| Cardiology Research, ISSN 1923-2829 print, 1923-2837 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, Cardiol Res and Elmer Press Inc |
| Journal website https://www.cardiologyres.org |
Original Article
Volume 14, Number 3, June 2023, pages 201-210
Differentiating Characteristics and Responses to Treatment of New-Onset Heart Failure With Preserved and Reduced Ejection Fraction in Ambulatory Patients
Osama Alhadramya, c , Refal A. Alahmadia
, Afrah M. Alameena
, Nada S. Ashmawia
, Nadeen A. Alrehailia
, Rahaf A. Afandia
, Tahani A. Alrehailia
, Saba Kassimb
aDepartment of Medicine, College of Medicine, Taibah University, Almadinah Almonawarah, Saudi Arabia
bDepartment of Preventive Dental Sciences, College of Dentistry, Taibah University, Almadinah Almonawarah, Saudi Arabia
cCorresponding Author: Osama Alhadramy, Department of Medicine, College of Medicine, Taibah University, Almadinah Almonawarah, Saudi Arabia
Manuscript submitted February 19, 2023, accepted May 6, 2023, published online May 26, 2023
Short title: New-Onset HFpEF vs. HFrEF
doi: https://doi.org/10.14740/cr1483
| Abstract | ▴Top |
Background: Differences in clinical presentation and therapy outcomes between heart failure with preserved ejection fraction (HFpEF) and heart failure with reduced ejection fraction (HFrEF) have been reported but described mainly among hospitalized patients. Because the population of outpatients with heart failure (HF) is increasing, we sought to discriminate the clinical presentation and responses to medical therapy in ambulatory patients with new-onset HFpEF vs. HFrEF.
Methods: We retrospectively included all patients with new-onset HF treated at a single HF clinic in the past 4 years. Clinical data and electrocardiography (ECG) and echocardiography findings were recorded. Patients were followed up once weekly, and treatment response was evaluated according to symptoms resolution within 30 days. Univariate and multivariate regression analyses were performed.
Results: A total of 146 patients were diagnosed with new-onset HF: 68 with HFpEF and 78 with HFrEF. The patients with HFrEF were older than those with HFpEF (66.9 vs. 62 years, respectively, P = 0.008). Patients with HFrEF were more likely to have coronary artery disease, atrial fibrillation, or valvular heart disease than those with HFpEF (P < 0.05 for all). Patients with HFrEF rather than HFpEF were more likely to present with New York Heart Association class 3 - 4 dyspnea, orthopnea, paroxysmal nocturnal dyspnea or low cardiac output (P < 0.007 for all). Patients with HFpEF were more likely than those with HFpEF to have normal ECG at presentation (P < 0.001), and left bundle branch block (LBBB) was observed only in patients with HFrEF (P < 0.001). Resolution of symptoms within 30 days occurred in 75% of patients with HFpEF and 40% of patients with HFrEF (P < 0.001).
Conclusions: Ambulatory patients with new-onset HFrEF were older, and had higher incidence of structural heart disease, in comparison to those with new-onset HFpEF. Patients presenting with HFrEF had more severe functional symptoms than those with HFpEF. Patients with HFpEF were more likely than those with HFpEF to have normal ECG at the time of presentation, and LBBB was strongly associated with HFrEF. Outpatients with HFrEF rather than HFpEF were less likely to respond to treatment.
Keywords: Heart failure; Ejection fraction; Epidemiology; Ambulatory care
| Introduction | ▴Top |
Heart failure (HF) is a complex syndrome manifesting as congestive symptoms (dyspnea, orthopnea, paroxysmal nocturnal dyspnea (PND) and lower limb edema), in the presence or absence of low cardiac output (COP) features, such as weakness and fatigue [ 1]. Worldwide, HF remains a major cause of hospitalization and contributes to substantial health care expenses [ 2].
On the basis of the systolic function of the left ventricle (LV), as measured by the ejection fraction (EF), HF is classified into three major subtypes; HF with reduced EF of ≤ 40% (HFrEF), HF with mid-range EF of 41-49% (HFmrEF) and HF with preserved EF of ≥ 50% (HFpEF) [ 3].
The overall prevalence of HF has been estimated to be < 1% in the population < 40 years of age and > 20% in the population > 80 years of age [ 4].
HFrEF is associated with a marked decrease in LV contractility and end-systolic elastance, with or without LV dilatation [ 5]. The pathophysiology of HFpEF is more complex than that of HFrEF and is driven primarily by impaired LV relaxation and compliance, which may be triggered by systemic conditions such as hypertension (HTN) and obesity [ 6].
Epidemiological data suggest that 40-55% of patients presenting with new-onset decompensated HF have HFpEF rather than HFrEF [ 7, 8]. Several prior studies have described the manifestations and risk factors for new-onset HFpEF and HFrEF, which include older age, HTN, and coronary artery disease (CAD) [ 9]. However, very few studies have examined the discriminating features that may have heterogeneous associations across both subtypes of HF. Patients with HFpEF have different characteristics, non-cardiac comorbidities and HF etiologies from those with HFrEF. However, most prior studies were conducted among hospitalized patients and those with chronic HF [ 10, 11]. HFpEF is more common than HFrEF in older people, women and obese people [ 10, 11]. Despite these differences, the clinical features of hospitalized patients with HFpEF and HFrEF are similar [ 10, 11]. The severity of symptoms, response to therapy, and length of hospital stay have been found to be comparable between HF subtypes [ 12]. However, these findings cannot be generalized to the outpatient HF population, because patients requiring hospitalization for HF have worsening symptoms and tend to have more comorbidities than ambulatory patients. Identifying discriminators between HFpEF and HFrEF in outpatient settings may facilitate early diagnosis. In addition, exploring the therapy response of each subtype may aid in designing efficient outpatient programs for each subtype. Accordingly, the objective of our study was to differentiate the demographic data, clinical presentations, etiologies, and responses to medical therapy between new-onset HFpEF and HFrEF in ambulatory patients.
