| Cardiology Research, ISSN 1923-2829 print, 1923-2837 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, Cardiol Res and Elmer Press Inc |
| Journal website https://www.cardiologyres.org |
Original Article
Volume 14, Number 4, August 2023, pages 302-308
Evaluation of Physicians’ Compliance With Secondary Prevention Among Ischemic Stroke Patients: A Retrospective Study
Alaa Alhubaishia , Maha A. Almutairib
, Malak A. Alasqahb
, Shihanah H. Alharthib
, Abdulhadi M. Alqahtanic
, Lina I. Alnajjara, d
aDepartment of Pharmacy Practice, College of Pharmacy, Princess Nourah bint Abdulrahman University, Riyadh 11671, Saudi Arabia
bCollage of Pharmacy, Princess Nourah Bint Abdulrahman University, Riyadh, Saudi Arabia
cClinical Research Department, Research Center, King Fahad Medical City, Riyadh, Saudi Arabia
dCorresponding Author: Lina I. Alnajjar, Department of Pharmacy Practice, College of Pharmacy, Princess Nourah bint Abdulrahman University, PO Box 84428, Riyadh 11671, Saudi Arabia
Manuscript submitted March 23, 2023, accepted June 9, 2023, published online July 12, 2023
Short title: Secondary Prevention in IS
doi: https://doi.org/10.14740/cr1500
| Abstract | ▴Top |
Background: Stroke is a leading cause of disability and death worldwide. Globally, stroke affects 13.7 million individuals every year. Several studies have shown an increase in the rehospitalization rate among stroke patients caused by non-adherence to secondary prevention as recommended by the American Heart Association/American Stroke Association (AHA/ASA) guideline. The aim of this study was to evaluate physicians’ compliance with secondary prevention of stroke upon patients’ discharge.
Methods: A retrospective chart review study was conducted at King Fahad Medical City. The primary outcome of this study was the number of patients discharged with the recommended medications for the secondary prevention of ischemic stroke (IS). The data were collected from the patient’s medical record files and analyzed using the Statistical Package for the Social Sciences (SPSS).
Results: Of the 675 patients who were screened for eligibility, 507 were included and 168 were excluded. The mean age of the patients was 59.5 (± 15.6) years. Of the 507 patients, 181 (35.7%) had a history of previous stroke. Overall, 376 (74%) stroke patients were discharged with appropriate secondary prevention recommendation per AHA/ASA guideline.
Conclusions: This study stresses the importance of compliance with the AHA/ASA guideline for secondary stroke prevention and highlights the role of pharmacists in the stroke unit in which it is necessary to ensure that all stroke patients are discharged with the recommended medications to reduce recurrent stroke.
Keywords: Stroke; Secondary prevention; Physician compliance; Ischemic stroke; Transient ischemic stroke
| Introduction | ▴Top |
Stroke affects 13.7 million individuals globally every year and is the cause of death for around 5.5 million individuals annually [1]. Stroke occurs in one out of every four people over the age of 25. While men have a higher risk of ischemic stroke (IS) than women at a younger age, women have a higher mortality rate. Locally, in Saudi Arabia, stroke is the second contributor to mortality, according to data reported by the World Health Organization (WHO) [2]. It occurs in 57.64 per 1,00,000 individuals every year and IS has the highest prevalence rate of 65.6% among other types of strokes [3].
The American Heart Association/American Stroke Association (AHA/ASA) defined stroke as an infraction in the spinal cord and brain, or retinal cell death due to ischemia, as indicated by the imaging, pathological, or objective evidence of central nervous system (CNS) infraction in a specified vascular distribution or the clinical evidence of CNS infraction as indicated by symptoms extending for ≥ 24 h or until death. Stroke can be categorized into three main categories: hemorrhagic, ischemic, or transient ischemic attack (TIA). IS defined as a neurological disorder affected by a CNS infraction [4], while TIA is a transient episode of neurological dysfunction induced by the spinal cord, focal brain, or retinal ischemia without acute infarction [4]. Risk factors for IS can be described as nonmodifiable, such as age and race, or modifiable, such as cigarette smoking, hypertension (HTN), diabetes mellitus (DM), dyslipidemia, atrial fibrillation (AF), and physical inactivity.
