| Cardiology Research, ISSN 1923-2829 print, 1923-2837 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, Cardiol Res and Elmer Press Inc |
| Journal website https://www.cardiologyres.org |
Original Article
Volume 14, Number 3, June 2023, pages 228-236
In-Hospital and One-Year Outcomes of Transcatheter Aortic Valve Replacement in Patients Requiring Supplemental Home Oxygen Use
Haris Pataila, f , Ritika Kompellaa, Nicole E. Hooverb, Wyona Reisb, Rohit Masihc, Jeff F. Matherd, Trevor S. Suttone, Raymond G. McKayb
aDepartment of Internal Medicine, University of Connecticut School of Medicine, Farmington, CT, USA
bDepartment of Cardiology, Hartford Hospital, Hartford, CT, USA
cDepartment of Internal Medicine, Hartford Hospital, Hartford, CT, USA
dDepartment of Research Administration, Hartford Hospital, Hartford, CT, USA
eIntegrated Anesthesia Associates, Hartford Hospital, Hartford, CT, USA
fCorresponding Author: Haris Patail, Department of Internal Medicine, University of Connecticut School of Medicine, Farmington, CT 06030, USA
Manuscript submitted March 15, 2023, accepted April 28, 2023, published online May 26, 2023
Short title: Home O2 TAVR
doi: https://doi.org/10.14740/cr1497
| Abstract | ▴Top |
Background: There have been limited reports with inconsistent results on the impact of long-term use of oxygen therapry (LTOT) in patients treated with transcatheter aortic valve replacement (TAVR).
Methods: We compared in-hospital and intermediate TAVR outcomes in 150 patients requiring LTOT (home O2 cohort) with 2,313 non-home O2 patients.
Results: Home O2 patients were younger, and had more comorbidities including chronic obstructive pulmonary disease (COPD), diabetes, carotid artery disease, lower forced expiratory volume (FEV1) (50.3±21.1% vs. 75.0±24.7%, P < 0.001), and lower diffusion capacity (DLCO, 48.6±19.2% vs. 74.6±22.4%, P < 0.001). These differences represented higher baseline Society of Thoracic Surgeons (STS) risk score (15.5±10.2% vs. 9.3±7.0%, P < 0.001) and lower pre-procedure Kansas City Cardiomyopathy Questionnaire (KCCQ-12) scores (32.5 ± 22.2 vs. 49.1 ± 25.4, P < 0.001). The home O2 cohort required higher use of alternative TAVR vascular access (24.0% vs. 12.8%, P = 0.002) and general anesthesia (51.3% vs. 36.0%, P < 0.001). Compared to non-home O2 patients, home O2 patients showed increased in-hospital mortality (5.3% vs. 1.6%, P = 0.001), procedural cardiac arrest (4.7% vs. 1.0%, P < 0.001), and postoperative atrial fibrillation (4.0% vs. 1.5%, P = 0.013). At 1-year follow-up, the home O2 cohort had a higher all-cause mortality (17.3% vs. 7.5%, P < 0.001) and lower KCCQ-12 scores (69.5 ± 23.8 vs. 82.1 ± 19.4, P < 0.001). Kaplan-Meir analysis revealed a lower survival rate in the home O2 cohort with an overall mean (95% confidence interval (CI)) survival time of 6.2 (5.9 - 6.5) years (P < 0.001).
Conclusion: Home O2 patients represent a high-risk TAVR cohort with increased in-hospital morbidity and mortality, less improvement in 1-year KCCQ-12, and increased mortality at intermediate follow-up.
Keywords: TAVR; Aortic stenosis; COPD; Home oxygen; Long-term oxygen therapy; Chronic lung disease
| Introduction | ▴Top |
The beneficial use of ambulatory and home oxygen for chronic obstructive pulmonary disease (COPD) and other forms of chronic lung disease has been well established for decades, where it has shown to improve physiological and functional outcomes for indicated patients [1]. Long-term use of oxygen therapy (LTOT) has shown to improve overall outcomes with patients who have profound hypoxemia (PaO2 < 55 mm Hg) or hypoxemia with objective evidence of cor pulmonale [2-4]. In this setting, supplemental oxygen use has been shown to improve dyspnea, cognitive impairment, exercise tolerance, quality of life (QOL), and overall mortality [1, 2, 5, 6].
