| Cardiology Research, ISSN 1923-2829 print, 1923-2837 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, Cardiol Res and Elmer Press Inc |
| Journal website https://www.cardiologyres.org |
Case Report
Volume 13, Number 1, February 2022, pages 65-70
“Broken Heart” and “Broken Brain”: Which Connection?
Athanasios Papadisa, c, Stefano Svaba, c, Nicolas Bruggera, Jonas Lanza, Robert von Arxa, Konstantinos Stamoub, Stefanos Sakellaropoulosa, d
aSwiss Cardiovascular Centre, Bern University Hospital, Bern, Switzerland
bSchool of Medicine, Faculty of Health Sciences, Aristotle University of Thessaloniki, Thessaloniki, Greece
cBoth authors have equally contributed to this article.
dCorresponding Author: Stefanos Sakellaropoulos, Swiss Cardiovascular Centre, Bern University Hospital, Bern, Switzerland;
Manuscript submitted November 22, 2021, accepted December 7, 2021, published online December 28, 2021
Short title: “Broken Heart” and “Broken Brain”
doi: https://doi.org/10.14740/cr1336
| Abstract | ▴Top |
The interconnections between brain and heart are increasingly recognized. Takotsubo cardiomyopathy, also known as “broken heart syndrome”, is characterized by a cardiovascular dysfunction provoked by an emotional or stressful situation. Similar events can trigger a neurological pathology called transient global amnesia. These conditions can occur simultaneously, although their precise connection is not well understood. We aim to present the case of a patient who experienced them and to review the relevant literature.
Keywords: Takotsubo cardiomyopathy; Transient global amnesia; Neurocardiology; Neurologic stunned myocardium; Broken heart syndrome; Stress cardiomyopathy; Anterograde amnesia; Cerebral dysfunction; Transient loss of memory
| Introduction | ▴Top |
Established by Natelson in 1985, the term neurocardiology is becoming increasingly popular in modern medicine [1], as the awareness over interconnections between central nervous system (CNS) and heart becomes widespread. Nevertheless, many aspects of this connection remain obscure.
| Case Report | ▴Top |
We report the case of a 75-year-old woman, known for tachycardia-bradycardia syndrome in the context of atrial fibrillation, which required a pacemaker implantation 1 year previously. The patient was also known for arterial hypertension (treated with double therapy with sartan and chlortalidon) and dyslipidemia treated with a statin. At the time of pacemaker implantation, she had a normal heart function in the echocardiography and she remained asymptomatic thereafter.
After an acute stress during a job meeting, she developed acute disorientation in time and space and asked repetitive questions. She was thus admitted to the emergency department where, due to persistent disorientation and new onset of strabismus, an intracranial bleeding was ruled out with native computed tomography (CT) scan. The neurological status recovered rapidly and the diagnosis of transient global amnesia (TGA) was made [2, 3]. She was hemodynamically stable, with minimal peripheral edema and otherwise unremarkable examination. Due to diffuse T-wave inversion on the electrocardiogram (ECG) and elevated troponin values, an echocardiogram was performed, which showed a moderately reduced ejection fraction (EF) with antero-apical akinesia (Fig. 1a-c). Because of a high cardiovascular risk, new wall motion abnormalities and low InterTAK score (60 points) [4], an obstructive coronary artery disease was excluded by means of invasive coronary angiography (Fig. 2). The left ventricular angiography documented an apical ballooning (Fig. 1d). The patient was discharged after 24 h, with increased sartan therapy and new beta-blocker (BB) therapy. At a follow-up after 2 months, she was asymptomatic and the cardiac function had completely recovered (Fig. 3): the diagnosis of Takotsubo cardiomyopathy (TTC) was thus confirmed.