| Materials and Methods | ▴Top |
Study design, sampling, and setting
We retrospectively reviewed the medical records of all consecutive patients presenting to a single HF clinic between January 2017 and September 2021. All patients 18 years of age or older who were referred to the clinic with new-onset HF, according to symptoms and physical examination, were included in this study. All patients underwent full echocardiographic evaluation by an experienced cardiologist and were accordingly diagnosed with HFpEF (EF of ≥ 50%) or HFrEF (EF of ≤ 40%). We excluded all patients with chronic or asymptomatic HF. Patients with HFmrEF (EF 41-49%) were not included in this cohort.
Data collection and variables
A structured electronic form consisting of eight main sections was used to extract data from the patients’ medical records. The first section collected data on patients’ baseline characteristics, and detailed cardiac and non-cardiac comorbidities. The second section collected data on the clinical presentation, including dyspnea (according to the New York Heart Association (NYHA) classification, grouped into two categories: NYHA class 1 - 2 and NYHA class 3 - 4), orthopnea, PND, angina, lower limb edema and low COP symptoms. The third section involved collecting detailed echocardiographic assessments of LV size, function (diastolic and systolic), regional wall motions and valvular structures. The fourth section collected detailed electrocardiography (ECG) findings, which were categorized into normal ECG, ischemic ECG (ST-segment deviation, pathological Q-wave and ischemic T-wave changes), left ventricular hypertrophy (LVH), left bundle branch block (LBBB), right bundle branch block (RBBB) and atrial fibrillation (AF). In the fifth section, the etiology of HF was recorded on the basis of thorough assessment by a cardiologist, and was categorized into undiagnosed HTN, uncontrolled HTN, CAD, dilated cardiomyopathy (DCM) or valvular heart disease (VHD). Guideline-directed medical therapy (GDMT) was then started according to the type of HF and was titrated according to the clinical status of each patient. Patients were followed up once weekly, and the response to medical therapy was assessed according to the resolution of HF symptoms within 30 days. Figure 1 represents the flow diagram of the patients and the study protocol.
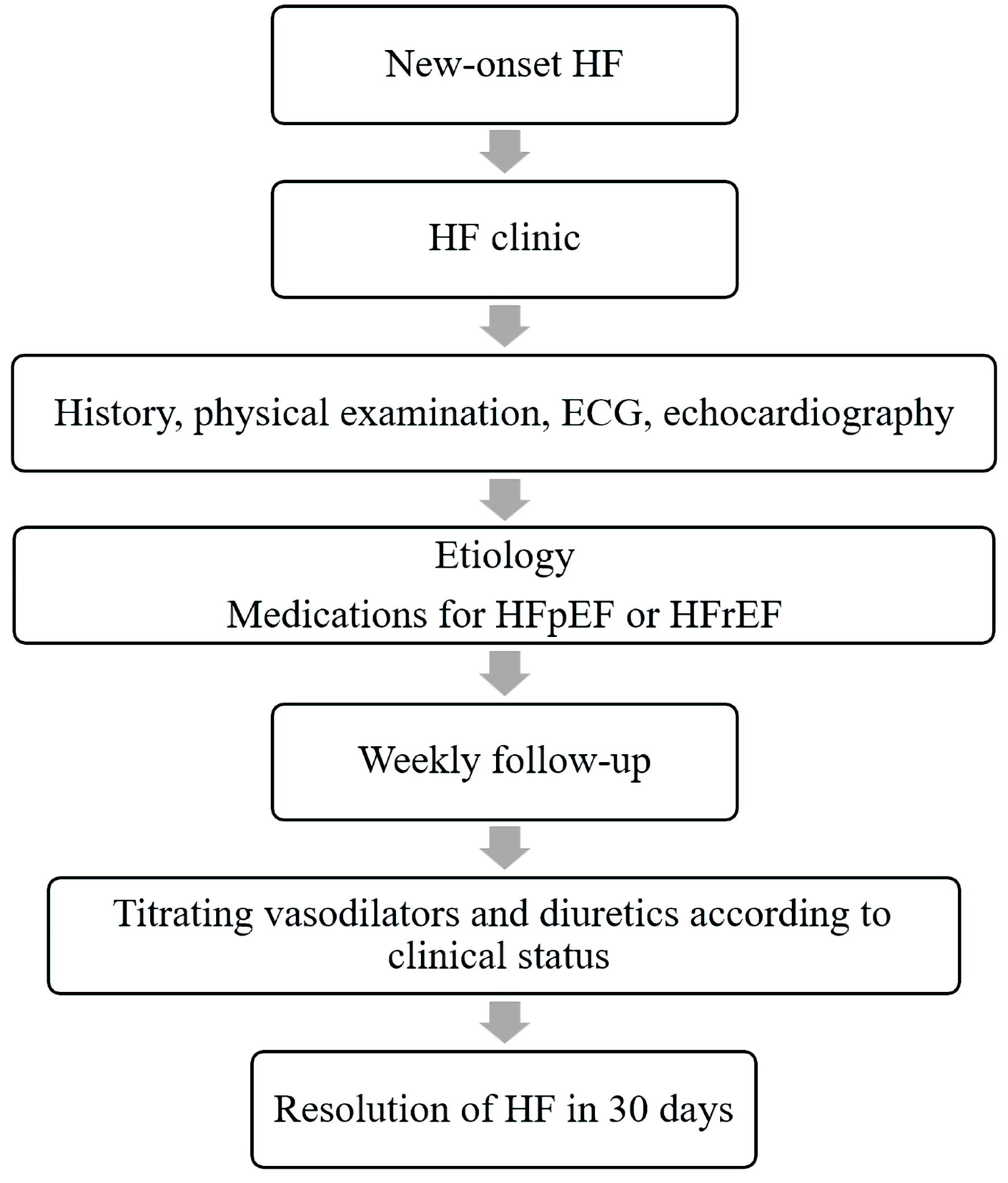 Click for large image | Figure 1. The flow diagram of the patients. All patients with new-onset heart failure (HF) were included in the study. The clinical characteristics and findings of electrocardiography (ECG) and echocardiography were recorded. Patients were diagnosed with HF preserved ejection fraction (HFpEF) or HF with reduced EF (HFrEF) and started medical therapy. They were followed up once weekly, and medications were titrated according to clinical status. The response to medical therapy was evaluated on the basis of resolution of HF in 30 days. |
Data analysis
Excel spreadsheets were downloaded and imported into Statistical Package for Social Sciences (SPSS software for Windows, version 22, IBM) for data analysis. Descriptive analysis was performed to report the sample characteristics. Categorical data are presented as numbers and percentages, and data for continuous variables are presented as mean ± standard deviation (SD) when the quantitative data were found to be normally distributed according to the Shapiro-Wilk test (P > 0.05). Otherwise, data are reported as median and interquartile range (IQR). The t-test and the Mann-Whitney U test were performed to compare the mean ± SD and medians (IQR) of continuous variables for both the HFpEF and HFrEF groups. The Chi-square test and Fisher’s exact test were performed as appropriate to identify any statistically significant associations between dependent variables (HFpEF and HFrEF) and relevant categorical variables. Variables significantly associated (P < 0.05) with each subtype in the univariate analysis were then input into a multivariable logistic regression analysis (adjusted for age and sex), to identify the potential significant (P < 0.05) variables associated with HFpEF or HfrEF.