Prior studies have demonstrated that LTOT is an independent predictor of adverse outcomes in patients with severe aortic stenosis (AS) who are treated with surgical aortic valve replacement (SAVR), with an increased incidence of respiratory complications, pneumonia, and short-term and long-term mortality [7, 8]. Owing to the less invasive nature of percutaneous valve replacement with less duration of mechanical ventilation and alternative availability of a minimalist approach with use of local/regional anesthesia and conscious sedation, some reports have postulated transcatheter aortic valve replacement (TAVR) as the more optimal approach in patients with severe chronic lung disease [9, 10]. There is controversy, however, over the risk of TAVR morbidity and mortality specifically in the LTOT patient subgroup.
To date, there have been limited reports on TAVR outcomes in patients requiring LTOT. Several studies have identified LTOT as an independent predictor of in-hospital and 1-year TAVR mortality, procedural futility, and unplanned hospital readmission [11-14]. Alternatively, a recent 2021 study by Kumar et al demonstrated no impact of home oxygen use on intermediate survival and clinical outcomes with a mean follow-up time of 2.3 years [15]. Given these results, the purpose of the present study was to compare in-hospital and intermediate clinical outcomes in patients on LTOT versus those that did not require oxygen therapy in a large volume TAVR center. We hypothesized that LTOT patients would represent a high-risk TAVR cohort with an increased in-hospital and 1-year morbidity and mortality.
| Materials and Methods | ▴Top |
Setting and design
This was a retrospective, observational study which was conducted at an 890-bed tertiary-care medical center, Hartford Hospital, in Hartford, Connecticut. The Institutional Review Board approved the study, meeting the criteria for a waiver of the requirement to obtain informed consent. This study was conducted in compliance with the ethical standards of the responsible institution on human subjects as well as with the Helsinki Declaration.
Study population
From a total cohort of 2,463 TAVR patients treated at our institution since 2012, we assessed in-hospital and intermediate outcomes in 150 patients requiring home O2 compared to 2,313 non-home O2 patients. All home O2 patients were on LTOT during the pre-TAVR evaluation and during the index TAVR hospital admission. All patients underwent evaluation by a multidisciplinary valve committee with a pre-procedure review of cardiac catheterization, echocardiographic, multi-slice computed tomography angiogram (CTA), and pulmonary function testing (PFT) data to document the severity of AS and suitability for TAVR. Baseline Society of Thoracic Surgeons (STS)-predicted risk of 30-day mortality (PROM) as well as incremental risk assessment based upon functional assessment including frailty, severe pulmonary and hepatic disease, porcelain aorta, and hostile mediastinum was determined for all patients. Pre-procedure QOL was assessed with baseline Kansas City Cardiomyopathy Questionnaires (KCCQ-12). The decision for valve choice and TAVR access route for each patient was made by the treating cardiothoracic surgeon and interventional cardiologist.
TAVR procedure
All TAVR procedures were performed in a hybrid catheterization laboratory using conscious sedation or general anesthesia with either transthoracic or transesophageal echocardiographic imaging. Standard techniques for implantation of balloon-expandable and self-expandable valves from either femoral or alternative access sites were employed. A temporary pacemaker was implanted either by a jugular or femoral vein access, and radial or femoral arterial access was used for pigtail aortography guidance. Following initial valve deployment, post-dilation was performed in all patients who demonstrated greater than mild paravalvular aortic regurgitation by echocardiography or aortography.
