| Cardiology Research, ISSN 1923-2829 print, 1923-2837 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, Cardiol Res and Elmer Press Inc |
| Journal website https://www.cardiologyres.org |
Original Article
Volume 14, Number 2, April 2023, pages 142-148
Left Atrial Remodeling in Patients With Severe Rheumatic Mitral Stenosis and Sinus Rhythm Using Two-Dimensional and Three-Dimensional Speckle Tracking Echocardiography
Taher Said Abd Elkareema, c, Taghreed Abdelrahman Ahmedb, Layla Ahmed Mohamedb
aIslamic Center of Cardiology, Al Azhar University, Cairo, Egypt
bCardiology Department, Faculty of Medicine for Girls, Al-Azhar University, Cairo, Egypt
cCorresponding Author: Taher Said Abd-Elkareem, Islamic Center of Cardiology, Al-Azhar University, Cairo, Egypt
Manuscript submitted January 4, 2023, accepted February 20, 2023, published online March 25, 2023
Short title: Left Atrial Remodeling in RHD MS Patient
doi: https://doi.org/10.14740/cr1465
| Abstract | ▴Top |
Background: In mitral stenosis (MS), the combination of an increase in left atrium (LA) pressure and atrial inflammatory response is accompanied by increase in interstitial fibrosis of the atrial wall with disorganization of atrial muscle bundles, LA dysfunction and subsequently LA dilatation. We aimed to assess the effect of severe rheumatic MS on LA volumes and mechanics.
Methods: We enrolled 40 patients with pure severe rheumatic MS and sinus rhythm as a patient group and 30 healthy subjects as a control group. All patient and control groups underwent two-dimensional (2D) transthoracic echo to measure left ventricle (LV) dimensions, function, LA deformations, estimated systolic pulmonary artery pressure (EPAP), and left ventricle global longitudinal strain (LV GLS). Also LA volumes and mechanics (LA strain during LV systole (reservoir function) and LV diastole (early = conduit, and late = booster pump = atrial contraction)) were measured by three-dimensional (3D) transthoracic echo; mitral valve (MV) area was measured by 3D transesophageal echo (as routine pre-percutaneous MV commissurotomy using multiplanar reconstruction in mid-esophageal apical long-axis view from LA prospective).
Results: By 2D transthoracic echo, patient group revealed significantly lower all LA function vs. control group including LA strain during reservoir (24 ± 6 vs. 43 ± 3, P < 0.001), LA strain during conduit (-11 ± 3 vs. -25 ± 2, P < 0.001), and during booster pump (-13 ± 4 vs. -18 ± 1, P < 0.001). EPAP was significantly higher in patient group (48 ± 7 vs. 27 ± 4 in control group). LV GLS was significantly lower in patient group (-16±2% vs. -23±2% in control group). All 3D LA volumes were significantly higher in patient group than control group including maximum LA volume (LAVmax) (76 ± 18 vs. 50 ± 5, P < 0.001), indexed LA volume (LAVi) (44.6 ± 10.1 vs. 28.7 ± 3.7, P < 0.001), LV minimum volume (LAVmin) (51 ± 15 vs. 30 ± 4, P < 0.001), and LA volume pre atrial contraction (LAVpre A) (63 ± 15 vs. 41 ± 6, P < 0.001). Also, there was significantly decreased LA strain using 3D speckle tracking echo in patient group including systolic deformation of LA (reservoir function) (23 ± 6 vs. 41 ± 3, P < 0.001) and diastolic deformation, early diastole (conduit function) (-10 ± 2 vs. -24 ± 2, P < 0.001), and late diastole (booster pump function) (-13 ± 4 vs. -18 ± 1, P < 0.001).
Conclusions: All LA function markedly reduced in pure severe rheumatic MS. The reduction of LA mechanics is directly related to the degree of reduction of the stenotic MV area. LV GLS significantly reduced in severe MS and its reduction is directly related to the degree of reduction of the stenotic MV area and the LAVi by 3D echo.