After IS managed urgently, AHA/ASA provides recommendations for secondary prevention, which includes pharmacological and non-pharmacological options (Table 1). Pharmacological options are mediation, such as β-hydroxy β-methyl glutaryl-CoA (HMG-CoA) reductase inhibitors known as statins and antiplatelet or anticoagulation therapy. This is recommended for all IS patients unless they are contraindicated. In addition, it is critical to control other comorbidities that can contribute to a new incidence of stroke, such as HTN, DM and dyslipidemia. Non-pharmacological options can improve overall health and reduce the risk factors of stroke, including physical activity, a healthy lifestyle, weight reduction, and smoking cessation [5].
 Click to view | Table 1. Recommended Secondary Prevention Medications for Ischemic Stroke per AHA/ASA Guideline |
Several studies have shown an increase in the rehospitalization rate among IS patients caused by not adhering to the guideline recommendations for secondary stroke prevention. Studies have found a decline in the rehospitalization rate of stroke patients as they followed the guideline recommendations [6-10]. According to a retrospective cohort study, patients who were discharged after IS with secondary stroke prevention therapies in the short and long term will help reduce the risk of recurrent stroke [10].
The aim of this study was to evaluate the physician’s adherence to secondary prevention of IS by determining the number of patients discharged from stroke units with appropriate secondary prevention medications recommended by AHA/ASA.
| Materials and Methods | ▴Top |
Study design and setting
A retrospective chart review study was conducted in one of the largest hospitals in the Riyadh region, which includes 460 beds. The targeted population was adult patients admitted to the stroke unit with a confirmed IS or TIA diagnosis. All patients were followed up from admission to discharge between January 2019 and December 2020.
Ethical issues and informed consent
The study was approved by the Institutional Review Board (IRB) at the King Fahad Medical City (KFMC) Research Center (IRB number 21-380), and the need for informed consent was waived. The study was conducted in accordance with the Declaration of Helsinki, and before the analysis, the patients’ information was anonymized and de-identified.
Study participants