In-hospital outcomes
Home O2 and non-home O2 cohorts were compared regarding baseline demographic data, cardiovascular risk factors, comorbidities, prior cardiac history, preoperative cardiac catheterization, echocardiogram findings, CTA results, PFT results, STS PROM, KCCQ-12 score, and procedural details. In addition, the two cohorts were compared for total length of hospital stay (LOS), post-procedure LOS, all-cause mortality, conversion to open-heart surgery, procedural cardiac arrest, transient ischemic attack (TIA), ischemic stroke, new-onset atrial fibrillation, major and minor vascular complications, composite bleeding, new requirements for dialysis, and need for permanent pacemaker implantation. Composite bleeding was defined as a combination of access site bleeding, hematoma at the access site, retroperitoneal bleeding, gastrointestinal bleeding, and genitourinary bleeding. All analyzed data were obtained from an institutional TAVR database prospectively maintained by the hospital’s cardiovascular quality department and queries from the institutional electronic medical record database (EPIC). All data elements were defined according to the Society of Thoracic Surgeons/American College of Cardiology Transcatheter Valve Therapy Registry (STS/ACC TVT Registry), and all adverse outcomes reported were in accordance with the Valve Academic Research Consortium (VARC-3) definitions [16].
Clinical follow-up outcomes
Clinical follow-up was assessed in all patients based on the analysis of post-discharge visits recorded in the electronic medical record and by telephone interviews with the patient or referring physician. Home O2 and non-home O2 cohorts were compared with respect to 1-year all-cause mortality, KCCQ-12 score, and hospital readmission. In addition, a Kaplan-Meier survival analysis was performed comparing the two groups up to 10 years post-TAVR.
Statistical analysis
Continuous variables are expressed as mean ± standard deviation (SD) or median (interquartile range) and were compared with a Student’s t-test or the Mann-Whitney U test, respectively. Categorical variables were analyzed using the Chi-square test or Fisher’s exact test. Post-hoc Bonferroni corrections were applied to adjust for multiple comparisons. Event rates were generated using the Kaplan-Meier method, and log-rank tests were used for group comparisons. Logistic regression was used to determine independent predictors of 1-year all-cause mortality in all patients. Univariate analysis was performed to identify variables to be entered into the logistic regression model, where the cut-off for model entry was set at P < 0.05. Pre-TAVR variables entered into the model including home O2, age, gender, body mass index, creatinine, diabetes, hypertension, atrial fibrillation, peripheral arterial disease, moderate/severe COPD, New York Heart Association (NYHA) III or IV heart failure, left ventricular ejection fraction, and STS risk score.
All effects were considered significant at P < 0.05. The statistical analyses were performed with SPSS 21.0 (SPSS, Chicago, Illinois).
| Results | ▴Top |
Baseline clinical characteristics
Baseline demographics, cardiovascular risk factors, prior cardiac history, and comorbidities for home O2 and non-home O2 patients are summarized in Table 1. The home O2 cohort was younger, had a larger body surface area, a lower incidence of prior coronary artery bypass grafting (CABG), and a greater prevalenvce of COPD, diabetes, and carotid artery disease. These differences translated into a higher STS risk score for the home O2 cohort (15.5±10.2% vs. 9.3±7.0%, P < 0.001). In addition, home O2 patients had a lower baseline KCCQ-12 score (32.5 ± 22.2 vs. 49.1 ± 25.4, P < 0.001) (Table 1).
 Click to view | Table 1. Baseline Clinical Characteristics |
Pre-TAVR testing results
Table 2 lists baseline echocardiographic, cardiac catheterization, CTA, and PFT results for home O2 and non-home O2 patients. There was no significant difference between the two cohorts with respect to pre-procedure echocardiographic, cardiac catheterization, and CTA annulus size findings. Home O2 patients had a lower forced expiratory volume (FEV1) and diffusion capacity (DLCO) on pulmonary function testing (Table 2).
 Click to view | Table 2. Pre-TAVR Laboratory Testing |
Procedural characteristics
As described in Table 3, home O2 patients required higher use of alternative TAVR vascular access (24.0% vs. 12.8%, P = 0.002) with greater use of general anesthesia (55.3% vs. 44.0%, P < 0.001). There were no differences between the two groups with respect to type of TAVR valve implanted, contrast use, or fluoroscopy time (Table 3).
 Click to view | Table 3. Procedural Characteristics |
In-hospital outcomes
Compared to non-home O2 patients, home O2 patients showed increased in-hospital mortality, procedural cardiac arrest, and postoperative atrial fibrillation. In addition, the home O2 cohort had longer total LOS, as well as a long post-TAVR LOS (Table 4).