Keywords: Left atrial strain; 2D and 3D speckle tracking echocardiography; Mitral stenosis
| Introduction | ▴Top |
Left atrium (LA) has three components of function: 1) During left ventricle (LV) systole, the LA acts as a reservoir, allowing the blood to be collected proximal to the closed mitral valve; 2) During early LV diastole, the LA has conduit function and results in its shortening; 3) During late diastole, the LA acts as a booster pump [1]. Given its important role, changes in LA size or function have been associated with adverse cardiovascular outcomes. For example, enlargement of the LA is associated with a higher incidence of atrial fibrillation (AF) and stroke [2]. Rheumatic heart disease (RHD) is a major health problem in developing countries and leads to significant comorbidities. In mitral stenosis (MS), the combination of an increase in LA pressure and an intense atrial inflammatory response secondary to the underlying rheumatic carditis is accompanied by a progressive increase in interstitial fibrosis of the atrial wall with disorganization of atrial muscle bundles, LA dysfunction, and subsequently LA dilatation [3]. Three-dimensional (3D) echocardiography is more accurate than conventional two-dimensional (2D) echocardiography in the assessment of LA volumes, as 3D echocardiography avoids errors in measuring left atrial volumes by 2D echo such as geometrical assumptions of left atrial shape and foreshortening in the 2D views [4]. In our study, we aimed to assess the effect of severe rheumatic MS on LA volumes (using 3D echo) and LA mechanics (using 2D and 3D echo).
| Materials and Methods | ▴Top |
Study design and populations
This study included 40 patients (patient group) and 30 healthy subjects (control group): all control group had no chronic illness and their age was less than 40; all patients had severe rheumatic MS referred to do pre-percutaneous mitral valvuloplasty echo-Doppler assessment. They were examined in a single center (Islamic Center of Cardiology, Al-Azhar University, Egypt). This study was ethically approved by Al-Azhar University's Research Ethics Committee (2022071413, 09/08/2022). Written informed consents from all the participants were obtained. The study protocol conformed to the Helsinki Declaration, the ethical norm of the World Medical Association for human testing.
From 117 examined patients favorable for percutaneous balloon dilatation, we included in this study only 40 patients; those were symptomatic (New York Heart Association (NYHA) classification III), severe MS (mitral valve area (MVA) less than 1.5 cm2) and had sinus rhythm.
We excluded patients with: 1) poor echo window; 2) significant aortic valve disease (more than mild aortic stenosis (AS) or aortic regurgitation (AR)); 3) more than mild mitral regurgitation (MR); 4) LA or left atrial appendage (LAA) thrombus; 5) echocardiographic evidence of other cardiac diseases such as ischemic, pericardial, or congenital heart disease; 6) AF or other arrhythmia; and 7) organic tricuspid valve disease.
All patient and control groups were subjected to the following measures: full history taking to assess severity of symptoms and medication used, full clinical examination, resting 12-lead electrocardiogram (ECG).
Transthoracic echo-Doppler scan
The examination was done using a 2.5 multi-frequency 1.7 - 4 MHz transducer (GE Vivid 95 ultrasound machine) and the off-line analysis of the 2D and 3D speckle tracking echocardiography (STE) was done using GE Echo pack 204 software. The following data were obtained: 1) Using 2D-guided M-mode to assess LV end-systolic and end-diastolic dimensions (mm2), LV ejection fraction (EF) (%), fractional shortening (%), interventricular septum end-diastolic diameter (mm), LV posterior wall end-diastolic diameter (mm) and left atrial dimension (mm); 2) Using 2D echo for the measurement of MVA by planimetry in short-axis view at the level of mitral valve and measurement of LVEF by biplane method from apical four-chamber and apical two-chamber views; 3) Using conventional pulsed wave Doppler to assess mitral E and A wave velocities (cm/s), E/A ratio; 4) Using conventional continuous wave Doppler to assess presence or absence of MR and its degree, and by Bernoulli equation from tricuspid regurgitation (TR) velocity to measure estimated systolic pulmonary artery pressure (EPAP) (mm Hg); 5) Using tissue Doppler imaging to assess S wave velocity, Ea wave velocity, Aa wave velocity and E/Ea ratio.
2D speckle tracking
For the assessment of LV longitudinal strain, three LV apical views, apical four-chamber, two-chamber, and long-axis views were acquired at high frame rates (range: 59 - 82 frame/s; mean: 72 ± 6 frame/s). In each plane, three consecutive cardiac cycles were acquired during a breath hold and digitally stored in a hard disk for off-line analysis. In order to measure the timing of cardiac events, LV inflow and outflow velocities were recorded using pulsed-wave Doppler echocardiography.
Also, we used 2D speckle tracking for the assessment of LA strain. Apical four-chamber and two-chamber were acquired at high frame rates (range: 59 - 82 frame/s; mean: 72 ± 6 frame/s), and from it we calculated biplane LA strain in reservoir, conduit, and contraction stages.
3D transthoracic echocardiography (TTE)
Using 3D TTE, apical four-chamber view was acquired at high frame rates (range: more than 25 frame/s, using multi-beat modality to increase frame rate while the patient catches his breath at the end of expiration) and digitally stored in a hard disk for off-line analysis. We measured LV volumes (maximum, indexed, minimum and pre A LA volumes), LAEF and LA strain in reservoir, conduit and contraction function.