Patients older than 18 years and admitted to the stroke unit with confirmed IS or TIA were eligible for inclusion. Patients were excluded if they were diagnosed with hemorrhagic stroke, pregnant, discharged against medical advice, or if the stroke was medically ruled out (Fig. 1).
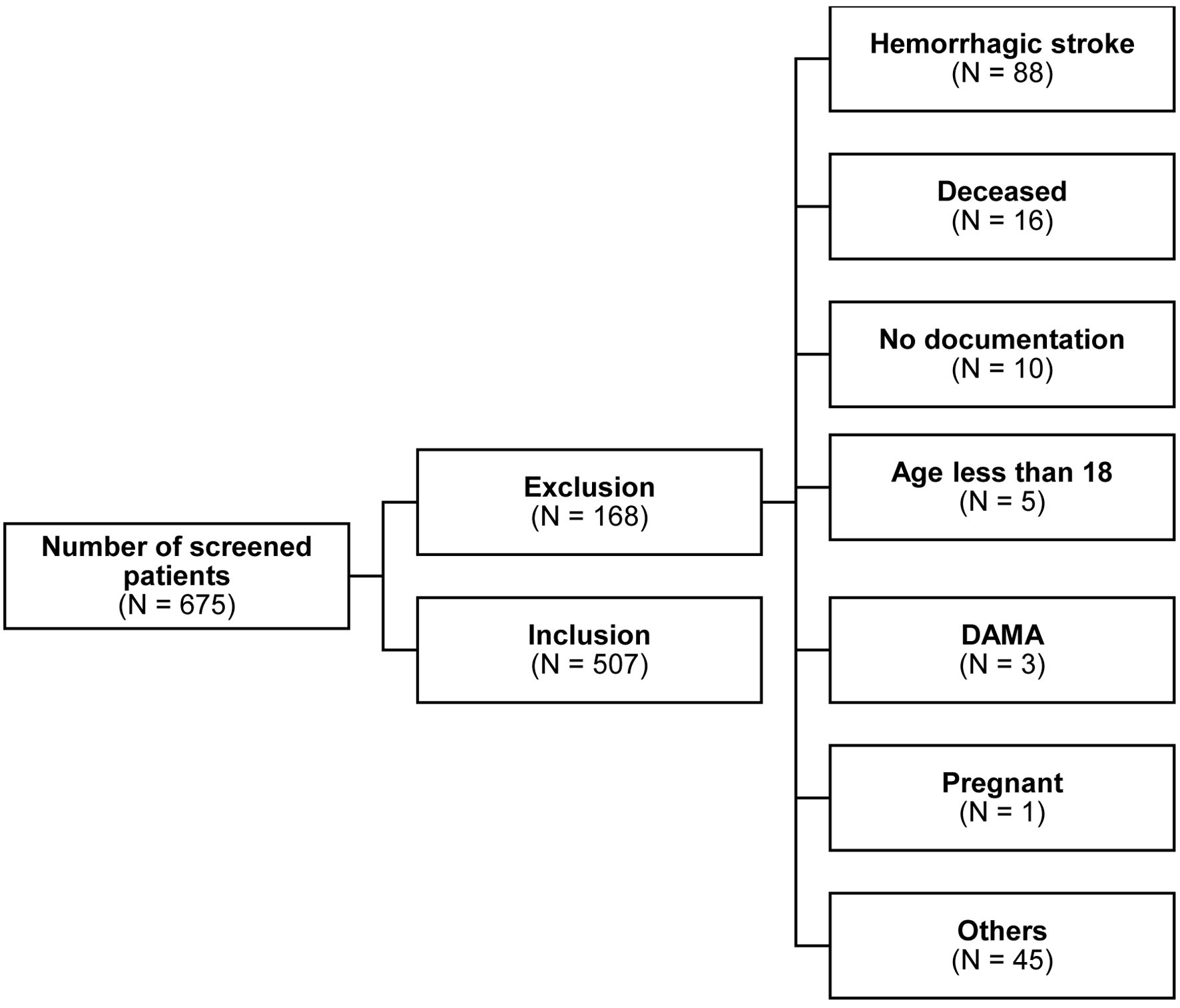 Click for large image | Figure 1. Flowchart of patients admitted to the stroke unit. Others were patients who were suspected of having IS or TIA but without any confirmed medical diagnosis. DAMA: discharged against medical advice; IS: ischemic stroke; N: number; TIA: transient ischemic attack. |
Study variables
The study data were collected and managed using a Microsoft Excel sheet. All patient data were obtained from the stroke unit at KFMC. The data included the patients’ demographics, medical history, date of admission and discharge, diagnosis type of stroke, number of prior strokes, laboratory results, and discharged medication. The primary outcome was the number of stroke patients discharged with appropriate secondary prevention. The medications of focus were the recommended secondary prevention medications based on the AHA/ASA guideline, which include antiplatelets or anticoagulants, statins, and other medications to manage high-risk comorbidities that can lead to stroke (Table 1). All patients’ discharged medication lists were reviewed and compared with AHA/ASA guideline recommended medications.
Statistical analysis
All data analyses were performed using the Statistical Package for the Social Sciences (SPSS) version 25. Since the study was a descriptive retrospective study, the data variables were expressed using descriptive statistics ether by percentage, mean ± standard deviation (SD), median, or average. The source data were validated using Pearson correlation, and the association was very strong (Pearson correlation = 1.0).
| Results | ▴Top |
A total of 675 patients were screened for eligibility, and 507 IS patients met our inclusion criteria in the final analysis sample. The exclusion criteria included patients who were diagnosed with hemorrhagic stroke (88, 52.3%), passed during hospitalization (16, 9.5%), were less than 18 years old (5, 2.9%), were pregnant (1, 0.5%), had no documentation in electronic medical records (EMR) (10, 5.9%), were discharged against medical advice (3, 1.7%), and were suspected to have IS or TIA, with no confirmed medical diagnosis (45, 26.7%) (Fig. 1).