 Click to view | Table 4. Comparison of In-Hospital Clinical Outcomes Between Home O2 and Non-Home O2 Cohorts |
Clinicl follow-up
At 1-year follow-up, the home O2 cohort had a higher all-cause mortality and lower KCCQ-12 score, with no difference in hospital readmission compared to non-home O2 patients. Of the 26 home O2 patients that expired within the first year, the causes of death were identified as cardiac in seven patients and non-cardiac in 19 patients. Total days spent in the hospital, inclusive of the index TAVR admission and hospital re-admissions, did not differ between home O2 and non-home O2 patients (median days (interquartile range): home O2 7.0 (5.0 - 15.5) versus non-home O2 7.0 (3.0 - 13.0), P = 0.17) (Table 5, Fig. 1).
 Click to view | Table 5. Comparison of 1-Year Clinical Outcomes Between Home O2 and Non-Home O2 Cohorts |
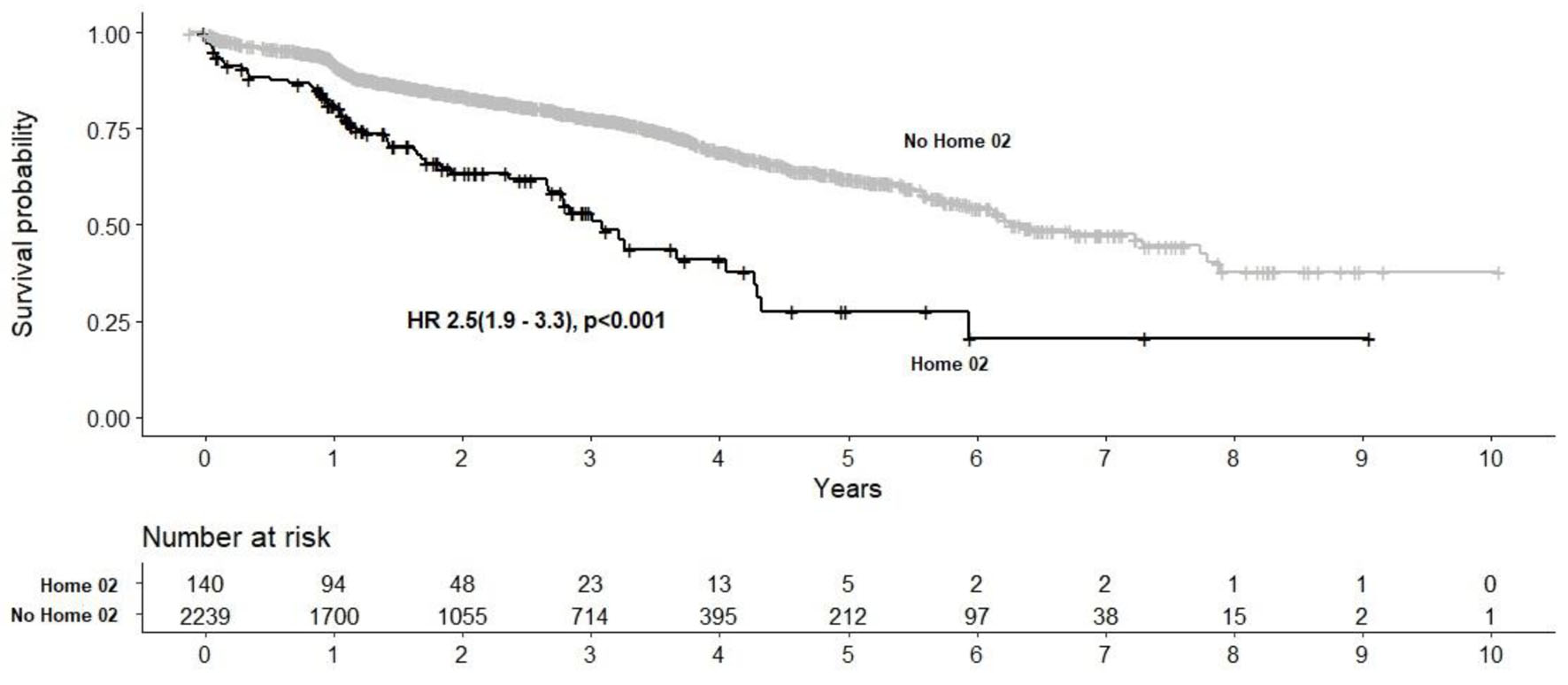 Click for large image | Figure 1. Kaplan-Meier survival analysis post-TAVR in home O2 and non-home O2 cohorts. TAVR: transcatheter aortic valve replacement. |
Multivariate logistic regression predictors of 1-year mortality included STS risk score (odds ratio (OR): 1.04; 95% confidence interval (CI): 1.02 - 1.06, P < 0.001), pre-TAVR atrial fibrillation (OR: 2.40; 95% CI: 1.73 - 3.33, P < 0.001), moderate/severe COPD (OR: 1.47; 95% CI: 1.03 - 2.08, P = 0.031) and NYHA III/IV (OR: 1.53; 95% CI 1.07 - 2.18, P = 0.019). Home O2 use was borderline significant after adjustment for these additional variables (OR: 1.74; 95% CI: 0.99 - 3.04, P = 0.050.)