We measured MVA by 3D transesophageal echocardiography (TEE) (as routine pre-percutaneous mitral valve commissurotomy using multiplanar reconstruction in mid-esophageal apical long-axis view from LA prospective to measure MVA (Fig. 1) in the study group data).
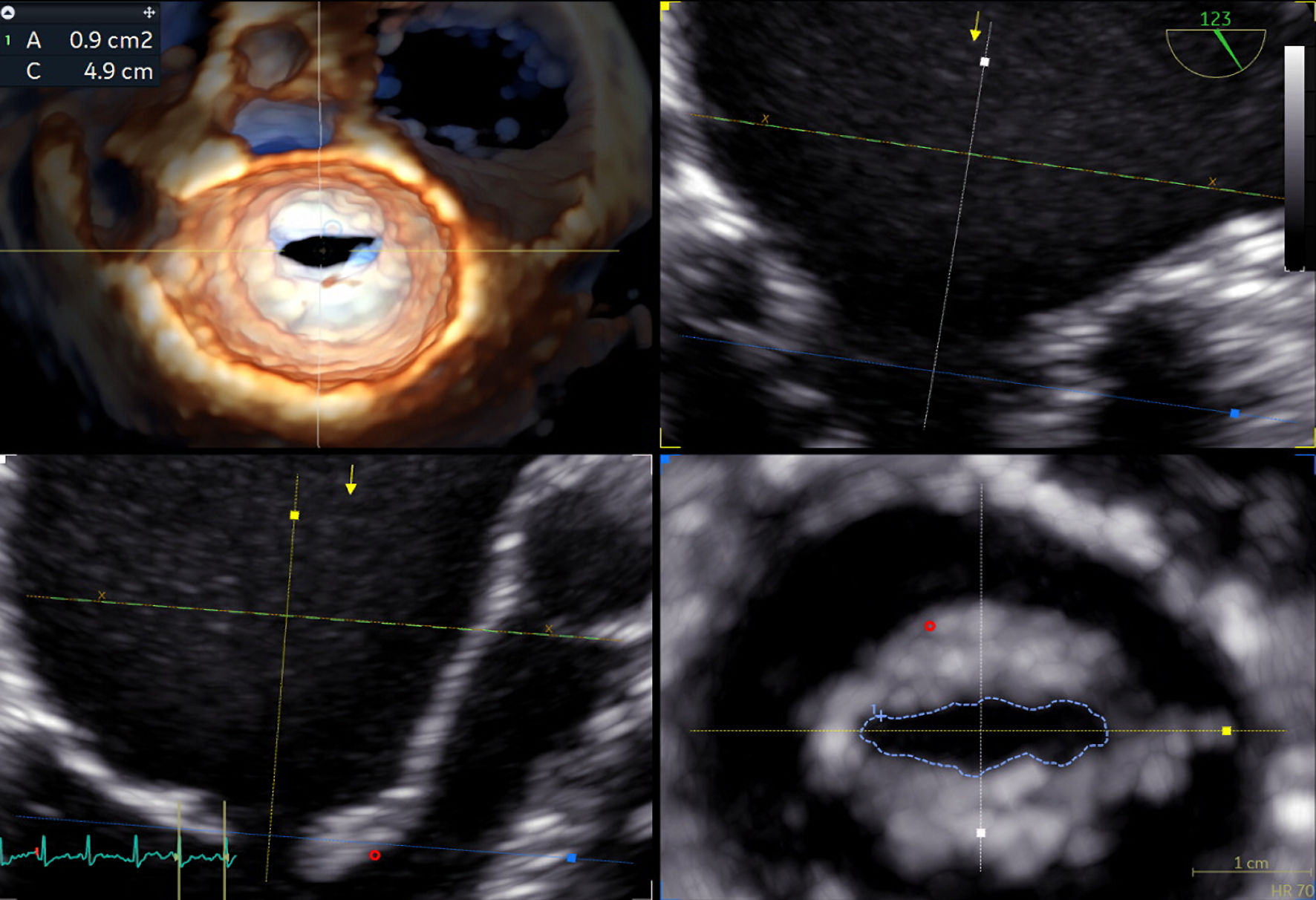 Click for large image | Figure 1. Measurement of MVA using multiplanar reconstruction by 3D TEE. MVA: mitral valve area; 3D: three-dimensional; TEE: transesophageal echocardiography. |
Statistical methods
Data management and statistical analysis were done using SPSS version 28 (IBM, Armonk, New York, United States). Quantitative data were assessed for normality using the Shapiro-Wilk test and direct data visualization methods. Quantitative data were summarized as means and standard deviations. Categorical data were summarized as numbers and percentages. Quantitative data were compared between the studied groups using independent t-test. Categorical data were compared using the Chi-square test. Agreement between 2D and 3D parameters was assessed using intraclass correlation coefficient (ICC). Correlation analyses were done using Pearson’s correlation. All statistical tests were two-sided. P values less than 0.05 were considered significant.
| Results | ▴Top |
General characteristics
The age was significantly higher in the patient group (35 ± 7 years) than in the control group (28 ± 5) (P < 0.001), because we enrolled in control group young healthy individuals free of any risk factors that may affect LA mechanics. No significant differences were observed regarding sex (P = 0.369), body mass index (BMI) (P = 0.379), and body surface area (BSA) (P = 0.130) as shown in Table 1.