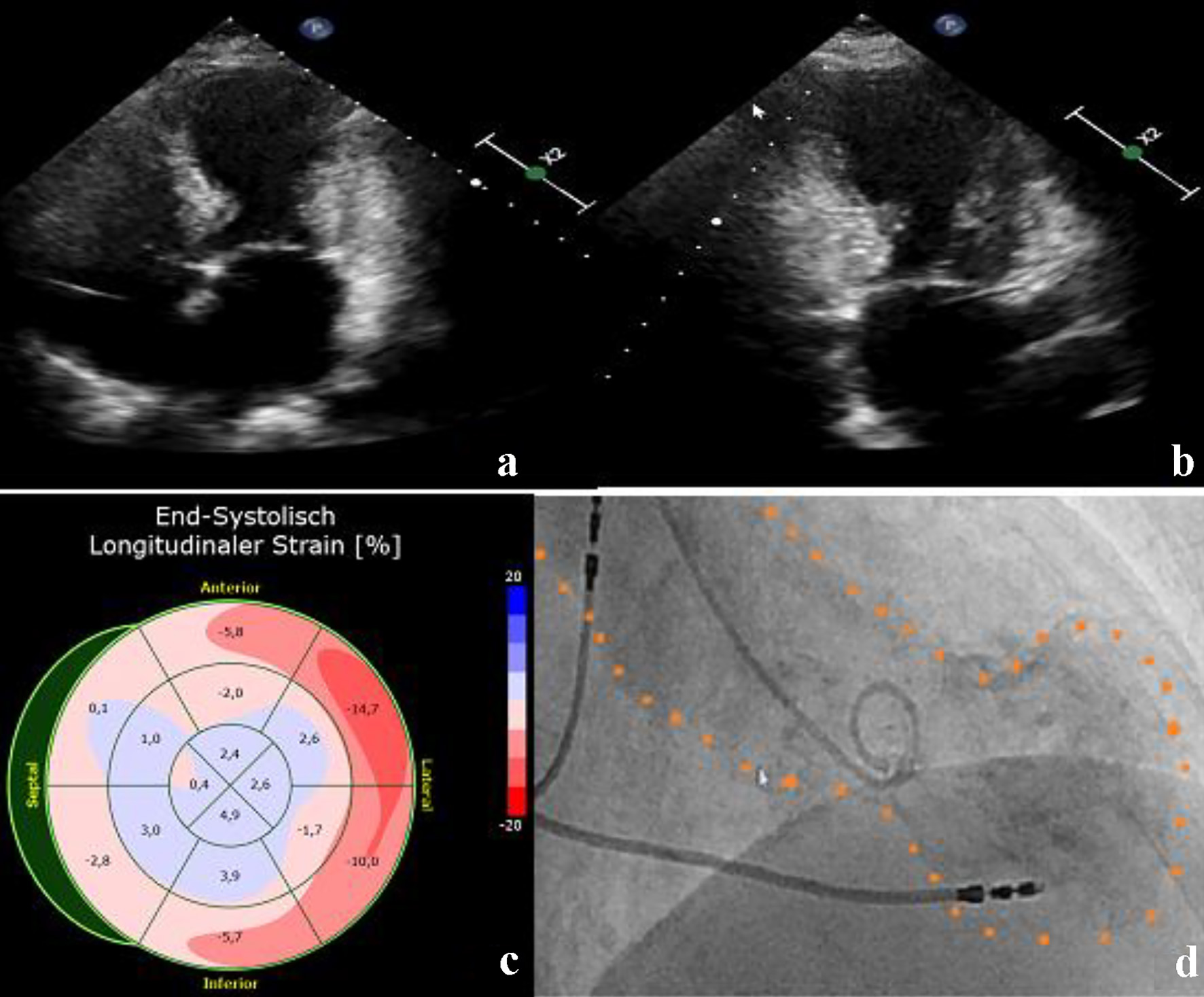 Click for large image | Figure 1. (a, b) Apical four- and two-chamber views on TTE on admission. (c) GLS on TTE on admission. (d) Left ventricular angiography. Apical akinesia (apical ballooning) can be appreciated in all. TTE: transthoracic echocardiography; GLS: global longitudinal strain. |
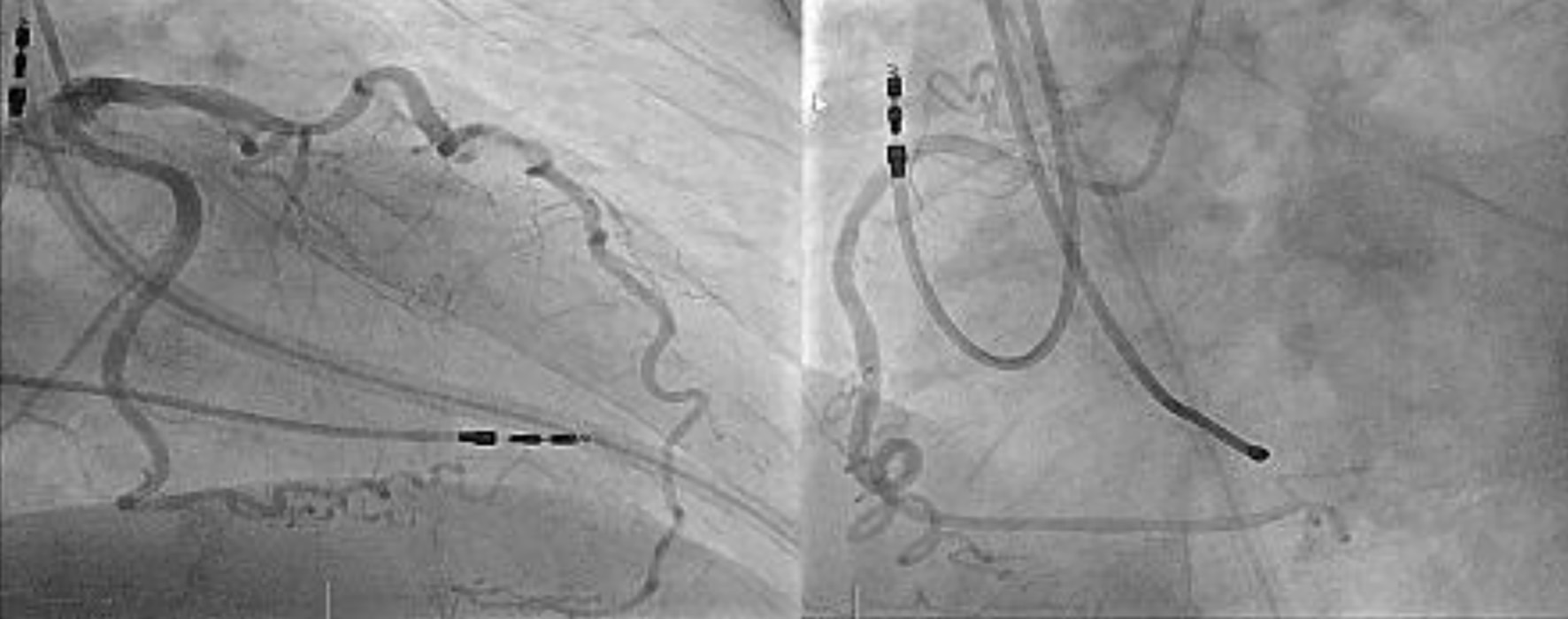 Click for large image | Figure 2. Tortuous coronary arteries without relevant stenosis. |
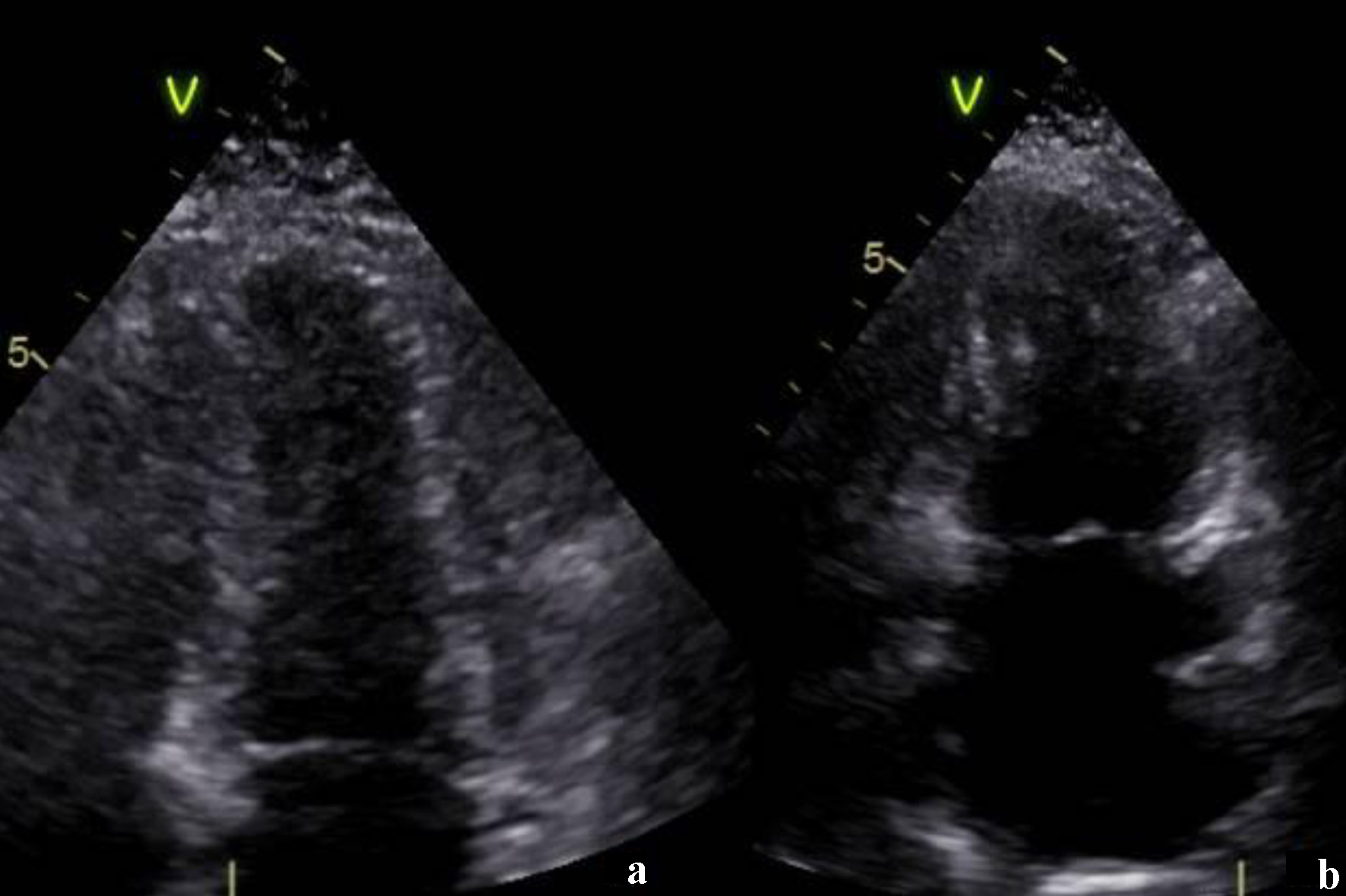 Click for large image | Figure 3. (a, b) Follow-up of apical four- and two-chamber view, respectively. Normalization of left ventricular geometry with no apical ballooning. |
| Discussion | ▴Top |
Our patient was diagnosed with TGA and TTC concomitantly. Intuitively, a connection between the two entities can be suspected, as both have been linked to stress situations. Indeed, similar