No prior sample size was calculated for this retrospective study; however, post hoc sample calculation revealed sufficient power for performing logistic regression modellings and was presented in results’ section under relevant tables.
Ethical consideration
The project adhered to the guidelines of the Declaration of Helsinki. The investigators ensured the integrity, privacy, and confidentiality of the patients’ data.
The study received the ethical approval from the Institutional Review Board of our institute (study ID: TU-21-019, dated March 4, 2022).
| Results | ▴Top |
Sample characteristics
A total of 146 consecutive patients with new-onset HF were identified, 68 (46.6%) with HFpEF and 78 (53.4%) with HFrEF. The patients with HFrEF were significantly older than those with HFpEF (mean ± SD age = 66.99 ± 11.19 vs. 62.12 ± 11.55 years, respectively, P = 0.008). The sex distribution between both subtypes was comparable (65% women for HFpEF vs. 62% women for HFrEF, P = 0.693), as was that of tobacco use (7% for HFpEF vs. 3% for HFpEF, P = 0.251). Table 1 summarizes the echocardiographic findings for the cohort.
 Click to view | Table 1. Echocardiographic Findings of the Cohort (N = 146) |
Analyses of comorbidities associated with HFpEF and HFrEF
As shown in Table 2, the univariate analysis indicated that patients with HFrEF, in comparison to those with HFpEF, had higher incidence of CAD (39.7% vs. 22.1%, P = 0.022), chronic kidney disease (CKD) (14.1% vs. 1.5%, P = 0.006), AF (20.5% vs. 8.8%, P = 0.049) or VHD (25.6% vs. 7.4%, P = 0.003), respectively. The body mass index was higher in patients with HFpEF rather than HFrEF (32 vs. 30.23, respectively, P = 0.022). Other comorbidities were comparable between groups (P > 0.05, Table 2). The adjusted model of multivariable logistic regression analysis revealed that patients with HFrEF were older than those with HFpEF (odds ratio (OR) = 1.8, P = 0.008), and have higher incidence of CAD (OR = 3.52, P = 0.005), VHD (OR = 6.93, P = 0.002) or AF (OR = 2.48, P = 0.013) than those with HFpEF.
 Click to view | Table 2. Univariate and Multivariate Adjusted Logistic Regression Analyses of Comorbidities in Patients With HFpEF and HFrEF |
Analyses of symptoms associated with HFpEF and HFrEF
The univariate analysis in Table 3 indicated that patients with HFpEF, compared with those with HFrEF, were more likely to present with NYHA class 1 - 2 dyspnea (86.8% vs. 51.3%, P < 0.001, respectively). In contrast, patients with HFrEF were more likely than those with HFpEF to present with NYHA class 3 - 4 dyspnea (33.3% vs. 5.9%, P < 0.001), orthopnea (41.0% vs. 11.8%, P < 0.001), PND (33.3% vs. 5.9%, P < 0.001) and low COP (14.1% vs. 1.5%, P = 0.006). However, the adjusted multivariable logistic regression model did not indicate significant differences in symptoms between HFpEF and HFrEF.
 Click to view | Table 3. Univariate and multivariate adjusted logistic regression analyses of clinical presentation in patients with HFpEF and HFrEF |
Analyses of ECG findings associated with HFpEF and HFrEF
The univariate analysis findings in Table 4 indicated that patients with HFpEF rather than HFrEF were more likely to have normal ECG at the time of presentation (69.1% vs. 9%, respectively, P < 0.001). AF was more common in patients with HFrEF than HFpEF (20.5% vs. 5.9%, respectively, P = 0.01). LBBB was present only in patients with HFrEF (19.2%, P < 0.001). The adjusted model of multivariable logistic regression analysis demonstrated that the presence of normal ECG correlated well with HFpEF, and LBBB was present only in those with HFrEF (P < 0.001 for both). The prevalence of LVH, ischemic ECG findings, and RBBB were comparable between subtypes.
