| Cardiology Research, ISSN 1923-2829 print, 1923-2837 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, Cardiol Res and Elmer Press Inc |
| Journal website https://www.cardiologyres.org |
Review
Volume 13, Number 5, October 2022, pages 264-267
Is Long COVID Syndrome a Transient Mitochondriopathy Newly Discovered: Implications of CPET
Stefanos G. Sakellaropoulosa, g, Muhammad Alib, Athanasios Papadisc, Muhemin Mohammedd, Andreas Mitsise, Zaza Zivzivadzef
aDepartment of Internal Medicine, Cardiology, Cantonal Hospital Baden, Baden, Switzerland
bClinic of Cardiology Salzgitter, Salzgitter, Germany
cSwiss Cardiovascular Centre, Bern University Hospital, Bern, Switzerland
dClinic of Internal Medicine, Hospital Affoltern, Affoltern, Switzerland
eCardiology Department, Nicosia General Hospital, Nicosia, Cyprus
fDepartment of Emergency Care, Hospital Affoltern, Affoltern, Switzerland
gCorresponding Author: Stefanos G. Sakellaropoulos, Department of Internal Medicine, Cardiology, Cantonal Hospital Baden, Baden, Switzerland
Manuscript submitted August 13, 2022, accepted September 23, 2022, published online October 25, 2022
Short title: Long COVID Syndrome
doi: https://doi.org/10.14740/cr1419
- Abstract
- Introduction
- Cardiorespiratory Function, Ventilation, Oxygen Delivery and Extraction
- Exercise Oscillatory Ventilation (EOV) Following COVID-19 Disease
- Mitochondrial Dysfunction and Vitamin D Deficiency
- Conclusions
- References
| Abstract | ▴Top |
The new outbreak of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection has an impact worldwide, primarily as a medical emergency. Even that the total constellation is considered as a pandemic of acute respiratory disease, coronavirus disease 2019 (COVID-19) gives rise to dysfunction in multiple organs (e.g., brain, lungs, heart, muscles) that impairs cardiopulmonary (CP) function. Parallel to the CP consequences of COVID-19 is a significant reduction in physical activity. Cardiopulmonary exercise testing (CPET) is daily used in clinical practice to define prognosis, provide risk stratification and treatment strategy. As such, the significance of CPET is crucial concerning clinical assessments of COVID-19 patients. Furthermore, new studies aim at understanding the effects of SARS-CoV-2 infection in long term. Multiple studies have investigated the cardiopulmonary function and impairment of exercise endurance in such patients, as well as a possible prolonged physical impairment. With this review, we summarize the COVID-19-associated pathophysiology for the Long COVID (LC) syndrome as well as the importance of performing CPET.
Keywords: Cardiopulmonary exercise test; Long COVID syndrome; Mitochondriopathy
| Introduction | ▴Top |
Almost 80% of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) cases are with no symptoms or with a mild form of the disease. Most of the patients recover within 2 - 4 weeks [1]. Between 2% and 12% of patients report prolonged symptoms, which reflect the Long COVID (LC) [2]. Prolonged illness, lasting up to 2 years, may lead to exercise intolerance, breathlessness, and palpitations [3]. Functional limitations [4] and anatomical or cellular abnormalities (e.g., fibrosis and myocardial inflammation) have been widely reported [5].
Cardiorespiratory fitness (CRF) may be affected following coronavirus disease 2019 (COVID-19) infection [6], due to the fact that the virus has an impact to the systems responsible for it, for example cardiac, pulmonary, and the skeletal muscle one [7]. Cardiopulmonary exercise testing (CPET) can define the quantification of CRF and provides important information concerning ventilatory inefficiency or other pathomechanisms of exercise limitation [8, 9].
| Cardiorespiratory Function, Ventilation, Oxygen Delivery and Extraction | ▴Top |
Current data indicate that at peak workload the maximal oxygen consumption, tidal volume, as well as peripheral oxygen consumption are found lower in Long COVID-19 patients than healthy individuals. On the other hand, it has been found the respiratory rate was higher. Apart from peak workload, even during submaximal exercise, exercise hyperventilation has been found higher, and as a result, the partial end tidal carbon dioxide has been found lower than healthy individuals [10].