clinical scenarios have already been reported [5, 6], and TTC has been associated with a two-fold increased risk for TGA [7]. However, the exact mechanism of both TGA and TTC is still not entirely understood, and thereby also the interconnection between the two pathological entities remains partially obscure.
The brain can exert control over the heart through different pathways [8, 9]. The “neuro-cardiac axis”, consisting of the prefrontal cortex, amygdala, insular cortex, the anterior cingulate cortex and the brainstem, is involved in the control of the autonomic nervous system, and different pathological events in these areas such as ischemic insults, epileptic seizures or tumors can elicit cardiac effects [10]. In addition, some neural reflexes can evoke cardiac responses. The most known is probably the vagal reflex, which leads to sudden bradycardia, depression of cardiac function and vasodilation resulting in hypotension. This can be triggered either by an emotional or a painful event through the motor nucleus of the vagus, or by ventricular mechanoreceptors in response to an increased inotropic state. Another neuro-cardiac reflex is the Cushing reflex [11], due to a rise of the intracranial pressure. The consequent CNS hypoperfusion triggers a sympathetic stimulation through the thalamus to increase the arterial blood pressure and thus brain perfusion, which in turn leads to a reflex bradycardia due to a carotid baroreceptors stimulation. A third reflex is the trigemino-cardiac reflex [12], initiated by the stimulation of the sensory branches of the trigeminal nerve resulting in cerebral vasodilation, bradycardia and hypotension, probably as a response to the excitation of oxygen-sensitive neurons in the rostral ventrolateral medulla oblongata.