 Click to view | Table 4. Univariate and Multivariate Adjusted Logistic Regression Analyses of ECG Findings in Patients With HFpEF and HFrEF |
Analyses of the etiology of HFpEF and HFrEF
Table 5 summarizes the etiology of HF in the cohort. Uncontrolled HTN was observed in approximately 52.9% of patients with HFpEF and 9% of patients with HFrEF (P < 0.001). Undiagnosed HTN was identified in 22.1% of patients with HFpEF and 2.6% of patients with HFrEF (P < 0.001). VHD and CAD were the main etiologies for HFrEF, as compared with HFpEF (23.1% vs. 5.9%; P = 0.004 and 30.8% vs. 1.5%, P < 0.001, respectively). DCM was diagnosed in 16.7% patients in the cohort, all of whom were identified to have HFrEF. The adjusted multivariable logistic regression model analysis findings were consistent with those from the univariate analysis with regards to the etiologies of HF.
 Click to view | Table 5. Univariate and Multivariate Adjusted Logistic Regression Analyses of the Etiology of HFpEF and HFrEF, as Well as the Diagnostic Methods |
Response of HFpEF and HFrEF to medical therapy
A total of 23 patients (15.7%) were lost to follow-up over 30 days (10 with HFpEF and 13 with HFrEF). The difference in attrition between groups was nonsignificant (14.7% vs. 16.7%, P = 0.746). Among the remining 123 patients, complete resolution of symptoms occurred in 76% of patients with HFpEF and only 40% of patients with HFrEF (P < 0.001) (Fig. 2). Table 6 summarizes the medications used for both subtypes.
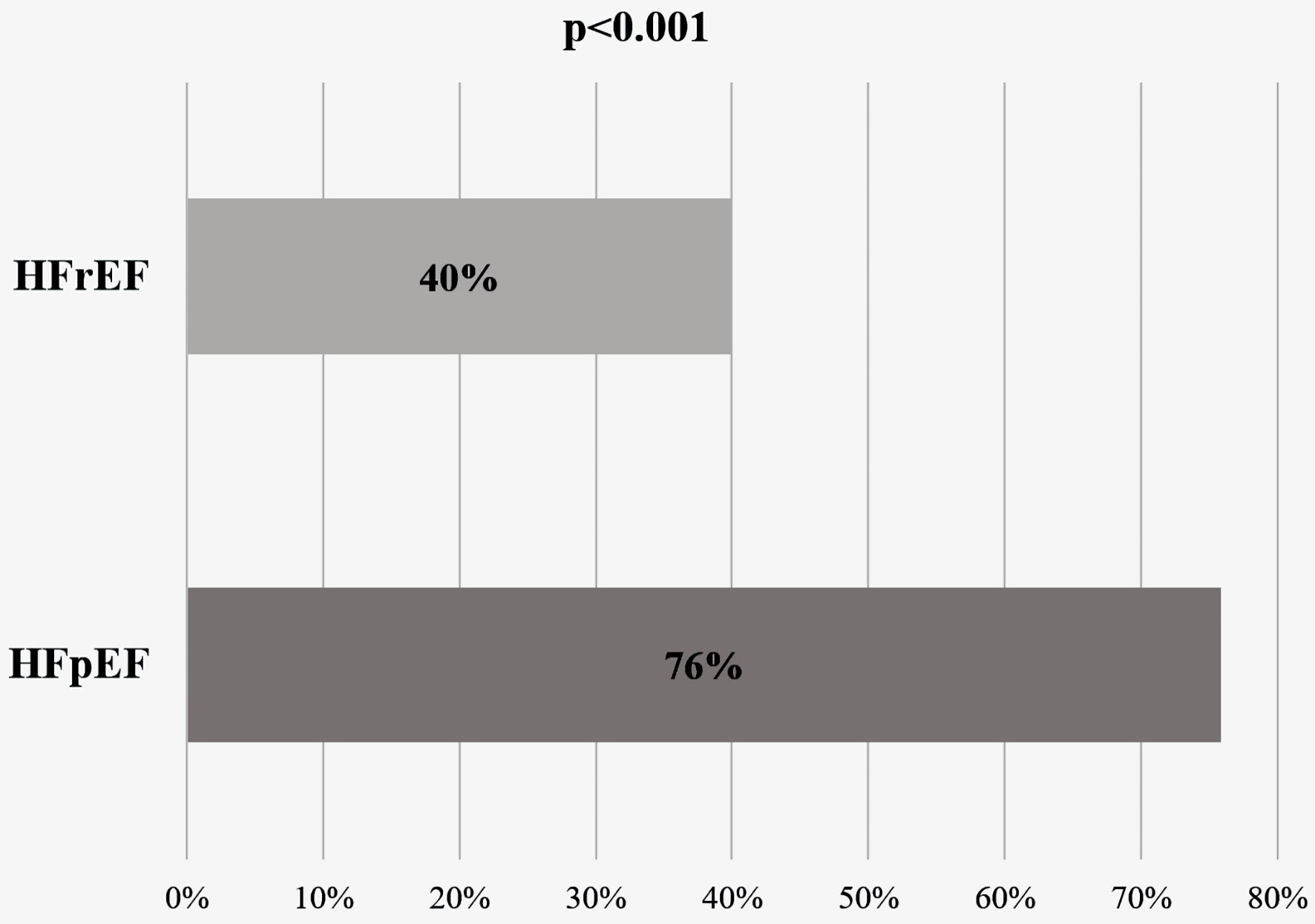 Click for large image | Figure 2. t-test comparison of the rate of resolution of heart failure (HF) in 30 days according to EF (n = 123 patients). HFpEF: heart failure with preserved ejection fraction; HFrEF: heart failure with reduced ejection fraction. |
 Click to view | Table 6. Comparison of Medications Used for Patients With Heart Failure With Preserved Ejection Fraction (HFpEF) and Heart Failure With Reduced Ejection Fraction (HFrEF) |
| Discussion | ▴Top |
Our study demonstrated that, among ambulatory patients with new-onset HF, the demographic data, clinical presentation, and ECG findings at the time of presentation differed between HFpEF and HFrEF. To our knowledge, the current study reports the first evidence of variations in response to medical therapy between subtypes of HF in the outpatient setting.