Interestingly, the maximal oxygen consumption at discharge was lower by 30% [11]. The extent of such functional impairment was larger than previous reports, lasted even for 12 months after discharge [12].
Moreover, reduction of oxygen content due to anemia (approximately 8-50% of patients) as well as by impaired peripheral extraction are considered as the main cause of functional limitation. The mechanism of anemia is unknown, most probably in the course of chronic persistent inflammation [13]. This constellation may also reflect the potential direct or indirect myopathic damage rather than isolated muscular disease [14].
| Exercise Oscillatory Ventilation (EOV) Following COVID-19 Disease | ▴Top |
Unfortunately and relatively often, pulmonary function tests fail to reveal the association between the severity of symptomatology and objective findings in patients after COVID-19 infection [11]. And so, CPET has emerged as the best option to quantify the degree of exercise impairment, while also facilitating differential diagnostics [15, 16]. Up to this day, there is no typical finding of “long COVID pattern” [17-19]. Hyperventilation in LC syndrome has been reported in several studies [20-22]. Current data suggest that approximately a third of post-COVID patients had an abnormal breathing pattern (BrP) or the so called EOV. Patients with an abnormal BrP had lower exercise capacity, lower maximal oxygen consumption and lower peak ventilation [23]. Accordingly, these results demonstrate that abnormal exercise ventilation may at least in part explain the symptomatology of the prolonged exercise intolerance.
| Mitochondrial Dysfunction and Vitamin D Deficiency | ▴Top |
Recent studies demonstrate the abnormally low fatty acid oxidation (FATox) and increased lactate production as a cause to the functional impairment. With gradual increase of glycolysis under exercise, lactate is oxidized for energy production in mitochondria, primarily in slow-twitch muscle fibers. Like FATox, lactate clearance capacity is an important marker for mitochondrial function. In post-COVID patients, the muscular metabolic disturbances may be worse than in active individuals or in individuals who suffer from metabolic syndrome [24].
Whereas increase of the lactate levels are usually seen during high exercise intensity, high blood levels at lower exercise intensity point out an underlying mitochondrial dysfunction. Increased arterial lactate levels at relatively low exercise intensity (e.g., .9 mM at 150 W) suggest the premature transition from FATox to carbohydrate oxidation (CHOox), showing metabolic reprogramming and dysfunctional mitochondria in long COVID-19 syndrome [25] (Fig. 1).
