| Cardiology Research, ISSN 1923-2829 print, 1923-2837 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, Cardiol Res and Elmer Press Inc |
| Journal website https://www.cardiologyres.org |
Original Article
Volume 13, Number 4, August 2022, pages 236-241
The Association Between Admission Heart Failure and In-Hospital Outcomes in ST-Elevation Myocardial Infarction Patients Undergoing Primary Percutaneous Coronary Intervention
Amr Elkammasha, d , Mohamed Abdelhamidb, Mohamed Sobhyb, Amr Zakib, Mohamed Sadakab, Mustafa Alsinanc, Khaled Elbastawisic, Ahmed Abbasc, Khaled Madic
aDepartment of Cardiology, The Royal Papworth Hospital NHS Foundation Trust, Cambridge, UK
bDepartment of Cardiology, Alexandria Main University Hospital, Alexandria, Egypt
cDepartment of General Internal Medicine, University Hospitals Dorset NHS Foundation Trust, The Royal Bournemouth Hospital, Bournemouth, UK
dCorresponding Author: Amr Elkammash, Department of Cardiology, The Royal Papworth Hospital NHS Foundation Trust, Cambridge, CB2 0AY, UK
Manuscript submitted July 31, 2022, accepted August 8, 2022, published online August 15, 2022
Short title: HF and Outcomes in STEMI Patients Undergoing PPCI
doi: https://doi.org/10.14740/cr1414
| Abstract | ▴Top |
Background: The Global Registry of Acute Coronary Events (GRACE) study showed that admission HF is associated with longer hospital stay and higher mortality in ST-elevation myocardial infarction (STEMI) patients. No data are available on the effect of heart failure (HF) on the length of cardiac care unit (CCU) stay and in-hospital major adverse cardiac events (MACEs). The link between the severity of HF and the in-hospital prognosis is not established. Therefore, we aimed to investigate the unstudied outcomes in HF patients as well as to compare the outcomes across the spectrum of HF presentations.
Methods: We studied 210 STEMI patients presenting to a single primary percutaneous coronary intervention (PPCI) center in a retrospective cohort pattern. We excluded those who received fibrinolysis, those who had chest pain for more than 24 h and those with previous stents and presenting with stent thrombosis. All the procedures followed the ethical standards of Alexandria University and the Helsinki Declaration.
Results: STEMI patients with HF had significantly longer CCU stay (mean value of 3.6 vs. 2.87 days, P = 0.009), higher in-hospital MACE (55% vs. 4.7%, P < 0.001) and higher mortality (15% vs. 0.53%, P < 0.001). Multivariate logistic regression analysis revealed that HF is an independent predictor of in-hospital mortality (odds ratio (OR) = 9.11, 95% confidence interval (CI): 1.66 - 49.9, P = 0.01). The patients with severe HF on admission (Killip III and IV) tended to stay longer in the CCU (4.13 ± 1.89 days vs. 3.25 ± 1.54 days, P = 0.069) and the hospital (5.88 ± 3.09 vs. 4.42 ± 2.47 days, P = 0.077), compared to those with mild HF (Killip II). There was a tendency for a higher incidence of in-hospital MACE (75% vs. 33%, P = 0.068) and mortality (16.7% vs. 12.5%, P = 0.798) in the former group compared to the latter. The differences among HF subgroups did not reach the point of statistical significance though.
Conclusions: The presence of HF on the admission of STEMI patients undergoing PPCI is associated with longer CCU stay, higher in-hospital MACE and mortality.
Keywords: Heart failure; STEMI; CCU; Stay; MACE; Mortality; Primary PCI
| Introduction | ▴Top |
Death from cardiovascular diseases represents 32% of all global deaths [1]. In the UK, admissions due to cardiovascular diseases cost the budget 9 billion pounds every year [2]. The estimated cost of cardiac care unit (CCU) and adult cardiology ward admission is estimated to be $434 and $342 per day, respectively [3]. Therefore, planning the care of patients with acute cardiovascular diseases, such as ST-elevation myocardial infarction (STEMI), is paramount.