 Click to view | Table 1. General Characteristics of the Studied Groups |
LA volumes and EF by 3D echocardiography
The patient group showed significantly higher LA maximum volume (V max) (76 ± 18 vs. 50 ± 5, P < 0.001), indexed LA volume (LAVi) (44.6 ± 10.1 vs. 28.7 ± 3.7, P < 0.001), LA minimum volume (V min) (51 ± 15 vs. 30 ± 4, P < 0.001), LA pre atrial contraction volume (V pre A) (63 ± 15 vs. 41 ± 6, P < 0.001) than control group and revealed significantly lower total LAEF (38 ± 7 vs. 45 ± 4, P < 0.001) as shown in Figure 2 and Table 2.
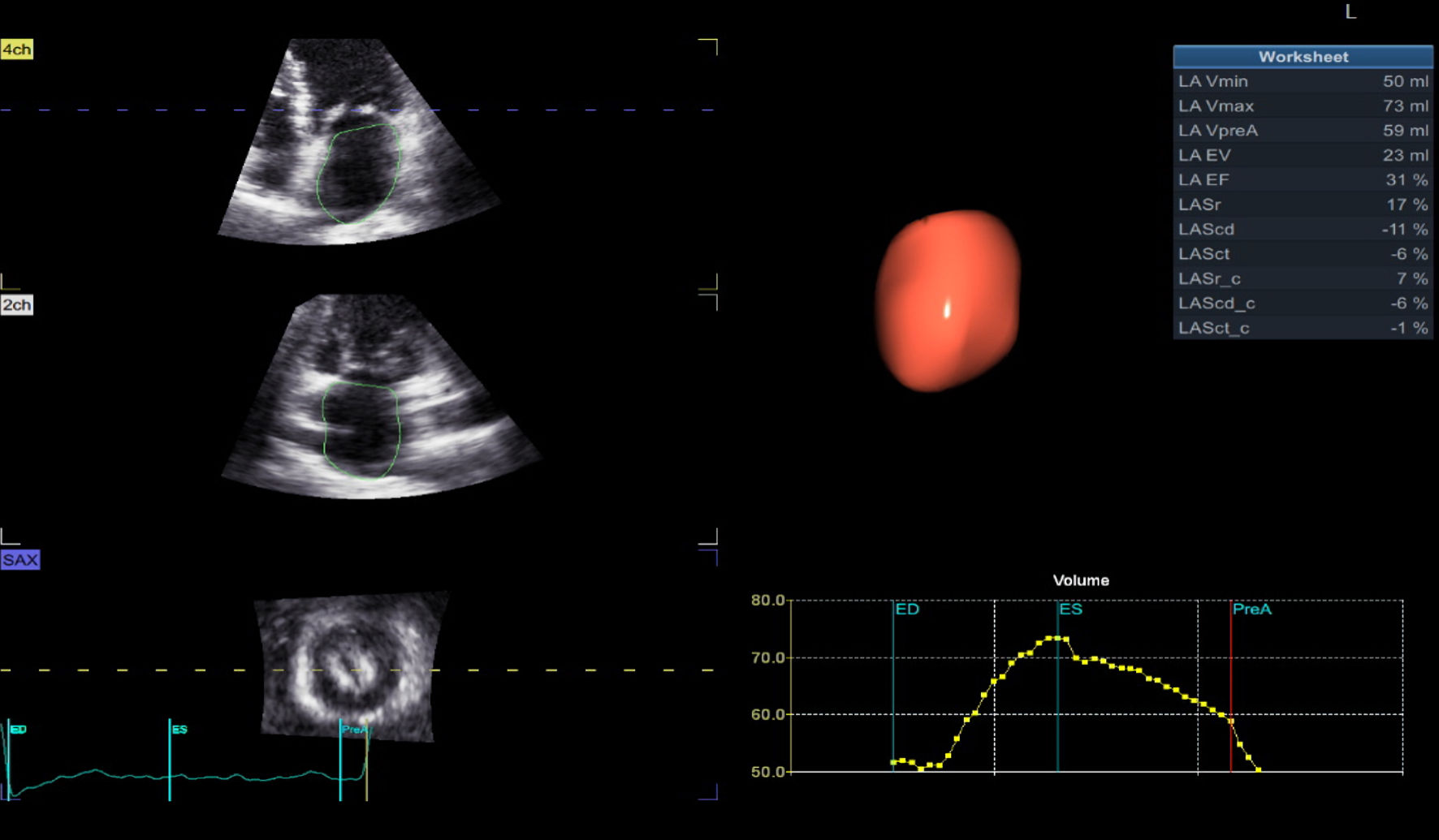 Click for large image | Figure 2. Increased LA volumes and decreased LA mechanics and EF% using 3D echo. LA: left atrium; 3D: three-dimensional; EF: ejection fraction. |
 Click to view | Table 2. 2D and 3D Left Atrial Parameters in the Patient Group |
Regarding LA mechanics using 3D STE and 2D STE
Using 3D STE, there were significantly decreased systolic deformation of LA (reservoir function) LAS-r (23 ± 6 vs. 41 ± 3, P < 0.001) and diastolic deformation (early diastole; conduit function) LAS-cd (-10 ± 2 vs. -24 ± 2, P < 0.001), and (late diastole; booster pump function) LAS-ct (-13 ± 4 vs. -18 ± 1, P < 0.001) in patient group vs. control group as shown in Table 2.
Also using 2D speckle tracking imaging, the patient group revealed significantly lower peak left atrial strain during reservoir (pLASr) (24 ± 6 vs. 43 ± 3, P < 0.001), peak left atrial strain during conduit (pLAS-cd) (-11 ± 3 vs. -25 ± 2, P < 0.001), and pLAS-ct (-13 ± 4 vs. -18 ± 1, P < 0.001) than control group as shown in Table 2. Also using 2D STE, the left ventricle global longitudinal strain (LV GLS) was significantly reduced in patient group (-16±2% vs. -23±2% in control group) instead of apparently normal EF in both groups shown in Table 2.