Demographics and clinical characteristics
As demonstrated in Table 2, most patients were male (63% versus 37.2% female) with a mean age of 59.5 ± 15.6 years. HTN was the most common past medical history in IS patients (398, 76.7%), followed by DM (311, 61.3%), obesity (191, 37.7%), ischemic heart disease (129, 25.4%), dyslipidemia (124, 24.5%), AF (49, 9.7%), chronic kidney disease (42, 8.3%), and seizures (73, 14.5%). A total of 181 (35.7%) patients in this study had a history of stroke before study enrolment: about 150 patients had one previous stroke, 30 patients had 2 - 4 stroke incidences, and one patient had more than five stroke events in his life. About 20 (17.8%) patients were currently smokers, and 64 (12.6%) were former smokers.
 Click to view | Table 2. Patients’ Demographic Characteristics |
Number of patients discharged with IS secondary prevention
Out of 507 IS patients, only 376 (74%) were discharged with complete recommended secondary prevention per guideline, which includes medications that prevent recurrent stroke and medications that manage other comorbidities that increase the risk of stroke. Moreover, 131 (26%) patients missed complete appropriate recommendations.
During admission, about 13 patients (2.5%) developed AF, which was the most prevalent new diagnosis comorbidity, followed by HTN (12, 2.3%), then DM (8, 1.5%). The majority of patients diagnosed with new comorbidities that increase the risk of recurrent stroke were discharged on appropriate medications (Table 3). However, not all patients with past medical history of comorbidities other than stroke have been discharged on their medications (Table 3). A high number of patients (469, 92.5%) were discharged on statin, 409 (80.6%) were discharged on antiplatelet, and 146 (28.7%) were discharged on anticoagulant. The types of antiplatelet or anticoagulation are detailed in Table 4. Nicotine replacement therapy was prescribed only for 20 out of 90 smokers in the study, and there were no documented recommendations for weight loss in obese patients.
 Click to view | Table 3. Number of Patients Discharged on Medications to Manage Comorbidities (Diagnosed During Admission) |
 Click to view | Table 4. Number of Patients Discharged on Medications to Manage Comorbidities (Past Medical History) |
| Discussion | ▴Top |
According to the AHA/ASA guideline, all IS or TIA patients should be discharged with antiplatelet therapy, either single or dual antiplatelet therapy (DAPT), depending on the patients’ case, high-intensity statin to prevent secondary vascular events, including stroke, and anticoagulant medication depending on the conditions associated with the embolic IS. Antiplatelet therapy is recommended for all IS patients unless contraindicated. This study showed a high number of patients discharged on antiplatelets (409, 80.7%) (Table 5) and 98 (19.3%) did not. The reason may be due to medical contraindication, such as severe bleeding or high sensitivity to antiplatelet medication. However, there was no documentation behind not recommending antiplatelets for the rest of the patients. A similar study found that 32 out of 275 stroke patients were discharged with no antiplatelet therapy [9]. In addition, the guideline recommended that DAPT should not exceed 90 days and should not be combined with anticoagulant medication, as recent trials have shown that there is no benefit over single antiplatelet therapy to reduce recurrent stroke, in addition to increasing the risk of major bleeding and intracerebral hemorrhagic stroke [11, 12]. Accordingly, in this study, about 46 patients had DAPT for longer than 90 days and six patients had a combination of DAPT and an anticoagulant without a clear indication of which was against the AHA/ASA guideline.