Figure 1 demonstrates a Kaplan-Meir survival analysis showing a significant increase in all cause mortality in the home O2 cohort with an overall mean (95% CI) survival time of 6.2 (5.9 - 6.5) years (P < 0.001).
| Discussion | ▴Top |
The results of this study demonstrate four important findings. First, patients with chronic lung disease who use LTOT and require evaluation for aortic valve (AV) replacement for severe AS represent a high-risk cohort with an increased burden of cardiovascular risk factors and clinical comorbidities. These findings translate into an elevated STS risk score and a lower KCCQ-12 score. Second, despite the availability of TAVR with less duration of mechanical ventilation and alternative use of conscious sedation, a significant percentage of home O2 patients required general anesthesia for non-femoral alternative vascular access, obviating any theoretical clinical benefit of a minimalist approach. Third, in comparison to non-home O2 TAVR patients, home O2 patients experience increased hospital morbidity, with an increase in procedural cardiac arrest, postoperative atrial fibrillation and LOS, and a more than three-fold increase in in-hospital mortality. Finally, home O2 patients have a higher mortality and lower improvement of QOL at 1-year follow-up, with Kaplan-Meir survival analysis showing increased all-cause mortality up to 10 years post-procedure.
The results of this study are in agreement with prior TAVR reports demonstrating LTOT as an independent predictor of poor short- and intermediate-term outcomes. In a 2016 report by Hermiller et al examing outcomes in 3,687 high- and extreme-risk patients from the Medtronic CoreValve US Pivotal Trial program, home oxygen use was an independent predictor of both 30-day and 1-year all-cause mortality [12]. In a 2018 report from the STS/ACC TVT Registry examining 30-day outcomes in 21,661 TAVR patients, multivariate logistic regression identified home oxygen use as an independent predictor of death [11]. Simialrly, in another STS/ACC TVT report from 2020 examing outcomes in 10,345 patients, home oxygen use was an independent predictor of 30-day unplanned hospital readmission [13]. Finally, in a 2021 report from Geisler et al examing outcomes from a single-center registry, home oxygen use was an independent predictor of procedural futility [14].
In contrast, the current study differs from a recent 2021 report by Kumar et al detailing similar intermediate survival outcomes between home O2 and non-home O2 TAVR patients with a mean follow-up of 2.3 years [15]. Notably, this report does not include baseline patient demographics, PFT testing, anesthetic use, in-hospital outcomes, and changes in QOL from both cohorts. In addition, the pre-TAVR STS risk scores for home O2 and non-home O2 patients measured 6.9% and 5.3%, respectively, indicating lower risk subsets compared to the present report.
