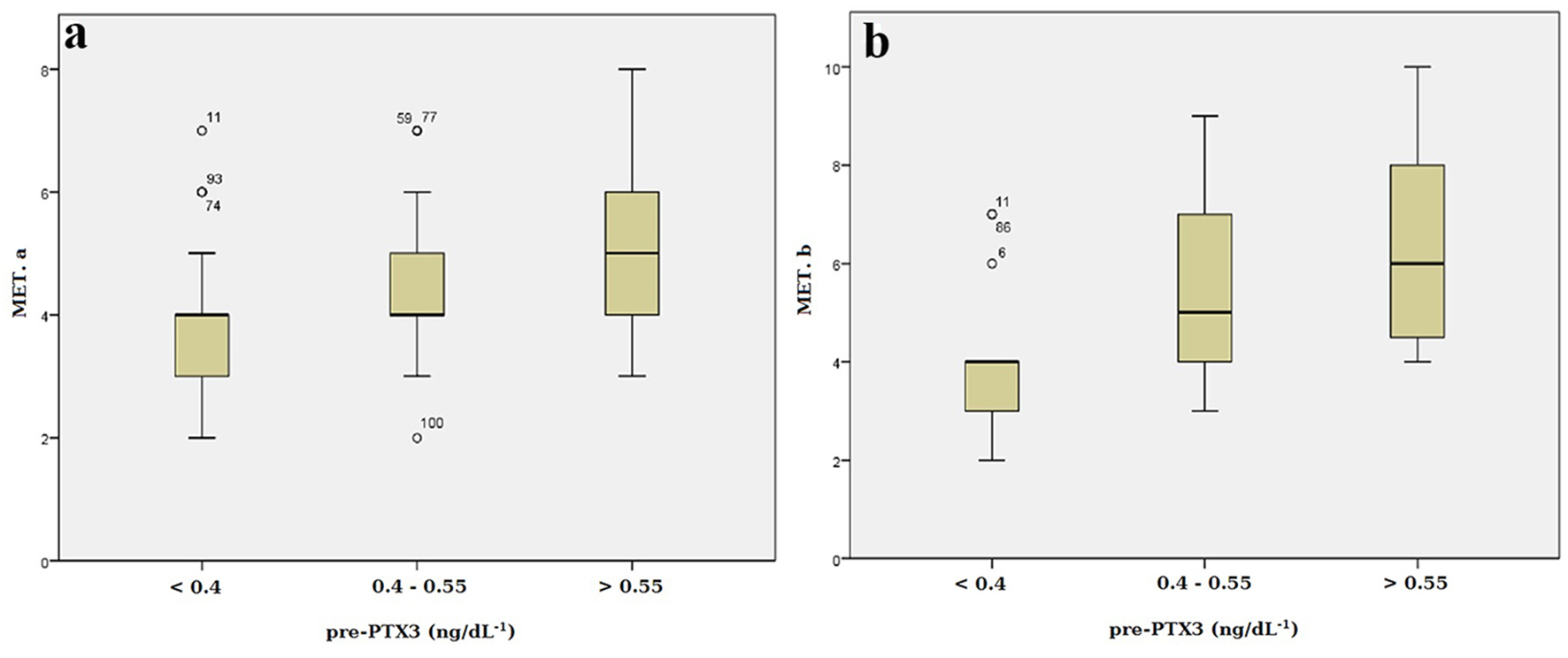 Click for large image | Figure 1. Distribution of MET among the patients undergoing CABG assigned to each PTX3 group. (a) Before cardiac rehabilitation. (b) After cardiac rehabilitation. MET: metabolic equivalent test; CABG: coronary artery bypass grafting; PTX3: pentraxin 3. |
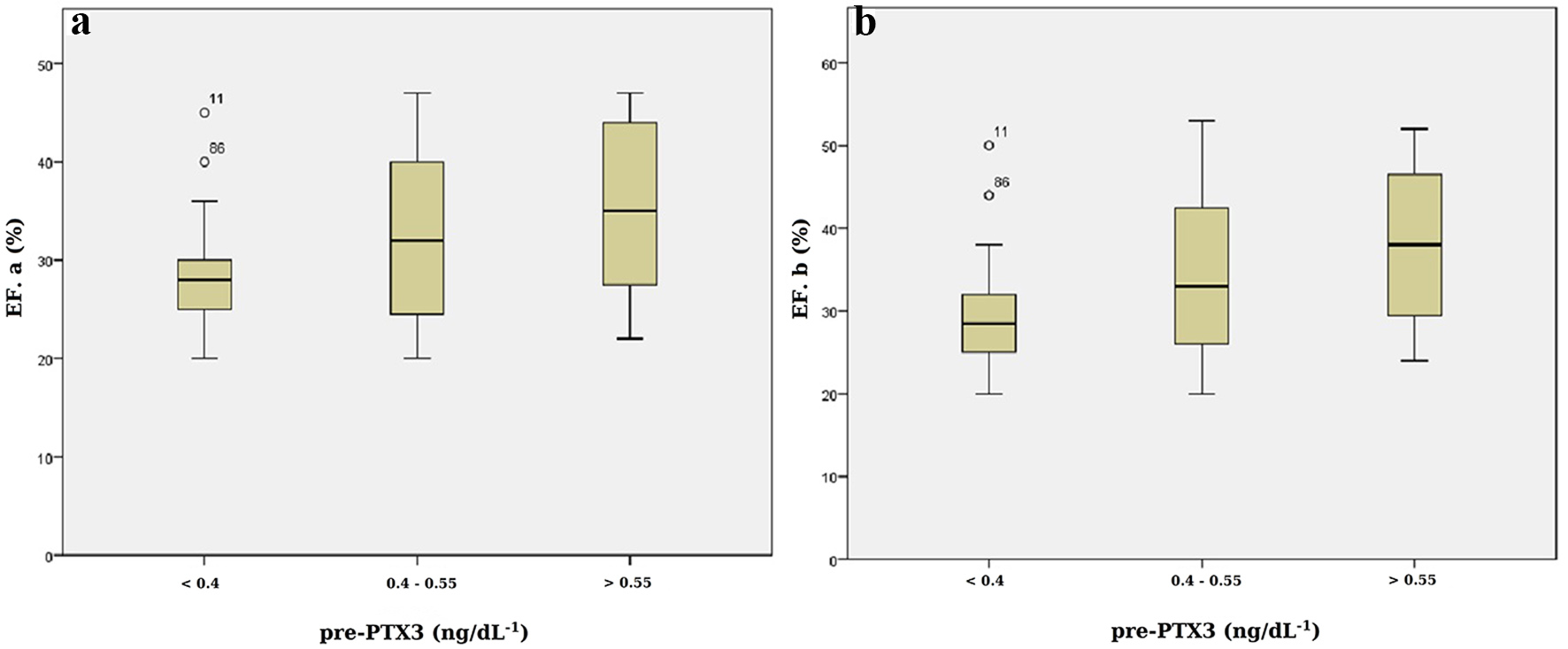 Click for large image | Figure 2. Distribution of EF% among the patients undergoing CABG assigned to each PTX3 group. (a) Before cardiac rehabilitation. (b) After cardiac rehabilitation. EF: ejection fraction; CABG: coronary artery bypass grafting. |
 Click to view | Table 4. The Number of the Patients in Each EF Group Pre- and Post-CR Program Based on Pre-PTX3 Values |
 Click to view | Table 5. The Number of the Patients in Each MET Group Pre- and Post-CR Program Based on Pre-PTX3 Values |
| Discussion | ▴Top |
CAD enumerates a pandemic disease, and improving the post-CAD events is a concern undoubtedly. Many studies have stated physical exercises accompanied with nutritional modification and lifestyle management will reduce resulting complaints of the CAD phenomena [4, 5]. To our knowledge, this is the first study that assessed some remarked inflammatory indicators after CABG in the patients with IHD. In this study, we performed a physical exercise based CR program for patients after CABG and assessed some inflammatory indicators simultaneously.