 Click to view | Table 5. Total Number of All Patients Discharged on Complete Ischemic Stroke Secondary Prevention |
Individuals with AF have a 3 - 5 times greater risk of IS. Direct oral anticoagulant (DOAC) is recommended for non-valvular AF and warfarin for valvular AF as lifetime management for the secondary prevention of IS unless contraindicated. A total of 49 patients had a history of AF, and 13 patients were newly diagnosed during admission. Moreover, 11 patients were not discharged on anticoagulants, probably which might be due to contraindication as high-risk hemorrhage, but this was not documented. However, this study had a lower percentage of physician noncompliance compared to another study, which mentioned that 1,756 out of 6,273 IS patients with a history of AF were discharged without anticoagulant therapy [13].
As for high-intensity statin, about 469 (92.5%) statins were prescribed upon discharge, while 38 (7.5%) IS patients were not discharged with any kind of statin. Although this study saw a higher rate of statin prescription, a retrospective, cross-sectional study found that only five patients out of 105 IS patients were not discharged with a statin [7]. On the other hand, a population-based survey study reported that 321 out of 931 IS patients were discharged with a statin, which was significantly low compared to this study [14]. Some patients found that the side effect of statin as rhabdomyolysis was unbearable. Here comes the importance of pharmacists, as they will suggest some strategies to manage the side effects of statins while using them.
In addition to the above medications, AHA/ASA guidelines recommend managing other comorbidities that increase the risk of stroke, such as HTN, diabetes, and AF. Lifestyle modifications, including physical activity, healthy diet, weight reduction in the case of obesity, and smoking cessation, are highly recommended by the guideline [15].
We found that across all patients who were admitted for stroke or TIA, cases were better managed when a new comorbidity was diagnosed during admission which indicate better practice at this cite. About 31 patients developed new comorbidities in which the majority were discharged on medications (Table 3). Incomplete secondary prevention medication on discharge was higher in patients with a past medical history of health conditions that increase the risk of stroke. However, vital signs confirmed uncontrolled HTN in 31 patients, and laboratory results showed A1C more than 7% in 36 diabetic patients and AF in eight patients (Table 4). Moreover, patients were not prescribed the necessary medications on discharge. This could be related to the physicians’ perception that the primary care physician would take the lead in prescribing the needed medications. If so, this practice exposes these patients to a higher risk of recurrent stroke sooner than expected. About 181 IS patients had a history of stroke (Table 2), which may be the result of not adhering to the guideline recommendation previously or of the patient not complying with their medication. Either way, there was no clear document about recurrent stroke history because some patients did not have the electronic record for their first-time stroke, as they had a stroke around 10 years ago, which was most likely managed in a different hospital.
HTN is the most critical risk factor for the development of stroke [15]. Therefore, ensuring that all patients with HTN are discharged with hypertensive medication is important to prevent recurrent IS. Overall, 378 out of 398 HTN patients were discharged with antihypertensive medications (Table 5). This study had higher patient compliance rates with antihypertensive medications compared with a similar study that found that 23 out of 116 IS patients with HTN were not prescribed antihypertensive medication at discharge [16].
Diabetic patients are twice more at risk of stroke than non-diabetic patients. About 283 out of 311 patients were discharged with antidiabetic medication, which leaves about 28 patients who were discharged with no medications although their A1C was higher than 7%, which indicates the need to manage medication according to the guideline to reduce the recurrence of IS. This might be due to the lack of pharmacists in the stroke unit since we could not find any documentation on why antidiabetic patients were not prescribed on discharge.
Regarding lifestyle modification, in this study, there were 191 (37.7%) obese patients with an average body mass index (BMI) of 30.3 kg/m2. Unfortunately, there was no mention of a weight loss plan for those patients in their records. Regarding smoking, continuing to smoke after a stroke is associated with a higher risk of stroke recurrence and other cardiovascular events [17]. In this study, there were 90 (17.8%) smokers. However, only 20 (22.2%) patients had a prescription for nicotine replacement therapy. This also emphasizes the role of a pharmacist in the stroke unit, as a meta-analysis concluded that stroke patients who smoked had an increased risk of recurrent stroke, with a pooled odds ratio (OR) of 1.61 (95% confidence interval (CI): 1.34 - 1.93, P < 0.001) [18].