Pathological responses in the CNS can elicit, mainly through these mechanisms, abnormal effects in heart function, such as alteration of blood pressure and cardiac rhythm, alteration in the conduction of the electric impulses and (mainly transient) cardiomyopathies. Although a univocal classification of these cardiomyopathies is still not available, two main entities have been described: the neurologic stunned myocardium (NSM) [13] and the TTC [4, 14]. In both, the pathophysiological mechanism resides probably in a catecholamine storm, triggered by an acute neurological injury in NSM (mainly in the caudal ventrolateral medulla, the tractus solitarius, the dorsal motor vagal nucleus and the posterior hypothalamus), by emotional or physical stress with consequent activation of hypotalamo-pituitary-adrenal and sympatho-adrenomedullary axis in TTC. The second mechanism could lead primarily to an increase in circulating blood catecholamines secreted from the adrenal medulla, whereas the first one could primarily be mediated from ventricular sympathetic nerve fiber terminals releasing norepinephrine. Sympathetic nerve fiber density and beta receptors for circulating adrenaline show an inverse pattern in the myocardium, the nerve fibers being more dense in the basal myocardium and the receptors for circulating adrenaline being more common in the apex. This observation could explain the preferential involvement of basal myocardium in NSM and of the apical myocardium in TTC as well as cases of patients with TTC despite normal circulating catecholamines. Alternative mechanisms have been evoked in order to explain TTC, such as immune-mediated or cytokine-mediated mechanisms and alterations in ion channels. Also a genetic predisposition seems to play a role [15].
TGA is a clinical syndrome characterized by the acute onset of anterograde amnesia. There is no consensus regarding a common underlying pathogenesis of TGA, but hypotheses include a vascular etiology (arterial or venous), a migrainous phenomenon (or cortical spreading depression), epilepsy, or a psychogenic disorder [2, 3].
In conclusion, a single, common pathological pathway between TTC and TGA is not self-evident. In particular, it is unclear whether there is a common cause (a single factor such as stress that could explain both conditions) or if one condition (such as TGA) could elicit the other (for example TTC). Although a higher catecholamine level has been described in patients with stress condition and other neurological and psychiatric disorders, its exact role in the pathogenesis of TGA is unclear.
Interestingly, it has been noted that the emotional stress triggering activation of the autonomic nervous system is mediated by two neurohumoral axes. Acutely, the sympathetic-adrenal-medulla axis leads to catecholamine release in the adrenal medulla. Chronically, the hypothalamic-pituitary-adrenal axis leads to cortisol release from the adrenal cortex. Notably, low cortisol blood levels have been reported in patients with chronic stress as a compensatory mechanism to avoid hypercortisolism. Thus, the inhibitory effects of catecholamine-release through high cortisol blood levels disappear in those patients, thus leaving the adrenaline effect on the entire body, and particularly on the heart, unbalanced [8]. However, in order to further elucidate the neuroendocrinological mechanisms in TTC, further studies are warranted.
Another pathophysiological hypothesis was described from neuroanatomical studies of TTC patients, which showed decreased resting functional connectivity in some areas of parasympathetic and sympathetic networks, hypothesized to play a role in TGA [16, 17].
Rationale for BB
Our patient was medically treated with BB and angiotensin II receptor blockers (ARBs). Several studies have sought to determine if BBs are beneficial in patients with Takotsubo syndrome (TTS). BBs are a logical choice, given their protective effect against cardiac remodeling in post-acute myocardial infarction and heart failure patients but they are also proposed to protect against TTS, considering the above mentioned role of catecholamines in the syndrome.
The rationale for BB therapy therefore has the following scopes: 1) prevention of vasospasm by the usage of BBs with concomitant α-blockade action such as carvedilol, labetalol or bucindolol; 2) prevention of catecholamine toxicity by causing a reduction of cardiac and systemic adrenergic drive, as previously demonstrated in the setting of HF; and 3) finally, attenuation of the depressed myocardial contractility, which might then promote the recovery from left ventricular (LV) dysfunction while inhibiting the detrimental β1 activation [18-20].