Few studies have investigated that a CR program elevates the vital capacities such as EF level and MET value. A recent study, which was performed on 140 CAD patients seeking care, showed that physical based CR program improves the EF and MET values [21]. Studies on the effects of CR program on the blood indicators are also rare. A study on 277 patients with coronary heart diseases showed that a 3-month course of a conventional CR program significantly reduces the plasma level of CRP [22]. Another study also showed the reduced levels of the circulating CRP in patients with CABG and acute myocardial infarction (AMI) after a CR program [23]. A study of 223 patients who had CABG and/or valve replacement or repair showed that the CR program reduces the plasma PTX3 levels and increases EF value as well as a 6-min walk test (6MWT) [24].
The EF indication reflects the ability of the cardiac functions. The correlation between a CR program based on physical exercises and improving the EF value seems to be controversial. Despite of this fact that most of the researchers have shown that a programmed physical exercise results in better cardiac function, some others have declared that not any improvement was seen in patients who had EF more than 50% [25]. However, more recently, Sadeghi and colleagues showed that the physical trains in CAD patients could be efficacious on cardiac functions without any side effects in patients [21]. Our study reveals that physical exercises are beneficial in patients with cardiac dysfunction, particularly in those patients with the pre-PTX3 level between 0.40 and 0.55 ng/dL and not in patients with the pre-PTX3 level less than 0.40 ng/dL. This finding suggests a potentially predicting role for PTX3 in inferring the CR outcomes in patients after CABG.
PTX3 regarded as a multifunctional evolutionary conserved protein that beside hs-CRP and serum amyloid P-component (SAP) are derived from pentraxin family [7]. Although both hs-CRP and PTX3 are the inflammatory blood indicators of which functions and structures are similar, the latter has a long N-terminal domain coupled to the C-terminal pentraxin domain and thus, has been known as long pentraxin [9]. PTX3 like hs-CRP has been described as an indicator of inflammation in atherosclerosis and new findings suggest a more prominent role for PTX3 in diagnosis of the progression and the development of atherosclerosis [14, 26]. Indeed, PTX3, compared with hs-CRP, is an acute inflammatory modulator; its level in blood increases rapidly and has different source and gene organization [6, 9].
According to our results, MET value and EF showed significant increased levels in patients with PTX3 level between 0.40 and 0.55 ng/dL compared with those patients with lower PTX3 levels. As some researchers have declared, the circulating PTX3 level might be accompanied with the tense outcomes of acute coronary syndrome [11, 27, 28]. On the other hand, increasing level of circulating PTX3 had been described in MI [28] and thus, a predicting role for the prognosis of patients who had underwent CABG was suggested recently [24].
However, Ferratini et al stated that the high concentration of the plasma PTX3 is likely related to the local activation of inflammation, tissue damage, 6MWT and the CR outcome in patients with cardiac surgery [24]. Recently, Salio and colleagues showed that PTX3-deficient mice after experimental MI had a larger infarct tissue compared with the mice that the PTX3 production was manipulated and thus, they suggested a protective role for PTX3 [29]. The latter study supports our findings that why patients with the pre-PTX level less than 0.40 ng/dL did not have sufficient improvement after the exercise based program while the patients with the PTX3 level between 0.40 and 0.55 ng/dL showed most improvement in both MET and EF indications. However, it seems that circulating levels of PTX3 probably have a protective role as mentioned elsewhere [6], particularly in specific levels.
Many studies have been carried out on the function of PTX3, but the exact role of PTX3 has not been clearly illustrated yet [6, 8, 30]. As available data represent, PTX3 plays an important regulatory role in modulation of the inflammatory response correlated with the atherosclerosis and ischemic cardiovascular events [6, 29, 31]. However, it conceives that increased level of PTX3 acts as a protective physiological response [32], which is correlated to the severity of the disease [33, 34]. This debated role is likely attributed to the better outcomes of MET and EF after the exercise based CR program, particularly in those patients with the pre-circulating levels of PTX3 more than 0.40 ng/dL. Some studies have shown high concentration of circulating PTX3 in patients with chronic kidney diseases (CKD) [33, 35] and it seems that high concentration of PTX3 influences endothelial functions [36]. Therefore, high concentration of PTX3 could be associated with endothelial functions in CAD patients, CR program outcomes and increased mortality risk as well [34].