EPAP
There was significant elevation of EPAP in patient group (48 ± 7 vs. 27 ± 4 in control group) as also shown in Table 2.
Agreement between 2D STE and 3D STE
There were good agreements between 2D and 3D LAS-r (ICC = 0.835, 95% confidence interval (CI) = 0.7 - 0.911) and LASR-ct (ICC = 0.862, 95% CI = 0.752 - 0.925), while a moderate agreement was reported regarding LASR-cd (ICC = 0.688, 95% CI = 0.477 - 0.823) as shown in Table 3.
 Click to view | Table 3. Agreement Between 2D and 3D Strain in the Studied Patients |
Correlation between 3D MVA and other 3D echo parameters
Significant positive correlations were reported between 3D MVA and 3D LAS-r (r = 0.475, P = 0.002), 3D LAS-cd (r = 0.495, P = 0.001), and 3D LAS-ct (r = 0.395, P = 0.012). In contrast, 3D MVA was significantly negatively correlated with 3D LAVi (r = -0.354, P = 0.025) as shown in Table 4.
 Click to view | Table 4. Correlation Between 3D MVA and Other 3D Echo Parameters |
Correlation between 2D MVA and other 2D echo parameters
2D MVA revealed significantly positive correlation with 2D peak LA strain in reservoir (pLASR-r) (r = 0.425, P value = 0.006) and 2D peak LA strain at conduit (pLASR-cd) (r = 0.490, P value = 0.001), while it did not show significant correlation with 2D peak LA strain during contraction (pLASR-ct) (P value = 0.009) as shown in Table 5.
 Click to view | Table 5. Correlation Between 2D MVA and Other 2D Parameters in the Patient Group |
Correlation between EPAP and other 3D echo parameters
EPAP showed significant negative correlations with 3D MVA (r = -0.849, P < 0.001) and 3D LAS-cd (r = -0.374, P = 0.017). In contrast, it did not reveal any significant correlation with 3D LAVi (P = 0.084), 3D LAS-r (P = 0.065), and 3D LAS-ct (P = 0.184) as shown in Figure 3.