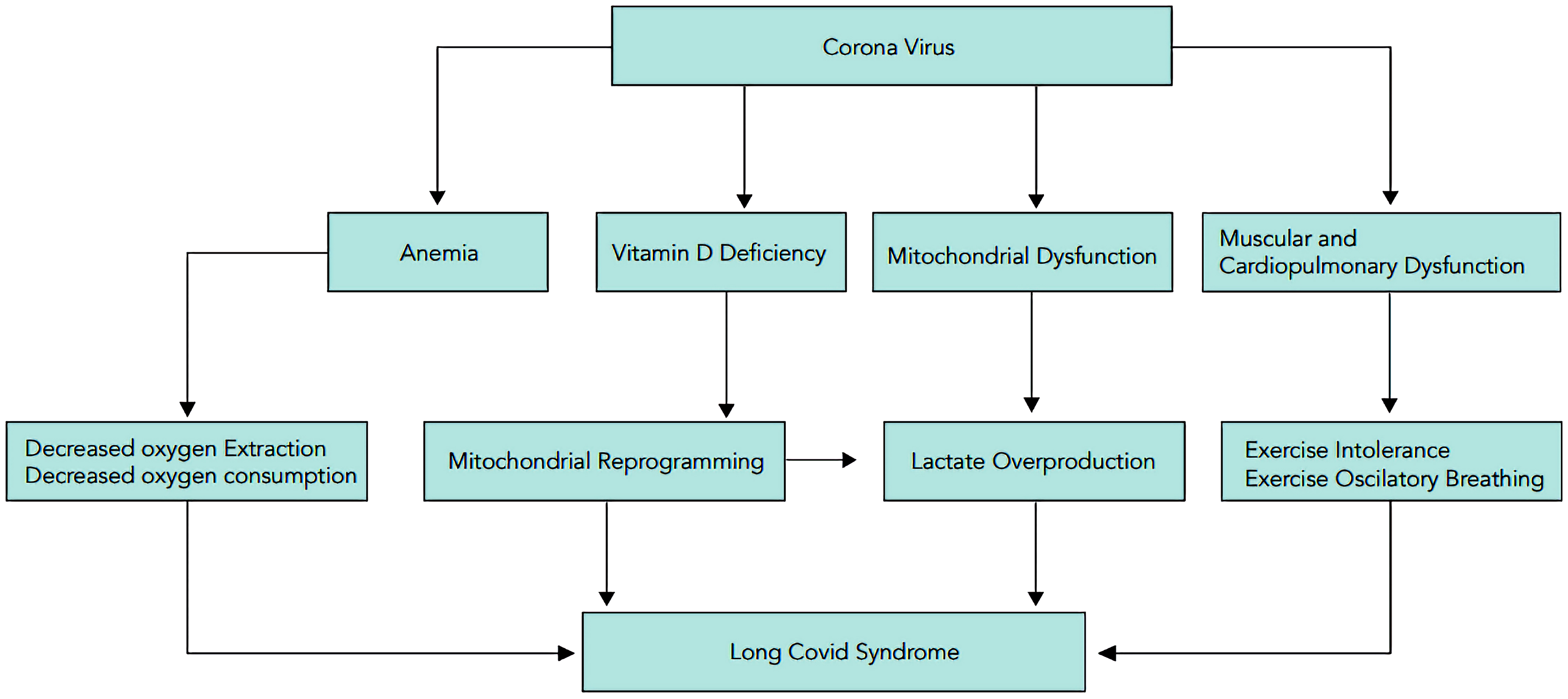 Click for large image | Figure 1. Proposed pathophysiology cascade of Long COVID syndrome. COVID: coronavirus disease. |
Current data indicate a significant association between vitamin D deficiency and COVID-19 susceptibility and severity. Numerous studies have suggested the benefit of vitamin D intake on ameliorating respiratory infections and COVID-19. Vitamin D supplementation is strongly recommended in order to avoid a cardiovascular outcome, optimize innate and adaptive immunity [25]. Current evidence suggests that taking a vitamin D supplement of at least 30 ng/mL can help reduce the risk of SARS-CoV-2 infection and its severe outcomes, including mortality.
On cellular basis, vitamin D inhibits apoptosis, predominantly of adipocytes by reducing expression of the mitochondrial uncoupling protein 2. Mitochondrial dysfunction due to vitamin D deficiency is critical in debilitated conditions because it decreases adenosine triphosphate formation and increases reactive oxygen species (ROS) generation. Moreover, vitamin D regulates the expression of adiponectin, a hormone with insulin-sensitizing and anti-inflammatory actions. In overall, cellular and systemic alterations due to vitamin D deficiency impair mitochondrial function, contributing to the progression and severity of COVID-19 [26].
| Conclusions | ▴Top |
CPET is especially useful tool to objectively identify the pathophysiology of exertional dyspnea, including in LC. A CPET with normal findings can provide increased comfort with physical activity. Furthermore, unresolved epidemiologic problems about the prevalence of decreased exercise capacity require further investigations and research in a larger scale. Since all CPET variables can provide a synergistic prognostic discrimination, it can certainly be used for further diagnostic approach, risk stratification and treatment strategy [27].
In overall, the summery of the current data suggest that exercise capacity is reduced after SARS-CoV-2 infection especially 3 - 6 months after hospitalization as well as among those with LC. We recommend further research studies in a larger scale to further clarify the trajectory of exercise capacity. Of special importance will be studies that will shed the light on potential therapies, improving conditioning, metabolic normalization, and recovering of mitochondrial function, as supplementation of vitamin D contributes to the normalization of mitochondrial function.