Peri and colleagues showed that the PTX3 levels in plasma elevate after 6 - 8 h and are not correlated with CRP. They also showed that almost 75% of patients at the time of discharging after the AMI event had abnormal levels of hs-CRP while the level of PTX3 was normal [15]. Our findings are in agreement with the mentioned study and no relationship was seen between hs-CRP and the pre-PTX levels. Non-reducing levels of hs-CRP after the CR program are probably related to dilatory nature of hs-CRP that reaches to the peak level after blood circulating PTX3.
However, our findings elucidate a potential role for PTX3 as an indication to include/exclude CABG patients in an exercise based CR program. This probable role can reduce expenditure of patients and governments as well as prescribe suitable care plan for patients. Therefore, designing studies on structure and function of PTX3 will clear the value of this interesting biomarker to estimate CR program outcomes, particularly in CAD patients.
Limitation of the study
To increase the precision of our study, we needed to include further patients surly. But unfortunately, in this study, we did not have adequate facilities for great population. Indeed, considering several exclusion criteria, the sample size was decreased. However, we investigated the plausible role of an interesting inflammation blood-circulating biomarker to predict CR program outcomes and future studies will be required for deep cognition of this interesting biomarker.
Conclusion
In conclusion, our study showed that a regular and sufficient exercise based CR program in IHD patients after CABG could increase EF and MET levels, particularly in the patients with pre-PTX3 levels more than 0.40 ng/dL.
Acknowledgement
The authors would like to appreciate Mrs. Molouk Salemzadeh and Niloufar Karimi for laboratory cooperation as well as Imam Khomeini hospital for providing samples. We also thank Dr. Hamed Mirjalali for editing the manuscript.
Conflict of Interest
The authors declare that there is no conflict of interests regarding the publication of this paper.
Funding
There are no funding sources for publication of this paper.
| References | ▴Top |
- Lim GB. Global burden of cardiovascular disease. Nat Rev Cardiol. 2013;10(2):59.
doi pubmed - Pinsky JL, Jette AM, Branch LG, Kannel WB, Feinleib M. The Framingham Disability Study: relationship of various coronary heart disease manifestations to disability in older persons living in the community. Am J Public Health. 1990;80(11):1363-1367.
doi pubmed - Hatmi ZN, Tahvildari S, Gafarzadeh Motlag A, Sabouri Kashani A. Prevalence of coronary artery disease risk factors in Iran: a population based survey. BMC Cardiovasc Disord. 2007;7:32.
doi pubmed - Taylor RS, Brown A, Ebrahim S, Jolliffe J, Noorani H, Rees K, Skidmore B, et al. Exercise-based rehabilitation for patients with coronary heart disease: systematic review and meta-analysis of randomized controlled trials. Am J Med. 2004;116(10):682-692.
doi pubmed - Giannuzzi P, Temporelli PL, Corra U, Tavazzi L. Antiremodeling effect of long-term exercise training in patients with stable chronic heart failure: results of the Exercise in Left Ventricular Dysfunction and Chronic Heart Failure (ELVD-CHF) Trial. Circulation. 2003;108(5):554-559.
doi pubmed - Norata GD, Garlanda C, Catapano AL. The long pentraxin PTX3: a modulator of the immunoinflammatory response in atherosclerosis and cardiovascular diseases. Trends Cardiovasc Med. 2010;20(2):35-40.
doi pubmed - Mantovani A, Garlanda C, Bottazzi B, Peri G, Doni A, Martinez de la Torre Y, Latini R. The long pentraxin PTX3 in vascular pathology. Vascul Pharmacol. 2006;45(5):326-330.
doi pubmed - Garlanda C, Bottazzi B, Moalli F, Deban L, Molla F, Latini R, Mantovani A. Pentraxins and atherosclerosis: the role of PTX3. Curr Pharm Des. 2011;17(1):38-46.
doi pubmed - Du Clos TW. Pentraxins: structure, function, and role in inflammation. ISRN Inflamm. 2013;2013:379040.