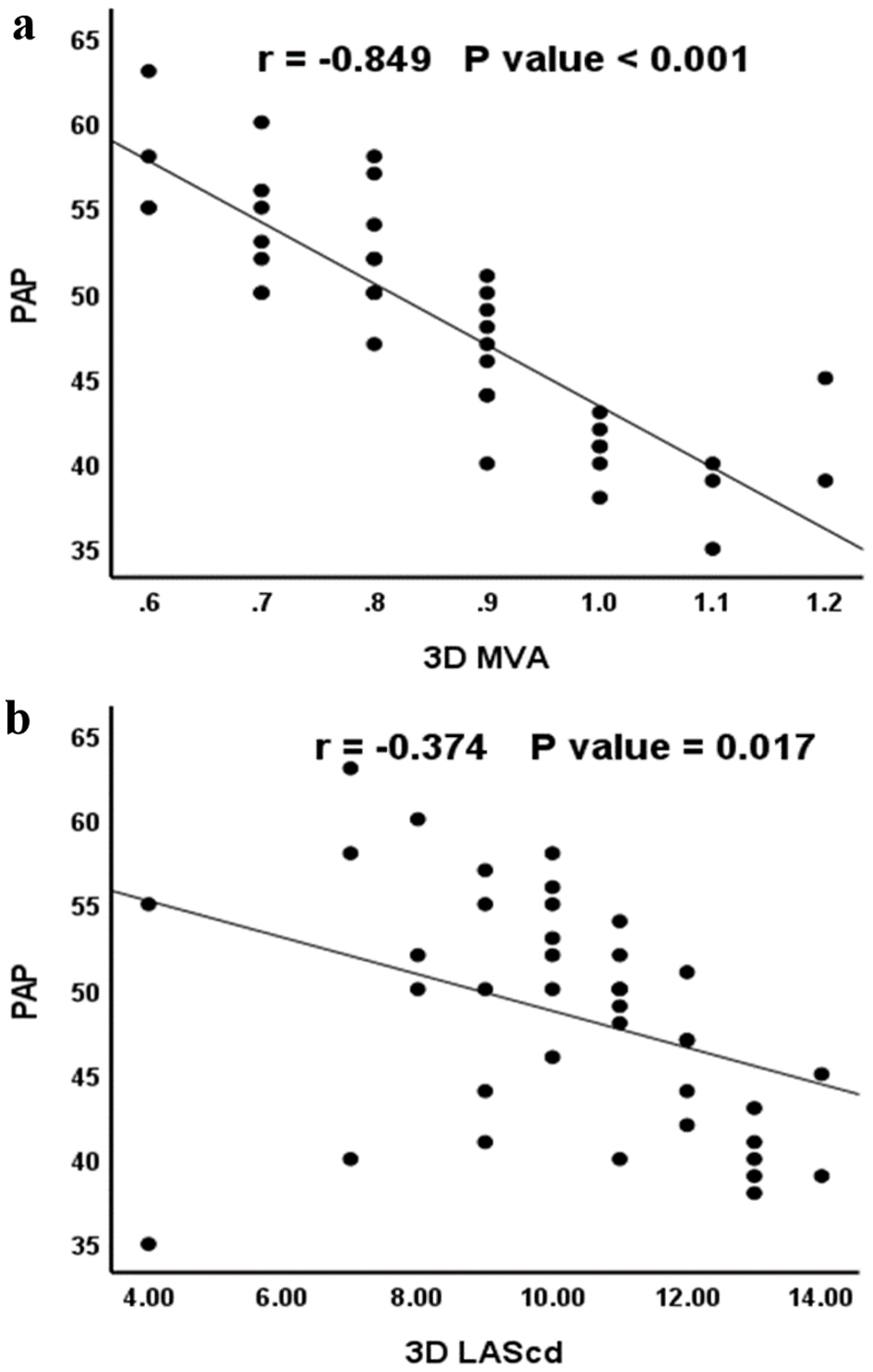 Click for large image | Figure 3. Correlation between EPAP and (a) 3D MVA, (b) 3D LAS-cd. EPAP: estimated systolic pulmonary artery pressure; 3D: three-dimensional; PAP: pulmonary artery pressure; MVA: mitral valve area; LAS-cd: left atrial strain during conduit. |
Correlation between LV GLS and 3D MVA and LAVi
LV GLS showed significant positive correlations with 3D MVA (r = 0.433, P = 0.005) and a significant negative correlation with 3D LAVi (r = -0.509, P < 0.001) as shown in Table 6.
 Click to view | Table 6. Correlation Between LV GLS and 3D MVA and LAVi in the Patient Group |
| Discussion | ▴Top |
LA has three components of function: 1) During LV systole, the LA acts as a reservoir, allowing the blood to be collected proximal to the closed mitral valve; 2) During early LV diastole, the LA has conduit function and results in its shortening; 3) During late diastole, the LA acts as a booster pump [1]. Given its important role, changes in LA size or function have been associated with adverse cardiovascular outcomes. For example, enlargement of the LA is associated with a higher incidence of AF and stroke [2].