Acknowledgments
We deeply thank Mrs. Vasiliki Filippopoulou for providing assistance with the illustration of the article.
Financial Disclosure
This review was not supported by any foundation, grant maker or donor.
Conflict of Interest
None to declare.
Author Contributions
Stefanos G. Sakellaropoulos: main text, mitochondriopathy pathomechanisms, exercise oscillatory ventilation, illustration formation. Muhammad Ali, Athanasios Papadis, Muhemin Mohammed, Andreas Mitsis and Zaza Zivzivadze contributed to the review of main text.
Data Availability
Any inquiries regarding supporting data availability of this study should be directed to the corresponding author.
Abbreviations
BrP: breathing pattern; CHOox: oxidation of carbohydrates; CP: cardiopulmonary; CPET: cardiopulmonary exercise test; COVID19: coronavirus disease 2019; CRF: cardiorespiratory fitness; FATox: oxidation of fatty acids; LC: Long COVID; ROS: reactive oxygen species; SARS-CoV-2: severe acute respiratory syndrome coronavirus 2
| References | ▴Top |
- John Hopkins University Coronavirus Resource Center. https://coronavirus.jhu.edu/ [2022 Mar 3].
- Ayoubkhani D, Pawelek P. Prevalence of ongoing symptoms following coronavirus (COVID-19) infection in the UK: 3 February 2022 (Online). Off Natl Stat. 2022;1-6.
- Carfi A, Bernabei R, Landi F, Gemelli Against C-P-ACSG. Persistent symptoms in patients after acute COVID-19. JAMA. 2020;324(6):603-605.
doi pubmed - Brawner CA, Ehrman JK, Bole S, Kerrigan DJ, Parikh SS, Lewis BK, Gindi RM, et al. Inverse relationship of maximal exercise capacity to hospitalization secondary to coronavirus disease 2019. Mayo Clin Proc. 2021;96(1):32-39.
doi pubmed - Puntmann VO, Carerj ML, Wieters I, Fahim M, Arendt C, Hoffmann J, Shchendrygina A, et al. Outcomes of cardiovascular magnetic resonance imaging in patients recently recovered from coronavirus disease 2019 (COVID-19). JAMA Cardiol. 2020;5(11):1265-1273.
doi pubmed - Raman B, Cassar MP, Tunnicliffe EM, Filippini N, Griffanti L, Alfaro-Almagro F, Okell T, et al. Medium-term effects of SARS-CoV-2 infection on multiple vital organs, exercise capacity, cognition, quality of life and mental health, post-hospital discharge. EClinicalMedicine. 2021;31:100683.
doi pubmed - Silva RN, Goulart CDL, Oliveira MR, Tacao GY, Back GD, Severin R, Faghy MA, et al. Cardiorespiratory and skeletal muscle damage due to COVID-19: making the urgent case for rehabilitation. Expert Rev Respir Med. 2021;15(9):1107-1120.
doi pubmed - Ross R, Blair SN, Arena R, Church TS, Despres JP, Franklin BA, Haskell WL, et al. Importance of assessing cardiorespiratory fitness in clinical practice: a case for fitness as a clinical vital sign: a scientific statement from the American Heart Association. Circulation. 2016;134(24):e653-e699.
doi pubmed - Gao Y, Chen R, Geng Q, Mo X, Zhan C, Jian W, Li S, et al. Cardiopulmonary exercise testing might be helpful for interpretation of impaired pulmonary function in recovered COVID-19 patients. Eur Respir J. 2021;57(1):2004265.
doi pubmed - Ong KC, Ng AW, Lee LS, Kaw G, Kwek SK, Leow MK, Earnest A. Pulmonary function and exercise capacity in survivors of severe acute respiratory syndrome. Eur Respir J. 2004;24(3):436-442.
doi pubmed - Hui DS, Wong KT, Ko FW, Tam LS, Chan DP, Woo J, Sung JJ. The 1-year impact of severe acute respiratory syndrome on pulmonary function, exercise capacity, and quality of life in a cohort of survivors. Chest. 2005;128(4):2247-2261.