doi pubmed - Karakas MF, Buyukkaya E, Kurt M, Motor S, Akcay AB, Buyukkaya S, Karakas E, et al. Serum pentraxin 3 levels are associated with the complexity and severity of coronary artery disease in patients with stable angina pectoris. J Investig Med. 2013;61(2):278-285.
pubmed - Namazi MH, Saadat H, Safi M, Vakili H, Alipourparsa S, Bozorgmanesh M, Haybar H. Pentraxin 3 Is Highly Specific for Predicting Anatomical Complexity of Coronary Artery Stenosis as Determined by the Synergy between Percutaneous Coronary Intervention with Taxus and Cardiac Surgery Score. Korean Circ J. 2014;44(4):220-226.
doi pubmed - Knoflach M, Kiechl S, Mantovani A, Cuccovillo I, Bottazzi B, Xu Q, Xiao Q, et al. Pentraxin-3 as a marker of advanced atherosclerosis results from the Bruneck, ARMY and ARFY Studies. PLoS One. 2012;7(2):e31474.
doi pubmed - Rolph MS, Zimmer S, Bottazzi B, Garlanda C, Mantovani A, Hansson GK. Production of the long pentraxin PTX3 in advanced atherosclerotic plaques. Arterioscler Thromb Vasc Biol. 2002;22(5):e10-14.
doi pubmed - Jenny NS, Arnold AM, Kuller LH, Tracy RP, Psaty BM. Associations of pentraxin 3 with cardiovascular disease and all-cause death: the Cardiovascular Health Study. Arterioscler Thromb Vasc Biol. 2009;29(4):594-599.
doi pubmed - Peri G, Introna M, Corradi D, Iacuitti G, Signorini S, Avanzini F, Pizzetti F, et al. PTX3, A prototypical long pentraxin, is an early indicator of acute myocardial infarction in humans. Circulation. 2000;102(6):636-641.
doi pubmed - Miyaki A, Maeda S, Choi Y, Akazawa N, Tanabe Y, Ajisaka R. Habitual aerobic exercise increases plasma pentraxin 3 levels in middle-aged and elderly women. Appl Physiol Nutr Metab. 2012;37(5):907-911.
doi pubmed - Nakajima T, Kurano M, Hasegawa T, Takano H, Iida H, Yasuda T, Fukuda T, et al. Pentraxin3 and high-sensitive C-reactive protein are independent inflammatory markers released during high-intensity exercise. Eur J Appl Physiol. 2010;110(5):905-913.
doi pubmed - Fukuda T, Kurano M, Iida H, Takano H, Tanaka T, Yamamoto Y, Ikeda K, et al. Cardiac rehabilitation decreases plasma pentraxin 3 in patients with cardiovascular diseases. Eur J Prev Cardiol. 2012;19(6):1393-1400.
doi pubmed - Haybar H, Assareh A, Ghotbi Y, Torabizadeh M, Bozorgmanesh M. Incremental diagnostic value of circulating pentraxin in patients with intermediate risk of coronary artery disease. Heart. 2013;99(9):640-648.
doi pubmed - Chaitman BR. Exercise Stree Testing. In: Bonow RO, Mann DL, Zipes DP, Libby P, eds. Braunwald's Heart disease: A textbook of cardiovascular medicine. 9 ed. Philadelphia: WB Saunders; 2012:168-200.
- Sadeghi M, Garakyaraghi M, Taghavi M, Khosravi M, Sarrafzadegan N, Roohafza H. The Impacts of Cardiac Rehabilitation Program on Exercise Capacity, Quality of Life, and Functional Status of Coronary Artery Disease Patients with Left Ventricular Dysfunction. Rehabil Nurs. 2015;40(5):305-309.
doi pubmed - Milani RV, Lavie CJ, Mehra MR. Reduction in C-reactive protein through cardiac rehabilitation and exercise training. J Am Coll Cardiol. 2004;43(6):1056-1061.
doi pubmed - Pluss CE, Karlsson MR, Wallen N, Billing E, Held C. Effects of an expanded cardiac rehabilitation programme in patients treated for an acute myocardial infarction or a coronary artery by-pass graft operation. Clin Rehabil. 2008;22(4):306-318.