There are numerous studies showing benefit from the usage of BBs in the context of TTS although most of them are observational. Yasar et al published in 2020 a big meta-analysis of all the recent observational studies and clinical trials and concluded that BB therapy is indicated in most of the TTS patients [21, 22]. The observational study from Komlavi et al in year 2016, which investigated the acute and post-discharge management of TTS was also included. This study proved that beta-blockers among others together with psychological stress relief help to lower inpatient mortality and recurrence of TTS [23]. In other studies, it was confirmed that BB could help reverse the repolarization changes observed in TTS [24] as well as prevent cardiac rupture [25]. BBs should be started especially in patients with left ventricular outflow tract obstruction (LVOTO) to reduce the basal hypercontractility according to Chazal et al [26].
The beneficial effect was also shown in a study of Silverio et al [27] with a bigger population (n = 548). For the composite of cardiac death and rehospitalization landmark analysis showed a wider survival benefit in the BB patients after 2 years. The same study showed absence of a secondary preventive effect on TTS recurrence even though BBs may improve the long-term cardiac outcome in patients with TTS. That was previously also shown in older meta-analyses [28-30].
There was no benefit concerning mortality for BB therapy above 3 months something that was pointed out in an older study by Fazio et al in 2008 but also confirmed by a newer study from Abanador-Kamper et al in 2017 [31, 32]. Also in a large multinational review, Tempin et al found that there was no evidence of survival benefit at 1 year from use of a BB at discharge but also no particular benefit in preventing recurrence [33]. Similarly, a later Mayo Clinic study of 265 patients with TTS found no association between BB use at discharge and survival [34]. Observational data coming from numerous studies suggested that use of BBs might not even improve in-hospital mortality [35].
A recent publication from Santoro et al in 2021 [36], however, pointed out that BB could generally have an impact on survival but there is still lack of evidence for their usage. According to this article there is, however, limited retrospective evidence that the BB could have a benefit on the 1-year survival of patients with cardiogenic shock because of TTS. Finally, for the patients with LVOTO in the acute phase of TTS, there is again lack of evidence for the long-term benefit of BB.
Conclusions
The current case is a good example of the connection between TTC and TGA and raises Awareness for the possibility of a concomitant cardiac pathology in asymptomatic patients with primary neurological conditions seems to be important. Therapeutic consequences of the early recognition of the TTC have already been thoroughly described [4, 14].
The present case also raises questions about the exact connection between TTC and TGA, which is perceivable at a first look, but indeed not well understood. Further studies are thus warranted to better explain the two conditions and their relation.
Concerning the medical therapy of TTS it is clear that there is until to date no enough data to define an optimal medical regimen for stress cardiomyopathy. All of the previously mentioned studies, concerning BBs and other therapies, are retrospective in nature, and their observational mixed findings highlight the need for prospective randomized studies since the results have been inconclusive and not sufficient to define therapy.
We generally treat hemodynamically stable patients with standard medications for heart failure with reduced EF, especially as the diagnosis may not be definitive at the time of presentation. These should include beta-blocker therapy and that is the consensus opinion based on the last studies. Since the condition may recur, we tend to favor continuing adrenergic blockade until normalization of the contractility of left ventricle in the absence of contraindications or intolerance. However, there is currently no therapy at discharge that proved to reduce the incidence of recurrence at follow-up.
Acknowledgments
We thank our colleges from Inselspital for providing the images.
Financial Disclosure
None to declare.
Conflict of Interest
None to declare.
Informed Consent
Written informed consent was obtained from the patient to publish this report in accordance with the journal’s patient consent policy.
Author Contributions
Athanasios Papadis, Robert von Arx and Konstantinos Stamou have contributed to the article concerning case report, discussion and rational for beta-blocker. Nicolas Brugger has contributed to the article concerning echocardiography modalities. Jonas Lanz has contributed to the article concerning invasive diagnostics. Stefanos Sakellaropoulos and Stefano Svab have contributed to the article concerning article design, providing clinical expertise to revise critically.
Data Availability
The data are available from the corresponding author upon reasonable request.