The incidence of HFpEF in our cohort was 53.4%, as compared with 46.6% for HFrEF, in agreement with the literature [ 13]. The mean age (± SD) for patients with HFpEF and HFrEF was 62.12 ± 11.5 and 66.9 ± 11.1 years, respectively, in agreement with findings from studies exploring the incidence of HF subtypes in our region [ 14]. However, our patients were 10 years younger than those with HFpEF and HFrEF in developed countries. In a large systematic review including 109,275 ambulatory and hospitalized patients with HF, the mean age for patients with HFpEF and HFrEF was 77.6 and 72.3 years, respectively [ 15].
Patients with HFrEF in our cohort were significantly older than those with HFpEF. This finding is not consistent with those of several studies conducted in developed countries, which have reported that patients with HFpEF were older than those with HFrEF [ 16]. Patients with HF in our region are substantially different from those in developed countries [ 17], because of their exceptionally high incidence of DM, CAD, obesity and HTN [ 18].
The sex distribution between subtypes of HF in the current study was comparable, in accordance with findings from a study examining the incidence of HFpEF and HFrEF among Medicare beneficiaries [ 19]. In our region, one study has examined the differences in demographic data between both HF subtypes and has not observed a significant difference in sex distribution [ 20]. However, other studies from developed countries have demonstrated that women are at greater risk of developing HFpEF than men, with an estimated ratio of 2:1 [ 21].
Analysis of the comorbidities associated with HFpEF and HFrEF indicated that patients with HFpEF were more obese than those with HFrEF. This finding was in accordance with those from most related studies [ 22]. Compared with non-obese patients, obese patients tend to have more sodium retention, high levels of neurohormones and a systemic inflammatory response, which compromises LV compliance [ 23].
We found that CAD and VHD were more common in patients with HFrEF in comparison to those with HFpEF. This finding has also been verified by previous studies [ 24, 25]. Chronic or acute ischemia directly damages myocytes, thus leading to LV remodeling, scar formation and a decline in LV systolic function [ 26]. Severe mitral regurgitation, the most common VHD among our cohort with HFrEF, has been strongly associated with HFrEF [ 27].
We demonstrated that AF was more common in patients with HFrEF in comparison to those with HFpEF. This finding is probably attributable to the high prevalence of structural heart disease in patients with HFrEF. The estimated prevalence of AF in patients with CAD, VHD and DCM is 53%, 25% and 40%, respectively [ 28]. HF registries in the Middle East have reported less AF than international registries [ 17, 18], probably because of the relatively younger population of patients with HF in our region. The present study indicated that CKD tended to be more common in patients with HFrEF in comparison to those with HFpEF, in accordance with findings from a meta-analysis examining the distribution of CKD across HF subtypes [ 15].
In the present study, we showed that patients with HFrEF presented with more severe functional symptoms, i.e., NYHA class 3 - 4 dyspnea, orthopnea, PND and low COP symptoms, than patients with HFpEF. This finding is probably attributable to the higher prevalence of structural heart disease in patients with HFrEF rather than HFpEF. Few studies have explored differences in clinical presentation across HF subtypes. In a community-based study, patients with HFrEF have been found to be more likely to present with NYHA class 3 - 4 dyspnea than patients with HFpEF [ 29]. The OPTIMIZE-HF registry has also indicated that patients with NYHA class 4 dyspnea are more likely to have EF < 40% than EF > 50% [ 30]. In another study examining the incidence and outcomes of HFpEF and HFrEF in the SPRINT trial, patients with HFrEF had more NYHA class 4 dyspnea and orthopnea than patients with HFpEF [ 31]. In the KorAHF registry, NYHA class 3 - 4 was experienced by 86.9% of patients with HFrEF [ 32]. Finally, in a Canadian study including more than 2,000 hospitalized patients with HF, 30.1% of patients with a diagnosis of HFrEF had PND, compared with 24% of patients with HFpEF (P = 0.007) [ 33].
Symptoms of low COP occur in < 10% of patients with acute HF [ 34] and consequently have been underinvestigated in the literature. The decrease in COP is directly proportional to the magnitude of the functional impairment [ 35- 37]. In our study, these symptoms were encountered by 14% of patients with HFrEF, compared with 1.5% of patients with HFpEF (P = 0.006). This finding is consistent with those from a study in which patients with HFrEF walked significantly shorter distances than those with HFpEF in 6-min walking tests [ 35]. Patients with HFrEF in our cohort had more structural heart disease and more severe functional class than those with HFpEF. These results have been shown to correlate well with a decline in upper and lower extremity exercises [ 36]. Our study indicated that patients with mild dyspnea (NYHA 1 or 2) were more likely to have HFpEF than HFrEF (86.8% and 51.3%, respectively; P < 0.001), probably because most of the former patients were younger and were less likely to have significant structural heart disease. These findings are consistent with previously reported observations [ 29].
Analysis of the ECG findings in this cohort indicated that the presence of LBBB at the time of presentation was strongly associated with HFrEF. This result is similar to the findings of studies exploring ECG differences between HFpEF and HFrEF [ 8].