doi pubmed - Hui DS, Joynt GM, Wong KT, Gomersall CD, Li TS, Antonio G, Ko FW, et al. Impact of severe acute respiratory syndrome (SARS) on pulmonary function, functional capacity and quality of life in a cohort of survivors. Thorax. 2005;60(5):401-409.
doi pubmed - Ferrandi PJ, Alway SE, Mohamed JS. The interaction between SARS-CoV-2 and ACE2 may have consequences for skeletal muscle viral susceptibility and myopathies. J Appl Physiol (1985). 2020;129(4):864-867.
doi pubmed - Ferrandi PJ, Alway SE, Mohamed JS. Last Word on Viewpoint: The interaction between SARS-CoV-2 and ACE2 may have consequences for skeletal muscle viral susceptibility and myopathies. J Appl Physiol (1985). 2020;129(4):872.
doi pubmed - Sakellaropoulos S, Mitsis A. Cardiopulmonary exercise test-the revolving door of left ventricular assist devices in heart failure. Curr Probl Cardiol. 2021;46(3):100651.
doi pubmed - Froidure A, Mahsouli A, Liistro G, De Greef J, Belkhir L, Gerard L, Bertrand A, et al. Integrative respiratory follow-up of severe COVID-19 reveals common functional and lung imaging sequelae. Respir Med. 2021;181:106383.
doi pubmed - Lerum TV, Aalokken TM, Bronstad E, Aarli B, Ikdahl E, Lund KMA, Durheim MT, et al. Dyspnoea, lung function and CT findings 3 months after hospital admission for COVID-19. Eur Respir J. 2021;57(4):2003448.
doi pubmed - Naeije R, Caravita S. Phenotyping long COVID. Eur Respir J. 2021;58(2).
doi pubmed - Barbagelata L, Masson W, Iglesias D, Lillo E, Migone JF, Orazi ML, Maritano Furcada J. Cardiopulmonary exercise testing in patients with post-COVID-19 syndrome. Med Clin (Engl Ed). 2022;159(1):6-11.
doi - Skjorten I, Ankerstjerne OAW, Trebinjac D, Bronstad E, Rasch-Halvorsen O, Einvik G, Lerum TV, et al. Cardiopulmonary exercise capacity and limitations 3 months after COVID-19 hospitalisation. Eur Respir J. 2021;58(2):2100996.
doi pubmed - Baratto C, Caravita S, Faini A, Perego GB, Senni M, Badano LP, Parati G. Impact of COVID-19 on exercise pathophysiology: a combined cardiopulmonary and echocardiographic exercise study. J Appl Physiol (1985). 2021;130(5):1470-1478.
doi pubmed - Motiejunaite J, Balagny P, Arnoult F, Mangin L, Bancal C, d'Ortho MP, Frija-Masson J. Hyperventilation: a possible explanation for long-lasting exercise intolerance in mild COVID-19 survivors? Front Physiol. 2020;11:614590.
doi pubmed - Sakellaropoulos SG, Baggish AL, Fifer MA, Lewis GD. Exercise oscillatory ventilation in hypertrophic cardiomyopathy. Curr Probl Cardiol. 2022;47(5):100911.
doi pubmed - San-Millan I, Brooks GA. Assessment of metabolic flexibility by means of measuring blood lactate, fat, and carbohydrate oxidation responses to exercise in professional endurance athletes and less-fit individuals. Sports Med. 2018;48(2):467-479.
doi pubmed - Parikh S, Goldstein A, Koenig MK, Scaglia F, Enns GM, Saneto R, Anselm I, et al. Diagnosis and management of mitochondrial disease: a consensus statement from the Mitochondrial Medicine Society. Genet Med. 2015;17(9):689-701.
doi pubmed - Ayres JS. A metabolic handbook for the COVID-19 pandemic. Nat Metab. 2020;2(7):572-585.
doi pubmed - Sakellaropoulos S, Lekaditi D, Svab S. Cardiopulmonary exercise Test in heart failure: A Sine qua non. International Journal of Physical Education, Fitness and Sports. 2020;9(2):1-8.
doi
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cardiology Research is published by Elmer Press Inc.