Coincident with the growth of TAVR and its approval by the US Food and Drug Administration in all patient risk categories, there has been increasing referrals of patients with severe lung disease for percutaneous valve replacement rather than SAVR. As the third leading cause of death in the United States and a condition that affects around 5% of the general population, COPD is a common comorbidity identified in patients presenting with severe AS who require AV replacement. Prior studies have documented a COPD incidence of approximately 20% in patients referred for SAVR and an incidence ranging between 12.5% and 43.4% for patients treated with TAVR [17]. Moreover, in a 2019 study by Kwak et al examing referral trends described in the National Inpatient Sample, the rate of TAVR among COPD patients has been steadily increasing nationally since 2011 [18]. The presumed basis for this referral increase is related to prior reports demonstrating improved outcomes in the TAVR COPD cohort, with decreases in reintubation, tracheostomy, pneumonia, acute kidney injury, acute myocardial infarction, bleeding requiring transfusion, and overall mortality compared to the SAVR group [18, 19]. Despite these reports, however, COPD remains a well documented risk factor for adverse TAVR outcomes. In addition, the current report suggests that COPD patients requiring LTOT represent a more advanced stage of disease severity with an even higher risk of TAVR morbidity and mortality.
An important factor cited as the basis for improved TAVR outcomes in patients with severe lung disease is anesthetic technique with more favorable outcomes associated with conscious sedation versus general anesthesia. For the general TAVR population, prior reports on the use of anesthesia have shown a benefit of conscious sedation with local anesthesia compared to general anesthesia with respect to procedural duration, faster recovery, shorter intensive care unit and hospital LOS, avoidance of postoperative delirium, and 30-day mortality [20]. Monitored anesthesia care (MAC) with use of conscious sedation has emerged as a critical component of the “minimalist TAVR technique” allowing for earlier patient mobilization and discharge. For patients with severe lung disease, the utilization of regional versus general anesthesia for procedures including carotid endarterectomy, total knee arthroplasty, total hip arthroplasty, and open inguinal hernia repair in COPD has been associated with a lower incidence of pulmonary complications [21]. With respect to TAVR, a 2017 study by Condado et al demonstrated that a minimalist approach with conscious sedation results in less resource utilization and improved 1-year survival compared to general anesthesia in patients with severe COPD [10]. Similarly, in a 2021 study by Serkan et al, the use of conscious sedation compared with general anesthesia was associated with lower incidence of respiratory-related complications and a shorter intensive care unit (ICU) LOS [22]. An important limitation of these studies is that patients were treated with transfemoral TAVR rather than alternative vascular access. In the current study, 24% of patients required alternative vascular access with either transcarotid, subclavian, direct aortic, or transapical approaches. While MAC has been successfully documented in a minority of patients undergoing both transcarotid [23] and subclavian [24] procedures, all intrathoracic (e.g., transapical, direct aortic) and the vast majority of extrathoracic alternative access procedures are currently performed under general anesthesia, obviating any theoretical benefit of a minimalist approach.
Limitations
This study is inherently limited by its retrospective nature, single-center experience, inability to perform randomization, and the relatively small sample size of the home O2 cohort. Second, the wide disparity between home O2 and non-home O2 patients with respect to age, cardiovascular risk factors, comorbidities, STS risk score, and vascular access did not allow for meaningful propensity matching between the two groups. Finally, while all home O2 patients required oxygen therapy prior to and during their TAVR hospital admission, we were not able to report on the requirement of LTOT following valve replacement.
Conclusion
In this single-center retrospective study, LTOT in TAVR patients was associated with increased in-hospital and intermediate all-cause mortality compared to non-home O2 patients. Home O2 patients experienced higher rates of procedural cardiac arrest and postoperative atrial fibrillation, with significantly less improvement of QOL at 1-year follow-up. Potential beneficial use of a minimalist approach with conscious sedation in this patient cohort was offset with an increased need for non-femoral alternative vascular access requiring use of general anesthesia. Additional studies are warranted to further investigate the optimal treatment of LTOT patients with severe AS and to guide physicians in their treatment recommendation of TAVR, SAVR, or medical palliation.
Acknowledgments
None to declare.
Financial Disclosure
None to declare.
Conflict of Interest
None to declare.
Informed Consent
The Institutional Review Board approved the study, meeting the criteria for a waiver of the requirement to obtain informed consent.
Author Contributions
Haris Patail: conceptualization, validation, formal analysis, writing (review and editing). Ritika Kompella, Nicole E. Hoover, Wyona Reis, Rohit Masih, and Trevor S. Sutton: formal analysis, investigation, writing (review and editing). Jeff F. Mather: methodology, software, validation, formal analysis, data curation, visualization. Raymond G. McKay: conceptualization, methodology, validation, formal analysis, writing (original draft), writing (review and editing), supervision.