More than 60% of patients with HFpEF in the present cohort did not have any significant ECG changes. To our knowledge, our study is the first to demonstrate this correlation. This finding may be explained by the younger age and the lower prevalence of structural heart disease in patients with HFpEF rather than HFrEF. This correlation is consistent with literature reports [ 38, 39]. The prevalence of LVH in our patients was comparable between HFpEF and HFrEF, in agreement with previously reported findings [ 40].
Analysis of the etiology of HF indicated that the leading cause of HFrEF was CAD (30%), and the leading cause of HFpEF was uncontrolled HTN (52.9%). CAD has been established to be responsible for approximately 35-55% of all HFrEF hospital visits [ 41]. In contrast, HTN is the leading cause of HFpEF, with an estimated prevalence of 45-80% [ 42]. Interestingly, undiagnosed HTN was identified in 24.7% of the patients in our cohort, 92% of whom had HFpEF. HTN is a potential risk factor for all types of HF [ 1, 2]; however, its existence as a solitary etiology for HFrEF is uncommon [ 43]. Although cardiovascular features in HFpEF have been described in people with asymptomatic HTN [ 44], to our knowledge, our study is the first to estimate its prevalence across both subtypes.
Resolution of HF symptoms among patients who were successfully followed up once weekly for 30 days was more common in HFpEF than HFrEF (76% and 40%, respectively; P < 0.001). Despite close follow-up and titration of GDMT once weekly, patients with HFrEF responded more poorly to therapy than patients with HFpEF. To our knowledge, no studies have examined this response in ambulatory patients, but hospitalized patients with HFrEF have been reported to have longer hospital stays than patients with HFpEF [ 45]. We attribute our findings to the milder symptoms (NYHA of class 1 - 2), younger age and less structural heart disease in patients with HFpEF rather than HFrEF. Exploring the appropriate follow-up interval to improve the rate of the resolution of symptoms among patients with HFrEF was beyond the scope of our study.
Limitations
The results of our study should be carefully interpreted in the context of various limitations. Because this retrospective study included a small sample size from a single HF clinic, the findings may not represent the full spectrum of ambulatory HF patients. In addition, the findings should not be generalized to asymptomatic, hospitalized patients or those with chronic HF, who were excluded from the study. The diagnosis and evaluation of HF were established mainly on the basis of clinical assessment, and few patients had supporting evidence such as elevated brain natriuretic peptide levels. The resolution of HF in 30 days was determined on the basis of clinical evaluation, which is subjected to significant inter-observer variability. The patients with HFpEF in our cohort were younger than those with HFrEF, thus potentially influencing the ECG findings and clinical characteristics. Finally, the discriminators identified in the current study should not replace echocardiography in establishing the diagnosis of HFpEF and HFrEF.
Conclusions
In summary, many clinical characteristics and ECG findings differed in ambulatory patients with new-onset HFpEF versus HFrEF. Patients with HFrEF were more likely to have cardiac comorbidities and to present with more severe functional status in than patients with HFpEF. These discriminators may facilitate earlier diagnosis and referral to HF clinics. Outpatients with new-onset HFrEF were less likely to respond to treatment than those with HFpEF.
Acknowledgments
None to declare.
Financial Disclosure
This research did not receive any funding.
Conflict of Interest
The authors have no conflict of interest to declare.
Informed Consent
Not applicable.
Author Contributions
OA: conception and design of the project, recruitment of patients, supervision, literature review and writing of the final manuscript; RA Alahmadi, AMA, NSA, NAA, RA Afandi and TAA: data collection, processing, analysis of data, literature review and writing of the first draft of the manuscript; SK: design and execution of statistical analysis, supervision of data entry, and writing the first draft of the methods and results sections of the manuscript.
Data Availability
The data supporting the findings of this study are available from the corresponding author upon reasonable request.
Abbreviations
HF: heart failure; PND: paroxysmal nocturnal dyspnea; COP: cardiac output; LV: left ventricle; HFpEF: heart failure with preserved ejection fraction; HFmrEF: heart failure with mid-range ejection fraction; HFrEF: heart failure with reduced ejection fraction; HTN: hypertension; CAD: coronary artery disease; NYHA: New York Heart Association; ECG: electrocardiography; LVH: left ventricular hypertrophy; LBBB: left bundle branch block; RBBB: right bundle branch block; DCM: dilated cardiomyopathy; VHD: valvular heart disease; GDMT: guideline-directed medical therapy; SPSS: Statistical Package for the Social Sciences; IBM: International Business Machines; SD: standard deviation; IQR: interquartile range; CKD: chronic kidney disease; DM: diabetes mellitus
| References | ▴Top |
- Hayes SM, Peloquin S, Howlett JG, Harkness K, Giannetti N, Rancourt C, Ricard N. A qualitative study of the current state of heart failure community care in Canada: what can we learn for the future? BMC Health Serv Res. 2015;15:290.
doi pubmed pmc - Benjamin EJ, Muntner P, Alonso A, Bittencourt MS, Callaway CW, Carson AP, Chamberlain AM, et al. Heart disease and stroke statistics-2019 update: a report from the American Heart Association. Circulation. 2019;139(10):e56-e528.
doi pubmed - Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE, Jr., Drazner MH, Fonarow GC, et al. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2013;62(16):e147-239.
doi pubmed - Mosterd A, Hoes AW. Clinical epidemiology of heart failure. Heart. 2007;93(9):1137-1146.
doi pubmed pmc - Komajda M, Lam CS. Heart failure with preserved ejection fraction: a clinical dilemma. Eur Heart J. 2014;35(16):1022-1032.
doi pubmed - Rose-Jones LJ, Rommel JJ, Chang PP. Heart failure with preserved ejection fraction: an ongoing enigma. Cardiol Clin. 2014;32(1):151-161.