Acute heart failure (HF) in patients with STEMI has many causes, including myocardial stunning, myocardial necrosis, decompensation of pre-existing HF and acute mitral regurgitation due to papillary muscle dysfunction [4]. The GRACE study is a cornerstone study that investigated the length of hospital stay and mortality in ACS patients with and without HF. However, the study did not study other important prognostic variables such as in-hospital major adverse cardiac events (MACEs) and length of CCU stay. It did not compare the outcomes between patients with mild and severe HF on presentation [5].
We designed our study to fill this gap of evidence not illustrated in the GRACE study. We studied STEMI patients and investigated the link between acute HF and different clinical outcomes post primary percutaneous coronary intervention (PPCI) including length of CCU stay, length of hospital stay, in-hospital MACEs, and mortality. We also compared these variables in different severities of HF.
| Materials and Methods | ▴Top |
This is an observational retrospective cohort study. We included 210 consecutive STEMI patients eligible for PPCI according to the European Society of Cardiology (ESC) guidelines who presented to a large-volume tertiary cardiac center (The international Cardiac Centre, Alexandria, Egypt) [6]. We excluded patients who received fibrinolysis, those who had previous PCI and presented with acute stent thrombosis and those who presented more than 24 h from the onset of pain. We divided the recruited patients into two groups based on their Killip class at the time of presentation to the emergency department (Killip I and Killip ≥ II) [7]. We compared the two groups with regard to various cardiovascular risk factors. We also compared the length of CCU stay, the total length of hospital stay, in-hospital MACEs, and mortality in them.
We stratified the HF group according to the severity of presentation into two groups; the patients with mild HF (Killip II) and those with severe HF and/or cardiogenic shock (Killip III - IV). We studied the HF strata for the length of CCU and hospital stay, in-hospital MACEs, and mortality. The definition of MACE includes HF, major bleeding, target vessel revascularisation (TVR), reinfarction and cerebrovascular stroke. The major bleeding indicates clinically overt bleeding accompanied by a decrease in the hemoglobin level of 2 g/dL or more or requiring the transfusion of two or more units of packed red cells, occurring at a critical site or resulting in death [8].
Ethical issues and informed consent
All procedures of the present study were conducted in compliance with the Helsinki Declaration for research on human beings. The study was approved by the Research Ethics Committee at Alexandria University, Egypt (number 783006/22).
Statistics
A professional statistician did the statistical analysis using IBM SPSS 21.0 software (SPSS, Chicago, IL, USA). Quantitative data were expressed using mean, standard deviation, and median while qualitative data were expressed in frequency and percent. Qualitative data were analyzed using the Chi-square test. Non-normally distributed quantitative data were analyzed using the Mann-Whitney test for comparing the two groups. The P value was assumed to be significant at 0.05.
| Results | ▴Top |
There were 190 patients in the Killip I group and 20 patients in the Killip ≥ II group. The studied groups did not differ significantly regarding the different cardiovascular risk factors including diabetes, hypertension, smoking, dyslipidaemia and previous stroke or myocardial infarction (Table 1).
 Click to view | Table 1. Clinical Characteristics of the Studied Groups |
The HF group had a significantly longer CCU stay (mean value of 3.6 vs. 2.87 days, P = 0.009), a higher incidence of in-hospital MACEs (55% vs. 4.7%, P < 0.001) and death (15% vs. 0.53%, P < 0.001) (Figs. 1-3). They stayed longer in the hospital compared to those without; such a difference did not reach the point of statistical significance (mean value of 5 vs. 4.17 days, P = 0.124) (Fig. 4). The multivariate logistic regression analysis showed that admission HF is an independent predictor of in-hospital mortality (odds ratio (OR) = 9.11, 95% confidence interval (CI): 1.66 - 49.9, P = 0.01) (Table 2).