doi pubmed - Ferratini M, Ripamonti V, Masson S, Grati P, Racca V, Cuccovillo I, Raimondi E, et al. Pentraxin-3 predicts functional recovery and 1-year major adverse cardiovascular events after rehabilitation of cardiac surgery patients. J Cardiopulm Rehabil Prev. 2012;32(1):17-24.
doi pubmed - Kim C, Kim DY, Lee DW. The impact of early regular cardiac rehabilitation program on myocardial function after acute myocardial infarction. Ann Rehabil Med. 2011;35(4):535-540.
doi pubmed - Inoue K, Sugiyama A, Reid PC, Ito Y, Miyauchi K, Mukai S, Sagara M, et al. Establishment of a high sensitivity plasma assay for human pentraxin3 as a marker for unstable angina pectoris. Arterioscler Thromb Vasc Biol. 2007;27(1):161-167.
doi pubmed - Savchenko A, Imamura M, Ohashi R, Jiang S, Kawasaki T, Hasegawa G, Emura I, et al. Expression of pentraxin 3 (PTX3) in human atherosclerotic lesions. J Pathol. 2008;215(1):48-55.
doi pubmed - Latini R, Maggioni AP, Peri G, Gonzini L, Lucci D, Mocarelli P, Vago L, et al. Prognostic significance of the long pentraxin PTX3 in acute myocardial infarction. Circulation. 2004;110(16):2349-2354.
doi - Salio M, Chimenti S, De Angelis N, Molla F, Maina V, Nebuloni M, Pasqualini F, et al. Cardioprotective function of the long pentraxin PTX3 in acute myocardial infarction. Circulation. 2008;117(8):1055-1064.
doi pubmed - Garlanda C, Hirsch E, Bozza S, Salustri A, De Acetis M, Nota R, Maccagno A, et al. Non-redundant role of the long pentraxin PTX3 in anti-fungal innate immune response. Nature. 2002;420(6912):182-186.
doi pubmed - Norata GD, Marchesi P, Pulakazhi Venu VK, Pasqualini F, Anselmo A, Moalli F, Pizzitola I, et al. Deficiency of the long pentraxin PTX3 promotes vascular inflammation and atherosclerosis. Circulation. 2009;120(8):699-708.
doi pubmed - Deban L, Jarva H, Lehtinen MJ, Bottazzi B, Bastone A, Doni A, Jokiranta TS, et al. Binding of the long pentraxin PTX3 to factor H: interacting domains and function in the regulation of complement activation. J Immunol. 2008;181(12):8433-8440.
doi pubmed - Tong M, Carrero JJ, Qureshi AR, Anderstam B, Heimburger O, Barany P, Axelsson J, et al. Plasma pentraxin 3 in patients with chronic kidney disease: associations with renal function, protein-energy wasting, cardiovascular disease, and mortality. Clin J Am Soc Nephrol. 2007;2(5):889-897.
doi pubmed - Dubin R, Li Y, Ix JH, Shlipak MG, Whooley M, Peralta CA. Associations of pentraxin-3 with cardiovascular events, incident heart failure, and mortality among persons with coronary heart disease: data from the Heart and Soul Study. Am Heart J. 2012;163(2):274-279.
doi pubmed - Dubin R, Shlipak M, Li Y, Ix J, de Boer IH, Jenny N, Peralta CA. Racial differences in the association of pentraxin-3 with kidney dysfunction: the Multi-Ethnic Study of Atherosclerosis. Nephrol Dial Transplant. 2011;26(6):1903-1908.
doi pubmed - Yilmaz MI, Sonmez A, Ortiz A, Saglam M, Kilic S, Eyileten T, Caglar K, et al. Soluble TWEAK and PTX3 in nondialysis CKD patients: impact on endothelial dysfunction and cardiovascular outcomes. Clin J Am Soc Nephrol. 2011;6(4):785-792.
doi pubmed
This is an open-access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cardiology Research is published by Elmer Press Inc.