doi pubmed - Owan TE, Hodge DO, Herges RM, Jacobsen SJ, Roger VL, Redfield MM. Trends in prevalence and outcome of heart failure with preserved ejection fraction. N Engl J Med. 2006;355(3):251-259.
doi pubmed - Ho JE, Lyass A, Lee DS, Vasan RS, Kannel WB, Larson MG, Levy D. Predictors of new-onset heart failure: differences in preserved versus reduced ejection fraction. Circ Heart Fail. 2013;6(2):279-286.
doi pubmed pmc - Lee GK, Lee LC, Liu CW, Lim SL, Shi LM, Ong HY, Lim YT, et al. Framingham risk score inadequately predicts cardiac risk in young patients presenting with a first myocardial infarction. Ann Acad Med Singap. 2010;39(3):163-167.
pubmed - Smith GL, Masoudi FA, Vaccarino V, Radford MJ, Krumholz HM. Outcomes in heart failure patients with preserved ejection fraction: mortality, readmission, and functional decline. J Am Coll Cardiol. 2003;41(9):1510-1518.
doi pubmed - Jaarsma T, Halfens R, Abu-Saad HH, Dracup K, Stappers J, van Ree J. Quality of life in older patients with systolic and diastolic heart failure. Eur J Heart Fail. 1999;1(2):151-160.
doi pubmed - Tsutsui H, Tsuchihashi M, Takeshita A. Mortality and readmission of hospitalized patients with congestive heart failure and preserved versus depressed systolic function. Am J Cardiol. 2001;88(5):530-533.
doi pubmed - Carlsen CM, Bay M, Kirk V, Gotze JP, Kober L, Nielsen OW. Prevalence and prognosis of heart failure with preserved ejection fraction and elevated N-terminal pro brain natriuretic peptide: a 10-year analysis from the Copenhagen Hospital Heart Failure Study. Eur J Heart Fail. 2012;14(3):240-247.
doi pubmed - Abohammar S, ElSaidy MA, Fathalla D, Aldosarri M. Baseline characteristics of patients with heart failure and preserved ejection fraction at admission with acute heart failure in Saudi Arabia. Egypt Heart J. 2017;69(1):21-28.
doi pubmed pmc - Lauritsen J, Gustafsson F, Abdulla J. Characteristics and long-term prognosis of patients with heart failure and mid-range ejection fraction compared with reduced and preserved ejection fraction: a systematic review and meta-analysis. ESC Heart Fail. 2018;5(4):685-694.
doi pubmed pmc - Borlaug BA, Paulus WJ. Heart failure with preserved ejection fraction: pathophysiology, diagnosis, and treatment. Eur Heart J. 2011;32(6):670-679.
doi pubmed pmc - Elasfar AA, Alhabeeb W, Elasfar S. Heart failure in the Middle East Arab countries: current and future perspectives. J Saudi Heart Assoc. 2020;32(2):236-241.
doi pubmed pmc - AlHabib KF, Elasfar AA, AlBackr H, AlFaleh H, Hersi A, AlShaer F, Kashour T, et al. Design and preliminary results of the heart function assessment registry trial in Saudi Arabia (HEARTS) in patients with acute and chronic heart failure. Eur J Heart Fail. 2011;13(11):1178-1184.
doi pubmed - Lee MP, Glynn RJ, Schneeweiss S, Lin KJ, Patorno E, Barberio J, Levin R, et al. Risk factors for heart failure with preserved or reduced ejection fraction among medicare beneficiaries: application of competing risks analysis and gradient boosted model. Clin Epidemiol. 2020;12:607-616.
doi pubmed pmc - Al Shamiri MQ, Alharbi W, Alanazi NA, Alsaleh AM. Mobarak M, Alsaluli. Prevalence and baseline characteristics of patients with heart failure and preserved ejection fraction at outpatients sitting in Saudi Arabia. Cardiology Research and Reports. 2022;4(4).
doi - Packer M, Kitzman DW. Obesity-related heart failure with a preserved ejection fraction: the mechanistic rationale for combining inhibitors of aldosterone, neprilysin, and sodium-glucose cotransporter-2. JACC Heart Fail. 2018;6(8):633-639.
doi pubmed - Koutroumpakis E, Kaur R, Taegtmeyer H, Deswal A. Obesity and Heart Failure with Preserved Ejection Fraction. Heart Fail Clin. 2021;17(3):345-356.
doi pubmed - Masoudi FA, Havranek EP, Smith G, Fish RH, Steiner JF, Ordin DL, Krumholz HM. Gender, age, and heart failure with preserved left ventricular systolic function. J Am Coll Cardiol. 2003;41(2):217-223.
doi pubmed - Philbin EF, Rocco TA, Jr., Lindenmuth NW, Ulrich K, Jenkins PL. Systolic versus diastolic heart failure in community practice: clinical features, outcomes, and the use of angiotensin-converting enzyme inhibitors. Am J Med. 2000;109(8):605-613.
doi pubmed - Purek L, Laule-Kilian K, Christ A, Klima T, Pfisterer ME, Perruchoud AP, Mueller C. Coronary artery disease and outcome in acute congestive heart failure. Heart. 2006;92(5):598-602.
doi pubmed pmc - Chioncel O, Lainscak M, Seferovic PM, Anker SD, Crespo-Leiro MG, Harjola VP, Parissis J, et al. Epidemiology and one-year outcomes in patients with chronic heart failure and preserved, mid-range and reduced ejection fraction: an analysis of the ESC Heart Failure Long-Term Registry. Eur J Heart Fail. 2017;19(12):1574-1585.