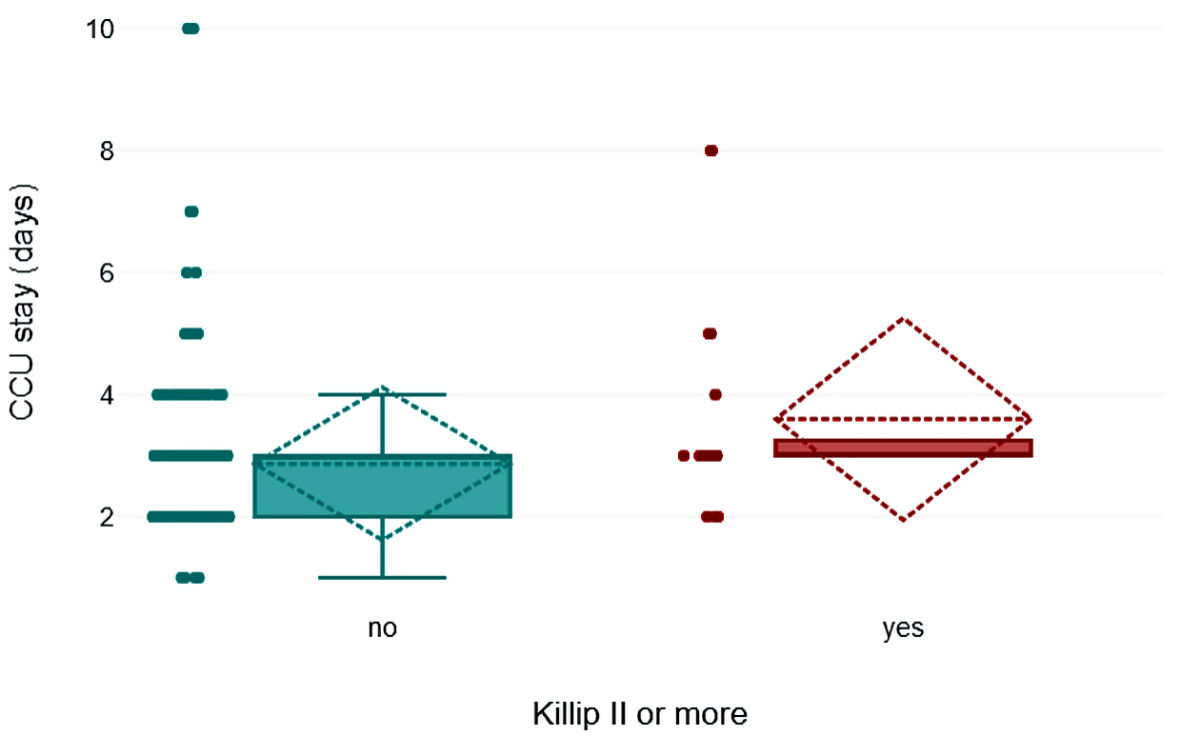 Click for large image | Figure 1. The length of CCU stay in STEMI patients with and without heart failure. CCU: coronary care unit; STEMI: ST-elevation myocardial infarction. |
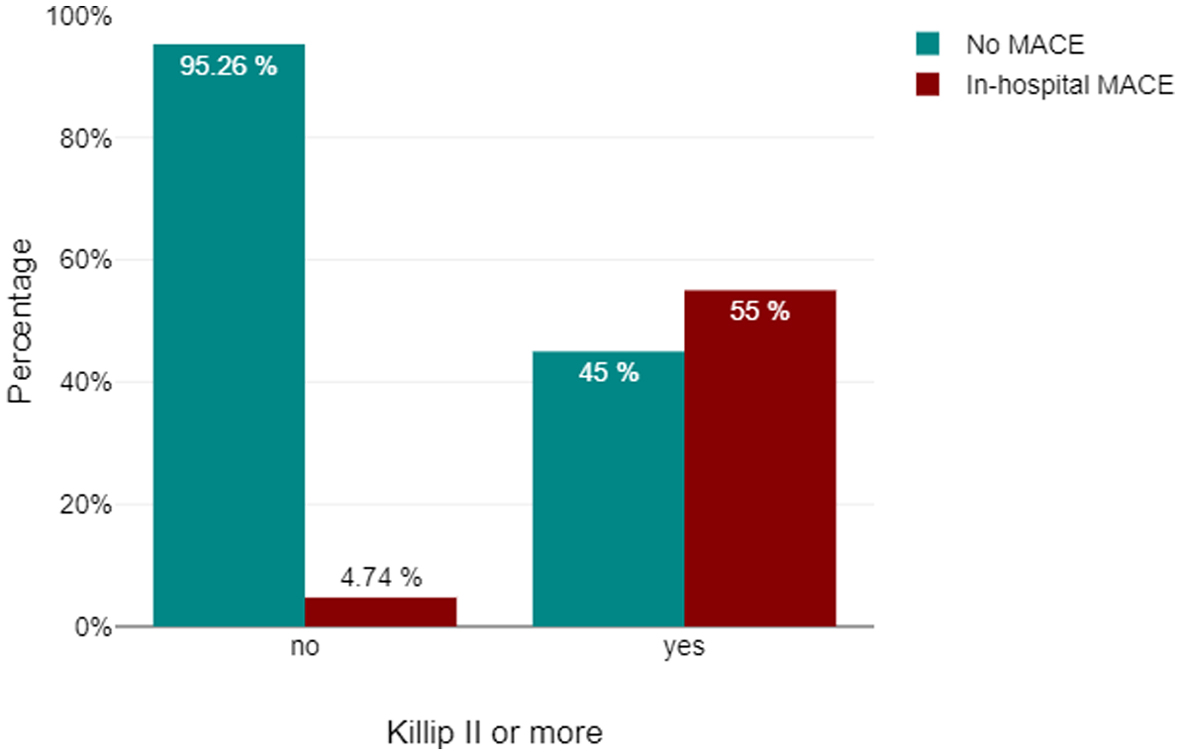 Click for large image | Figure 2. In-hospital MACEs in STEMI patients with and without heart failure. MACEs: major adverse cardiac events; STEMI: ST-elevation myocardial infarction. |
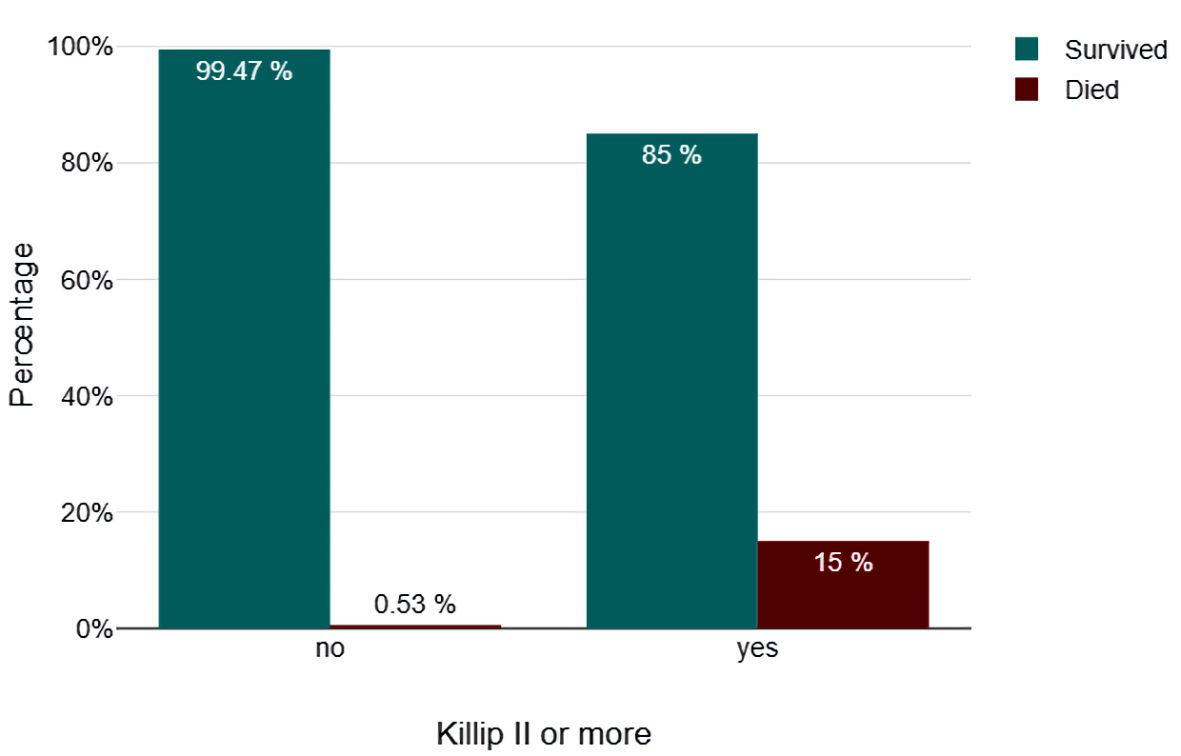 Click for large image | Figure 3. Mortality in STEMI patients with and without heart failure. STEMI: ST-elevation myocardial infarction. |
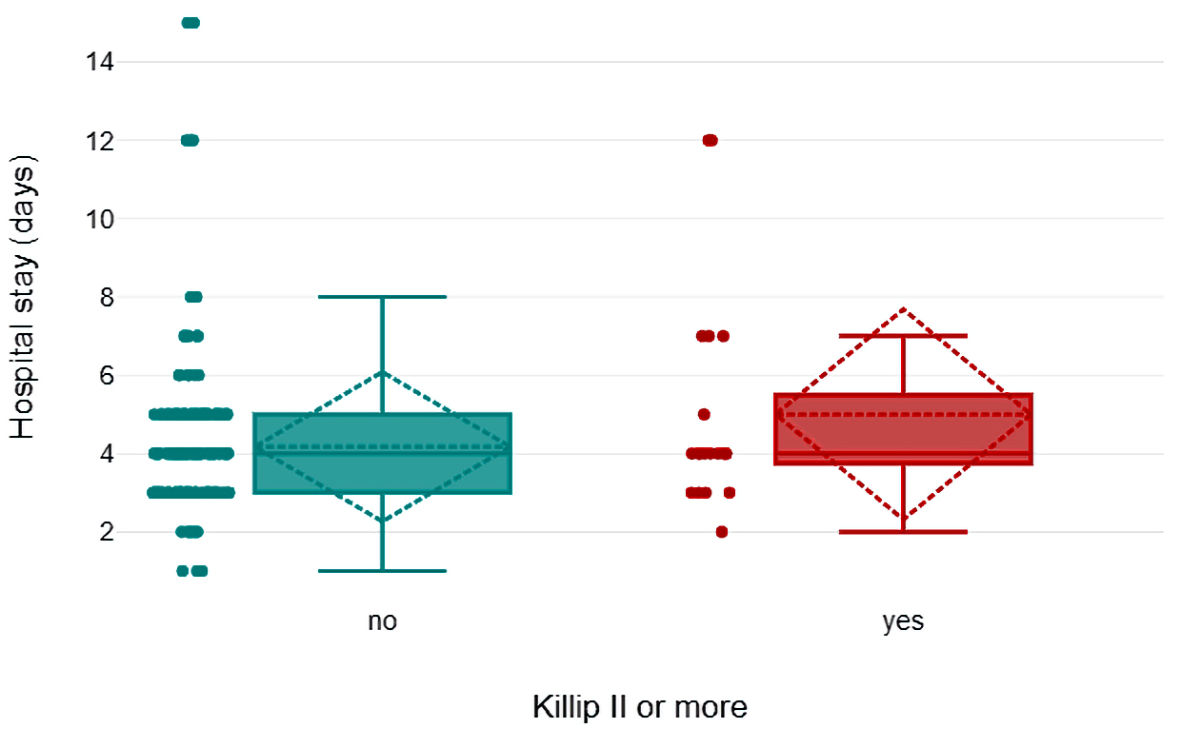 Click for large image | Figure 4. The length of hospital stay in STEMI patients with and without heart failure. STEMI: ST-elevation myocardial infarction. |
 Click to view | Table 2. The Length of CCU and Hospital Stay, the In-Hospital MACE, and Mortality in Patients With and Without Heart Failure |