This study demonstrated that about 376 (74%) IS or TIA patients were discharged with complete secondary prevention, while 131 (26%) patients were not discharged with the recommended medication for secondary stroke prevention.
Our study emphasizes the crucial role of pharmacists in stroke units. A systematic review concluded that pharmacist involvement in a stroke unit positively impacts stroke patient outcomes [17]. Another study found that clinical pharmacists in a stroke unit were able to identify 22.6% of 796 patients with untreated indications and 21% of patients with noncompliance [19].
For these purposes, it is recommended that pharmacists should be included in the stroke unit team for better outcomes.
There were some limitations to our study. First was the nature of the retrospective design in which data were based on patient records only. Second, some patients with past medical history were treated in other hospitals, and there was an obstacle in understanding the reasons behind the lack of management of comorbidities before admission that might have contributed to the cause of their current stroke.
Conclusions
Physician adherence to the guideline recommendations for secondary stroke prevention must be optimized. Comorbidity management, such as prescribing HTN, DM, and AF medications, is vital to reducing stroke recurrence. The presence of a pharmacist in a stroke unit is essential to ensure that stroke patients are discharged with the recommended medication according to recent guidelines that help reduce stroke recurrence. Future studies need to assess the impact of pharmacists’ role in reducing the number of recurrent IS and recommending appropriate secondary prevention.
Acknowledgments
None to declare.
Financial Disclosure
This research was supported by Princess Nourah bint Abdulrahman University Researchers Supporting Project number (PNURSP2023R351), Princess Nourah bint Abdulrahman University, Riyadh, Saudi Arabia.
Conflict of Interest
The authors declare that they have no conflict of interest.
Informed Consent
Not applicable. IRB clearance was provided for this study.
Author Contributions
AA has conceived of the presented idea, involved in planning, and reviewed the manuscript. AMA has verified the analytical methods, involved in planning, and supervised the research. MAA, MAA, and SHA have contributed to the design and implementation of the research, to the analysis of the results and to the writing of the manuscript. LIA has contributed to the writing of the manuscript, to the final editing and review. All authors were involved in writing, reviewing, and revising the article prior to submission.
Data Availability
The authors declare that data supporting the findings of this study are available within the article.
Abbreviations
AF: arterial fibrillation; AHA/ASA: American Heart Association/American Stroke Association; BMI: body mass index; CNS: central nervous system; DAPT: dual antiplatelet therapy; DM: diabetes mellitus; DOAC: direct oral anticoagulant; HTN: hypertension; IQR: interquartile range; IRB: Institutional Review Board; KFMC: King Fahad Medical City; SD: standard deviation; SPSS: Statistical Package for the Social Sciences; TIA: transient ischemic attack; WHO: World Health Organization
| References | ▴Top |
- Lindsay MP, Norrving B, Sacco RL, Brainin M, Hacke W, Martins S, Pandian J, et al. World Stroke Organization (WSO): global stroke fact sheet 2019. Int J Stroke. 2019;14(8):806-817.
doi pubmed - Donkor ES. Stroke in the 21(st) century: a snapshot of the burden, epidemiology, and quality of life. Stroke Res Treat. 2018;2018:3238165.
doi pubmed pmc - Basri R, Issrani R, Hua Gan S, Prabhu N, Khursheed Alam M. Burden of stroke in the Kingdom of Saudi Arabia: A soaring epidemic. Saudi Pharm J. 2021;29(3):264-268.
doi pubmed pmc - Sacco RL, Kasner SE, Broderick JP, Caplan LR, Connors JJ, Culebras A, Elkind MS, et al. An updated definition of stroke for the 21st century: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2013;44(7):2064-2089.
doi pubmed - Meschia JF, Bushnell C, Boden-Albala B, Braun LT, Bravata DM, Chaturvedi S, Creager MA, et al. Guidelines for the primary prevention of stroke: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2014;45(12):3754-3832.