Data Availability
The data supporting the findings of this study are available from the corresponding author upon reasonable request.
Abbreviations
AS: aortic stenosis; AV: aortic valve; BMI: body mass index; BSA: body surface area; CABG: coronary artery bypass grafting; COPD: chronic obstructive pulmonary disease; CTA: computed tomography angiogram; DLCO: diffusion capacity; FEV1: forced expiratory volume; home O2: home oxygen; KCCQ-12: Kansas City Cardiomyopathy Questionnaire; LTOT: long-term use of oxygen therapy; LOS: length of stay; MAC: monitored anesthesia care; MI: myocardial infarction; NYHA: New York Heart Association; PCI: percutaneous coronary intervention; PROM: predicted risk of mortality; QOL: quality of life; SAVR: surgical aortic valve replacement; STS: Society of Thoracic Surgeons; TIA: transient ischemic attack; TAVR: transcatheter aortic valve replacement
| References | ▴Top |
- Criner GJ. Ambulatory home oxygen: what is the evidence for benefit, and who does it help? Respir Care. 2013;58(1):48-64.
doi pubmed - Katsenos S, Constantopoulos SH. Long-term oxygen therapy in COPD: factors affecting and ways of improving patient compliance. Pulm Med. 2011;2011:325362.
doi pubmed pmc - Celli BR, MacNee W, Force AET. Standards for the diagnosis and treatment of patients with COPD: a summary of the ATS/ERS position paper. Eur Respir J. 2004;23(6):932-946.
doi pubmed - Oswald-Mammosser M, Weitzenblum E, Quoix E, Moser G, Chaouat A, Charpentier C, Kessler R. Prognostic factors in COPD patients receiving long-term oxygen therapy. Importance of pulmonary artery pressure. Chest. 1995;107(5):1193-1198.
doi pubmed - Thakur N, Blanc PD, Julian LJ, Yelin EH, Katz PP, Sidney S, Iribarren C, et al. COPD and cognitive impairment: the role of hypoxemia and oxygen therapy. Int J Chron Obstruct Pulmon Dis. 2010;5:263-269.
doi pubmed pmc - Dilektasli AG, Porszasz J, Stringer WW, Casaburi R. Physiologic effects of oxygen supplementation during exercise in chronic obstructive pulmonary disease. Clin Chest Med. 2019;40(2):385-395.
doi pubmed - Dvir D, Waksman R, Barbash IM, Kodali SK, Svensson LG, Tuzcu EM, Xu K, et al. Outcomes of patients with chronic lung disease and severe aortic stenosis treated with transcatheter versus surgical aortic valve replacement or standard therapy: insights from the PARTNER trial (placement of AoRTic TraNscathetER Valve). J Am Coll Cardiol. 2014;63(3):269-279.
doi pubmed - Huckaby LV, Aranda-Michel E, Sultan I, Chu D, Chen S, Thoma F, Kilic A. Outcomes in patients with severe chronic lung disease undergoing index cardiac operations. Ann Thorac Surg. 2021;112(2):481-486.
doi pubmed pmc - Konia MR, Helmer G, Raveendran G, Aposolidou I. Anesthetic implications of chronic lung disease in patients undergoing transcatheter valve implantation. J Cardiothorac Vasc Anesth. 2017;31(2):657-662.
doi pubmed - Condado JF, Haider MN, Lerakis S, Keegan P, Caughron H, Thourani VH, Devireddy C, et al. Does minimalist transfemoral transcatheter aortic valve replacement produce better survival in patients with severe chronic obstructive pulmonary disease? Catheter Cardiovasc Interv. 2017;89(4):775-780.
doi pubmed - Hermiller JB, Jr., Yakubov SJ, Reardon MJ, Deeb GM, Adams DH, Afilalo J, Huang J, et al. Predicting early and late mortality after transcatheter aortic valve replacement. J Am Coll Cardiol. 2016;68(4):343-352.