RHD is a major health problem in developing countries and leads to significant comorbidities. In case of MS, the combination of an increase in LA pressure and an intense atrial inflammatory response secondary to the underlying rheumatic carditis is accompanied by a progressive increase in interstitial fibrosis of the atrial wall with disorganization of atrial muscle bundles, LA dysfunction, and subsequently LA dilatation [3]. 3D echocardiography is more accurate than conventional 2D echocardiography in the assessment of LA volumes, as 3D echocardiography avoids errors in measuring left atrial volumes by 2D echo such as geometrical assumptions of left atrial shape and foreshortening of the 2D views [4].
In our study there were markedly increased all LA volumes in patient group, as the narrowing of the mitral valve orifice restricts the blood flow through the valve and increases the pressure gradient between the LA and the LV. This results in the increase of left atrial pressure and stretch of its myocardium, which leads to LA dilatation and its volumes increasing. Also, in rheumatic MS the inflammatory process of rheumatic carditis leads to replacement of healthy myocardium by fibrous tissue, which is another mechanism of LA dilatation and increases its volumes. These results were concordant with the study by Moise et al, who concluded that in non-significant MS there were increased LA dimensions and volumes in all cases group [5]. In our study the indexed LA volume shows significant increase (44.6 ± 10.1) in patient group, the indexed LA volume had a prognostic value, and is associated with increased mortality as concluded by Yedidya et al [6].
In our study there was a significant negative correlation between MVA (measured by multiplanar reconstruction using 3D TEE) and LAVi. This conclusion was discordant with what was proved by the study of Iqbal et al [7], which showed no significant correlation between MVA and LA size. This may be due to that in his study group 46% of patients had AF that was associated with more myocardial affection, and also he used 2D-guided M-mode modality to measure LA size, but in our study we use 3D volumetric method to measure LA size.
LA deformations either during LV systole (reservoir function) or LV diastole (conduit and contraction functions) by 3D echo were significantly reduced, and this may be due to the presence of forward LA outflow obstruction by stenotic mitral valve orifice, or as a sequel of prior rheumatic carditis. This reduction in LA deformation by 3D STE shows a good agreement when measured by 2D STE, and these results were concordant with the study of Ranien et al [8], which concluded reduction in LA function by 2D STE in rheumatic MS.
In severe MS, the elevated left atrial pressure passively elevates pulmonary venous and pulmonary capillary pressures and causes symptoms of pulmonary congestion reflex pulmonary arteriolar constriction, obliterative changes in pulmonary vascular bed and development of pulmonary artery hypertension (PAH) [9]. Bernoulli equation was used to measure estimated PAP, and this equation showed good correlation with the right heart catheterization measurements in assessment of pulmonary artery pressure in MS as concluded by Sohrabi et al [10]. We found significantly elevated EPAP in patient group, and as our patients had severe MS, elevated LA pressure and decreased LA compliance.
There were significant negative correlations between elevated EPAP and 3D MVA and also with late diastolic LA deformation (booster pump function) by 3D STE. These results was concordant with the results of Neema et al [11], who found the elevated PAP in MS is directly related to mitral valve orifice, LA compliance, LA pressure and pulmonary venous compliance [11].
LVEF was normal in patient group when measured by both M-mode and by biplane method; however it was significantly higher by M-mode method, in contrast to LV GLS that shows significant reduction in patient group. This is because LVEF only reflects volume changes between the end-diastole and end-systole phase and does not assess the myocardial mechanic. Therefore, LVEF has limitations in assessing cardiac function in abnormal hemodynamic conditions as concluded by Purwowiyoto et al [12]. Also, we found significant positive correlation between LV GLS and 3D MVA and significant negative correlation between LV GLS and LAVi, and these results were concordant with the results of Gerede et al, who concluded meaningful correlation between the change in MVA and LV GLS [13].
Limitation
Sample size of the study group was small, because we excluded a large number of patients who had AF or had significant affection of other cardiac valves.
Conclusions
3D speckle tracking echo is a feasible method for the assessment of LA mechanics in patients with rheumatic MS. All LA function markedly reduced in pure severe rheumatic MS. The reduction of LA mechanics is directly related to the degree of reduction of the stenotic MVA. LV GLS significantly reduced in severe MS and its reduction is directly related to the degree of reduction of the stenotic MVA and the indexed LA volume by 3D echo.
Acknowledgments
None to declare.
Financial Disclosure
None to declare.
Conflict of Interest
The authors declare that they have no conflict of interest.
Informed Consent
Written consent was obtained.
Author Contributions
Taher Said Abd Elkareem (first author) did the transthoracic echo, did the analysis of TTE data in the vendor software, wrote the paper and wrote the revised manuscript. Taghreed Abdelrahman Ahmed (second author) did the TEE to exclude contraindications for BMV, measured MV area by TEE 3D echo, collected the data and inserted it in the Excel sheet, and helped the corresponding author to write the discussion. Layla Ahmed Mohamed (third author) helped the second author in data collection, reviewed the grammar, helped in discussion writing, did the collection of references, and sent the collected data for statistical analysis.