doi pubmed - Buckley BJR, Harrison SL, Gupta D, Fazio-Eynullayeva E, Underhill P, Lip GYH. Atrial Fibrillation in Patients With Cardiomyopathy: Prevalence and Clinical Outcomes From Real-World Data. J Am Heart Assoc. 2021;10(23):e021970.
doi pubmed pmc - Iorio A, Senni M, Barbati G, Greene SJ, Poli S, Zambon E, Di Nora C, et al. Prevalence and prognostic impact of non-cardiac co-morbidities in heart failure outpatients with preserved and reduced ejection fraction: a community-based study. Eur J Heart Fail. 2018;20(9):1257-1266.
doi pubmed - Fonarow GC, Stough WG, Abraham WT, Albert NM, Gheorghiade M, Greenberg BH, O'Connor CM, et al. Characteristics, treatments, and outcomes of patients with preserved systolic function hospitalized for heart failure: a report from the OPTIMIZE-HF Registry. J Am Coll Cardiol. 2007;50(8):768-777.
doi pubmed - Upadhya B, Willard JJ, Lovato LC, Rocco MV, Lewis CE, Oparil S, Cushman WC, et al. Incidence and outcomes of acute heart failure with preserved versus reduced ejection fraction in SPRINT. Circ Heart Fail. 2021;14(12):e008322.
doi pubmed pmc - Cho JH, Choe WS, Cho HJ, Lee HY, Jang J, Lee SE, Choi JO, et al. Comparison of characteristics and 3-year outcomes in patients with acute heart failure with preserved, mid-range, and reduced ejection fraction. Circ J. 2019;83(2):347-356.
doi pubmed - Bhatia RS, Tu JV, Lee DS, Austin PC, Fang J, Haouzi A, Gong Y, et al. Outcome of heart failure with preserved ejection fraction in a population-based study. N Engl J Med. 2006;355(3):260-269.
doi pubmed - Abraham WT, Adams KF, Fonarow GC, Costanzo MR, Berkowitz RL, LeJemtel TH, Cheng ML, et al. In-hospital mortality in patients with acute decompensated heart failure requiring intravenous vasoactive medications: an analysis from the Acute Decompensated Heart Failure National Registry (ADHERE). J Am Coll Cardiol. 2005;46(1):57-64.
doi pubmed - Weber KT, Kinasewitz GT, Janicki JS, Fishman AP. Oxygen utilization and ventilation during exercise in patients with chronic cardiac failure. Circulation. 1982;65(6):1213-1223.
doi pubmed - Batalli A, Ibrahimi P, Bytyci I, Ahmeti A, Haliti E, Elezi S, Henein MY, et al. Different determinants of exercise capacity in HFpEF compared to HFrEF. Cardiovasc Ultrasound. 2017;15(1):12.
doi pubmed pmc - Jondeau G, Katz SD, Zohman L, Goldberger M, McCarthy M, Bourdarias JP, LeJemtel TH. Active skeletal muscle mass and cardiopulmonary reserve. Failure to attain peak aerobic capacity during maximal bicycle exercise in patients with severe congestive heart failure. Circulation. 1992;86(5):1351-1356.
doi pubmed - Ather S, Chan W, Bozkurt B, Aguilar D, Ramasubbu K, Zachariah AA, Wehrens XH, et al. Impact of noncardiac comorbidities on morbidity and mortality in a predominantly male population with heart failure and preserved versus reduced ejection fraction. J Am Coll Cardiol. 2012;59(11):998-1005.
doi pubmed pmc - Campbell RT, Jhund PS, Castagno D, Hawkins NM, Petrie MC, McMurray JJ. What have we learned about patients with heart failure and preserved ejection fraction from DIG-PEF, CHARM-preserved, and I-PRESERVE? J Am Coll Cardiol. 2012;60(23):2349-2356.
doi pubmed - Tribouilloy C, Rusinaru D, Mahjoub H, Souliere V, Levy F, Peltier M, Slama M, et al. Prognosis of heart failure with preserved ejection fraction: a 5 year prospective population-based study. Eur Heart J. 2008;29(3):339-347.
doi pubmed - McDermott MM, Feinglass J, Sy J, Gheorghiade M. Hospitalized congestive heart failure patients with preserved versus abnormal left ventricular systolic function: clinical characteristics and drug therapy. Am J Med. 1995;99(6):629-635.
doi pubmed - Pfeffer MA, Shah AM, Borlaug BA. Heart failure with preserved ejection fraction in perspective. Circ Res. 2019;124(11):1598-1617.
doi pubmed pmc - Felker GM, Thompson RE, Hare JM, Hruban RH, Clemetson DE, Howard DL, Baughman KL, et al. Underlying causes and long-term survival in patients with initially unexplained cardiomyopathy. N Engl J Med. 2000;342(15):1077-1084.
doi pubmed - Melenovsky V, Borlaug BA, Rosen B, Hay I, Ferruci L, Morell CH, Lakatta EG, et al. Cardiovascular features of heart failure with preserved ejection fraction versus nonfailing hypertensive left ventricular hypertrophy in the urban Baltimore community: the role of atrial remodeling/dysfunction. J Am Coll Cardiol. 2007;49(2):198-207.
doi pubmed - Joyce E, Chung C, Badloe S, Odutayo K, Desai A, Givertz MM, Nohria A, et al. Variable contribution of heart failure to quality of life in ambulatory heart failure with reduced, better, or preserved ejection fraction. JACC Heart Fail. 2016;4(3):184-193.
doi pubmed - Olchanski N, Vest AR, Cohen JT, Neumann PJ, DeNofrio D. Cost comparison across heart failure patients with reduced and preserved ejection fractions: Analyses of inpatient decompensated heart failure admissions. Int J Cardiol. 2018;261:103-108.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cardiology Research is published by Elmer Press Inc.