doi pubmed - Arnold SV, O'Brien SM, Vemulapalli S, Cohen DJ, Stebbins A, Brennan JM, Shahian DM, et al. Inclusion of functional status measures in the risk adjustment of 30-day mortality after transcatheter aortic valve replacement: a report from the Society of Thoracic Surgeons/American College of Cardiology TVT Registry. JACC Cardiovasc Interv. 2018;11(6):581-589.
doi pubmed pmc - Sanchez CE, Hermiller JB, Jr., Pinto DS, Chetcuti SJ, Arshi A, Forrest JK, Huang J, et al. Predictors and risk calculator of early unplanned hospital readmission following contemporary self-expanding transcatheter aortic valve replacement from the STS/ACC TVT registry. Cardiovasc Revasc Med. 2020;21(3):263-270.
doi pubmed - Geisler D, Rudzinski PN, Hasan W, Andreas M, Hasimbegovic E, Adlbrecht C, Winkler B, et al. Identifying patients without a survival benefit following transfemoral and transapical transcatheter aortic valve replacement. J Clin Med. 2021;10(21):4911.
doi pubmed pmc - Kumar K, Morris CC, Samhan A, Herman T, Chau T, Lantz G, Chadderdon SM, et al. Intermediate-term outcomes following transcatheter aortic valve implantation in patients with a history of supplemental home oxygen use. Am J Cardiol. 2022;167:159-160.
doi pubmed - Varc-3 Writing C, Genereux P, Piazza N, Alu MC, Nazif T, Hahn RT, Pibarot P, et al. Valve academic research consortium 3: updated endpoint definitions for aortic valve clinical research. J Am Coll Cardiol. 2021;77(21):2717-2746.
doi pubmed - Liao YB, He ZX, Zhao ZG, Wei X, Zuo ZL, Li YJ, Xiong TY, et al. The relationship between chronic obstructive pulmonary disease and transcatheter aortic valve implantation—A systematic review and meta-analysis. Catheter Cardiovasc Interv. 2016;87(Suppl 1):570-578.
doi pubmed - Kwak MJ, Bhise V, Warner MT, Balan P, Nguyen TC, Estrera AL, Smalling RW, et al. National trend of utilization, clinical and economic outcomes of transcatheter aortic valve replacement among patients with chronic obstructive pulmonary disease. Curr Med Res Opin. 2019;35(8):1321-1329.
doi pubmed - Ando T, Adegbala O, Akintoye E, Ashraf S, Pahuja M, Briasoulis A, Takagi H, et al. Is transcatheter aortic valve replacement better than surgical aortic valve replacement in patients with chronic obstructive pulmonary disease? A nationwide inpatient sample analysis. J Am Heart Assoc. 2018;7(7):e008408.
doi pubmed pmc - Villablanca PA, Mohananey D, Nikolic K, Bangalore S, Slovut DP, Mathew V, Thourani VH, et al. Comparison of local versus general anesthesia in patients undergoing transcatheter aortic valve replacement: A meta-analysis. Catheter Cardiovasc Interv. 2018;91(2):330-342.
doi pubmed - Hausman MS, Jr., Jewell ES, Engoren M. Regional versus general anesthesia in surgical patients with chronic obstructive pulmonary disease: does avoiding general anesthesia reduce the risk of postoperative complications? Anesth Analg. 2015;120(6):1405-1412.
doi pubmed - Aslan S, Guner A, Demir AR, Yilmaz E, Aslan AF, Celik O, Uzun F, et al. Conscious sedation versus general anesthesia for transcatheter aortic valve implantation in patients with severe chronic obstructive pulmonary disease. Perfusion. 2023;38(1):186-192.
doi pubmed - Debry N, Delhaye C, Azmoun A, Ramadan R, Fradi S, Brenot P, Sudre A, et al. Transcarotid transcatheter aortic valve replacement: general or local anesthesia. JACC Cardiovasc Interv. 2016;9(20):2113-2120.
doi pubmed - Schafer U, Deuschl F, Schofer N, Frerker C, Schmidt T, Kuck KH, Kreidel F, et al. Safety and efficacy of the percutaneous transaxillary access for transcatheter aortic valve implantation using various transcatheter heart valves in 100 consecutive patients. Int J Cardiol. 2017;232:247-254.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cardiology Research is published by Elmer Press Inc.