Data Availability
The authors declare that data supporting the findings of this study are available within the article.
Abbreviations
RHD: rheumatic heart disease; LA: left atrium; MS: mitral stenosis; 2D: two-dimensional; 3D: three-dimensional; STE: speckle tracking echocardiography; PAP: pulmonary artery pressure; LV GLS: left ventricle global longitudinal strain; LASr: left atrial strain during reservoir; LAS-cd: left atrial strain during conduit; LAS-ct: left atrial strain during contraction; pLASr: peak left atrial strain during reservoir; pLAS-cd: peak left atrial strain during conduit; pLAS-ct: peak left atrial strain during contraction; ICC: intraclass correlation coefficient; CI: confidence interval
| References | ▴Top |
- Ojaghi Haghighi Z, Naderi N, Amin A, Taghavi S, Sadeghi M, Moladoust H, Maleki M, et al. Quantitative assessment of right atrial function by strain and strain rate imaging in patients with heart failure. Acta Cardiol. 2011;66(6):737-742.
doi pubmed - Bouzas-Mosquera A, Broullon FJ, Alvarez-Garcia N, Mendez E, Peteiro J, Gandara-Sambade T, Prada O, et al. Left atrial size and risk for all-cause mortality and ischemic stroke. CMAJ. 2011;183(10):E657-664.
doi pubmed pmc - Her AY, Choi EY, Shim CY, Song BW, Lee S, Ha JW, Rim SJ, et al. Prediction of left atrial fibrosis with speckle tracking echocardiography in mitral valve disease: a comparative study with histopathology. Korean Circ J. 2012;42(5):311-318.
doi pubmed pmc - Badano LP, Miglioranza MH, Mihaila S, Peluso D, Xhaxho J, Marra MP, Cucchini U, et al. Left atrial volumes and function by three-dimensional echocardiography: reference values, accuracy, reproducibility, and comparison with two-dimensional echocardiographic measurements. Circ Cardiovasc Imaging. 2016;9(7):e004229.
doi pubmed - Moise B, Rosca M, Alexandru D, Ginghina C. Left atrial remodelling in patients with mitral stenosis. Romanian Journal of Cardiology. 2017;27(2).
- Yedidya I, Butcher SC, Stassen J, van der Bijl P, Ngiam JN, Chew NWS, Sia CH, et al. Prognostic value of left atrial volume index in degenerative mitral stenosis. Int J Cardiovasc Imaging. 2022;38(12):2687-2693.
doi pubmed pmc - Iqbal U, Kaleem M, Hanif A, Hanif MI. Correlation of left atrial size with mitral valve area & atrial fibrillation in the patients of mitral stenosis, an echocardiographic based study. J F J M C. 2014;8(1).
- El-shafai RH, El-Masry MM; El-Shedoudy SA, El-Saedy MA. Left atrial function assessment in patients with rheumatic mitral valve diseases. Med J Cairo Univ. 2019;87(1):769-780.
doi - Maeder MT, Weber L, Buser M, Gerhard M, Haager PK, Maisano F, Rickli H. Pulmonary hypertension in aortic and mitral valve disease. Front Cardiovasc Med. 2018;5:40.
doi pubmed pmc - Sohrabi B, Kazemi B, Mehryar A, Teimouri-Dereshki A, Toufan M, Aslanabadi N. Correlation between pulmonary artery pressure measured by echocardiography and right heart catheterization in patients with rheumatic mitral valve stenosis (A Prospective Study). Echocardiography. 2016;33(1):7-13.
doi pubmed - Neema PK, Rathod RC. Pulmonary artery hypertension in mitral stenosis: Role of right ventricular stroke volume, atrio-ventricular compliance, and pulmonary venous compliance. J Anaesthesiol Clin Pharmacol. 2012;28(2):261-262.
doi pubmed pmc - Purwowiyoto SL, Halomoan R. Highlighting the role of global longitudinal strain assessment in valvular heart disease. Egypt Heart J. 2022;74(1):46.
doi pubmed pmc - Gerede DM, Ongun A, Tulunay Kaya C, Acibuca A, Ozyuncu N, Erol C. Use of strain and strain rate echocardiographic imaging to predict the progression of mitral stenosis: a 5-year follow-up study the progression of mitral stenosis: a 5-year follow-up study. Anatol J Cardiol. 2016;16(10):772-777.
doi
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cardiology Research is published by Elmer Press Inc.