When we compared the patients with mild HF to those with a severe presentation, we found the latter group tended to stay longer in the CCU (4.13 ± 1.89 days vs. 3.25 ± 1.54 days, P = 0.069) and the hospital (5.88 ± 3.09 vs. 4.42 ± 2.47 days, P = 0.077). They also had a higher incidence of in-hospital MACEs (75% vs. 33%, P = 0.068) and mortality (16.7% vs. 12.5%, P = 0.798) compared to those with milder presentation. The P value did not achieve the point of statistical significance though (Table 3).
 Click to view | Table 3. The CCU and Hospital Stay and In-Hospital MACE and Mortality Across Different Grades of Heart Failure |
| Discussion | ▴Top |
Our study demonstrates the association between admission HF in STEMI patients undergoing PPCI and prolonged CCU and hospital stay, increased in-patient MACEs and death. It also shows a tendency towards worse outcomes in higher Killip classes.
We demonstrated that STEMI patients with HF on admission had a significantly longer CCU stay rather than the crude hospital stay. This is a more robust marker of the prognosis due to the higher costs of CCU care. The crude hospital stay can be prolonged for other reasons such as post STEMI rehabilitation and social issues. The GRACE study demonstrated that STEMI patients with admission HF had longer hospital stay than those without [5]. It did not look specifically into the length of CCU stay, which has a much higher cost of care compared to ward admission [3].
Our study highlighted the higher in-hospital MACEs and death in STEMI patients with HF. The MACEs were mainly in the form of post-PPCI HF and major bleeding. Patients with Killip III and IV HF had a higher incidence of MACEs, although the P value did not reach the value of statistical significance. The small number of the recruited patients might be responsible for that. A possible explanation for the higher MACEs and mortality may be the impaired coronary perfusion in patients with HF even after a successful PCI. HF causes coronary vasoconstriction by the release of neurohumoral factors (endothelin, angiotensin, and norepinephrine). In addition, it reduces the release of endothelium-derived vasodilator agents such as nitric oxide [9]. Another explanation can be the STEMI-induced myocardial damage in patients with pre-existing HF, leading to further myocardial compromise. The GRACE study also showed increased in-hospital mortality in STEMI patients who had HF at admission [5]. It showed that the mortality was even higher in those who developed HF during hospitalization compared to those who had HF at admission.
Study limitations
The study is limited by the small number of recruited patients. The difference in outcomes among HF patients of different severity may become significant in a larger sample size. Other limitations include the retrograde analysis and the small geographical area of recruitment. Larger prospective studies are needed to further identify markers of prognosis in STEMI patients post PPCI. In this study, we defined HF based on the clinical findings in the admitted patients. Inclusion of echocardiographic parameters to differentiate categories of HF (heart failure with preserved ejection fraction (left ventricular ejection fraction (LVEF) ≥ 50%) (HFpEF), HF with mid-range ejection fraction (LVEF 41-49%) (HFmrEF), and HF with reduced ejection fraction (LVEF ≤ 40%) (HFrEF)) could have added more depth to the results of the study.