doi pubmed pmc - Tamayo-Ojeda C, Parellada-Esquius N, Salvador-Gonzalez B, Oriol-Toron PA, Rodriguez-Garrido MD, Munoz-Segura D, en representacion del grupo de investigacion del p. [Compliance with recommendations in secondary prevention of stroke in primary care]. Aten Primaria. 2017;49(6):351-358.
doi pubmed pmc - Eissa A, Krass I, Bajorek BV. Use of medications for secondary prevention in stroke patients at hospital discharge in Australia. Int J Clin Pharm. 2014;36(2):384-393.
doi pubmed - Harewood-Marshall AS, Craig LS, Martelly TP, Corbin DOC, Maul L, McIntosh-Clarke D, Blackman T, et al. Managing acute ischaemic stroke in a small island developing state: meeting the guidelines in Barbados. BMC Public Health. 2018;18(1):648.
doi pubmed pmc - Al Qawasmeh M, Alhusban A, Alfwaress F, El-Salem K. An assessment of patients factors effect on prescriber adherence to ischemic stroke secondary prevention guidelines. Curr Rev Clin Exp Pharmacol. 2021;16(1):97-102.
doi pubmed - Tsai JP, Rochon PA, Raptis S, Bronskill SE, Bell CM, Saposnik G. A prescription at discharge improves long-term adherence for secondary stroke prevention. J Stroke Cerebrovasc Dis. 2014;23(9):2308-2315.
doi pubmed - Investigators SPS, Benavente OR, Hart RG, McClure LA, Szychowski JM, Coffey CS, Pearce LA. Effects of clopidogrel added to aspirin in patients with recent lacunar stroke. N Engl J Med. 2012;367(9):817-825.
doi pubmed pmc - Johnston SC, Easton JD, Farrant M, Barsan W, Conwit RA, Elm JJ, Kim AS, et al. Clopidogrel and aspirin in acute ischemic stroke and high-risk TIA. N Engl J Med. 2018;379(3):215-225.
doi pubmed pmc - Basaran O, Dogan V, Biteker M, Karadeniz FO, Tekkesin AI, Cakilli Y, Turkkan C, et al. Guideline-adherent therapy for stroke prevention in atrial fibrillation in different health care settings: Results from RAMSES study. Eur J Intern Med. 2017;40:50-55.
doi pubmed - Nilsson G, Samuelsson E, Soderstrom L, Mooe T. Low use of statins for secondary prevention in primary care: a survey in a northern Swedish population. BMC Fam Pract. 2016;17(1):110.
doi pubmed pmc - Kleindorfer DO, Towfighi A, Chaturvedi S, Cockroft KM, Gutierrez J, Lombardi-Hill D, Kamel H, et al. 2021 guideline for the prevention of stroke in patients with stroke and transient ischemic attack: a guideline from the American Heart Association/American Stroke Association. Stroke. 2021;52(7):e364-e467.
doi pubmed - Doogue R, McCann D, Fitzgerald N, Murphy AW, Glynn LG, Hayes P. Blood pressure control in patients with a previous stroke/transient ischaemic attack in primary care in Ireland: a cross sectional study. BMC Fam Pract. 2020;21(1):139.
doi pubmed pmc - Basaraba JE, Picard M, George-Phillips K, Mysak T. Pharmacists as care providers for stroke patients: a systematic review. Can J Neurol Sci. 2018;45(1):49-55.
doi pubmed - Pan B, Jin X, Jun L, Qiu S, Zheng Q, Pan M. The relationship between smoking and stroke: A meta-analysis. Medicine (Baltimore). 2019;98(12):e14872.
doi pubmed pmc - Semcharoen K, Supornpun S, Nathisuwan S, Kongwatcharapong J. Characteristic of drug-related problems and pharmacists' interventions in a stroke unit in Thailand. Int J Clin Pharm. 2019;41(4):880-887.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cardiology Research is published by Elmer Press Inc.