Conclusions
In summary, HF is a simple clinical marker to predict the risks of prolonged CCU, in-hospital MACEs and death in STEMI patients undergoing PPCI. More severe HF may even carry worse outcomes. These findings are important in planning their medical care.
Acknowledgments
None to declare.
Financial Disclosure
This research has not received any specific funding or grants.
Conflict of Interest
None to declare.
Informed Consent
Informed consent was obtained from all participants.
Author Contributions
MA conceptualized the research project. AE, M. Alsinan, AA, KM, and KE reviewed the literature. M. Abdelhamid collected the data. AE, M. Alsinan, AA, KM, and KE aided in the statistical analysis. AE wrote the first draft. M. Sobhy, AZ, and M. Sadaka critically reviewed the manuscript. AE revised and submitted the manuscript.
Data Availability
All the data supporting the findings of this study is available upon appropriate request to the corresponding author.
Abbreviations
HF: heart failure; PPCI: primary percutaneous coronary intervention; PCI: percutaneous coronary intervention; STEMI: ST-elevation myocardial infarction; GRACE: Global Registry of Acute Coronary Events; CCU: coronary care unit; TVR: target vessel revascularisation; MACEs: major adverse cardiac events; MI: myocardial infarction; CVA: cerebrovascular accident; IDDM: insulin-dependent diabetes mellitus; NIDDM: non-insulin-dependent diabetes mellitus; ESC: European Society of Cardiology; SD: standard deviation; HFpEF: heart failure with preserved ejection fraction (left ventricular ejection fraction (LVEF) ≥ 50%); HFmrEF: heart failure with mid-range ejection fraction (LVEF 41-49%); HFrEF: heart failure with reduced ejection fraction (LVEF ≤ 40%)
| References | ▴Top |
- Cardiovascular diseases (CVDs). https://www.who.int/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds). Accessed July 26, 2022.
- Heart statistics - heart and circulatory diseases in the UK | BHF. https://www.bhf.org.uk/what-we-do/our-research/heart-statistics. Accessed July 30, 2022.
- Kumar A, Siddharth V, Singh SI, Narang R. Cost analysis of treating cardiovascular diseases in a super-specialty hospital. PLoS One. 2022;17(1):e0262190.
doi pubmed - Cahill TJ, Kharbanda RK. Heart failure after myocardial infarction in the era of primary percutaneous coronary intervention: Mechanisms, incidence and identification of patients at risk. World J Cardiol. 2017;9(5):407-415.
doi pubmed - Steg PG, Dabbous OH, Feldman LJ, Cohen-Solal A, Aumont MC, Lopez-Sendon J, Budaj A, et al. Determinants and prognostic impact of heart failure complicating acute coronary syndromes: observations from the Global Registry of Acute Coronary Events (GRACE). Circulation. 2004;109(4):494-499.
doi pubmed - Ibanez B, James S, Agewall S, Antunes MJ, Bucciarelli-Ducci C, Bueno H, Caforio ALP, et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: the task force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2018;39(2):119-177.
doi pubmed - Killip T, 3rd, Kimball JT. Treatment of myocardial infarction in a coronary care unit. A two year experience with 250 patients. Am J Cardiol. 1967;20(4):457-464.
doi - Schulman S, Kearon C, Subcommittee on Control of Anticoagulation of the Scientific Standardization Committee of the International Society on Thrombosis Haemostasis. Definition of major bleeding in clinical investigations of antihemostatic medicinal products in non-surgical patients. J Thromb Haemost. 2005;3(4):692-694.
doi pubmed - Heusch G. Coronary blood flow in heart failure: cause, consequence and bystander. Basic Res Cardiol. 2022;117(1):1.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cardiology Research is published by Elmer Press Inc.