Abbreviations
ECG: electrocardiogram; EF: ejection fraction; CNS: central nervous system; GLS: global longitudinal strain; NSM: neurologic stunned myocardium; TTC: Takotsubo cardiomyopathy; TTE: transthoracic echocardiography; TGA: transient global amnesia; BB: beta-blocker
| References | ▴Top |
- Natelson BH. Neurocardiology. An interdisciplinary area for the 80s. Arch Neurol. 1985;42(2):178-184.
doi pubmed - Bartsch T, Deuschl G. Transient global amnesia: functional anatomy and clinical implications. Lancet Neurol. 2010;9(2):205-214.
doi - Spiegel DR, Smith J, Wade RR, Cherukuru N, Ursani A, Dobruskina Y, Crist T, et al. Transient global amnesia: current perspectives. Neuropsychiatr Dis Treat. 2017;13:2691-2703.
doi pubmed - Ghadri JR, Wittstein IS, Prasad A, Sharkey S, Dote K, Akashi YJ, Cammann VL, et al. International expert consensus document on takotsubo syndrome (part II): diagnostic workup, outcome, and management. Eur Heart J. 2018;39(22):2047-2062.
doi pubmed - Finsterer J, Stollberger C. Simultaneous transient global amnesia and Takotsubo syndrome after death of a relative: a case report. J Med Case Rep. 2019;13(1):22.
doi pubmed - Grautoff S, Sitzer M, Weitkamp P, Kahler J. [Transient global amnesia and Tako-Tsubo cardiomyopathy—coincidence or corollary?]. Dtsch Med Wochenschr. 2012;137(44):2256-2259.
doi pubmed - Morris NA, Chatterjee A, Adejumo OL, Chen M, Merkler AE, Murthy SB, Kamel H. The risk of Takotsubo cardiomyopathy in acute neurological disease. Neurocrit Care. 2019;30(1):171-176.
doi pubmed - Kastaun S, Gerriets T, Tschernatsch M, Yeniguen M, Juenemann M. Psychosocial and psychoneuroendocrinal aspects of Takotsubo syndrome. Nat Rev Cardiol. 2016;13(11):688-694.
doi pubmed - Prasad Hrishi A, Ruby Lionel K, Prathapadas U. Head rules over the heart: cardiac manifestations of cerebral disorders. Indian J Crit Care Med. 2019;23(7):329-335.
doi pubmed - Ardell JL, Andresen MC, Armour JA, Billman GE, Chen PS, Foreman RD, Herring N, et al. Translational neurocardiology: preclinical models and cardioneural integrative aspects. J Physiol. 2016;594(14):3877-3909.
doi pubmed - Heymans C. The control of heart rate consequent to changes in the cephalic blood pressure and in the intracranial pressure. Am J Physiol. 1928;85:498-505.
doi - Chowdhury T, Mendelowith D, Golanov E, Spiriev T, Arasho B, Sandu N, Sadr-Eshkevari P, et al. Trigeminocardiac reflex: the current clinical and physiological knowledge. J Neurosurg Anesthesiol. 2015;27(2):136-147.
doi pubmed - Ali A, Ahmad MQ, Malik MB, Alvi ZZ, Iftikhar W, Kumar D, Nasir U, et al. Neurogenic Stunned Myocardium: A Literature Review. Cureus. 2018;10(8):e3129.
doi - Ghadri JR, Wittstein IS, Prasad A, Sharkey S, Dote K, Akashi YJ, Cammann VL, et al. International Expert Consensus Document on Takotsubo Syndrome (Part I): Clinical Characteristics, Diagnostic Criteria, and Pathophysiology. Eur Heart J. 2018;39(22):2032-2046.
doi pubmed - Buchmann SJ, Lehmann D, Stevens CE. Takotsubo Cardiomyopathy-Acute Cardiac Dysfunction Associated With Neurological and Psychiatric Disorders. Front Neurol. 2019;10:917.
doi pubmed - Templin C, Hanggi J, Klein C, Topka MS, Hiestand T, Levinson RA, Jurisic S, et al. Altered limbic and autonomic processing supports brain-heart axis in Takotsubo syndrome. Eur Heart J. 2019;40(15):1183-1187.
doi pubmed - Finsterer J, Stollberger C. Transient global amnesia: The cerebral Takotsubo? J Neurol Sci. 2017;376:196-197.
doi pubmed - Aimo A, Pelliccia F, Panichella G, Vergaro G, Barison A, Passino C, Emdin M, et al. Indications of beta-adrenoceptor blockers in Takotsubo syndrome and theoretical reasons to prefer agents with vasodilating activity. Int J Cardiol. 2021;333:45-50.
doi pubmed - Bader Abu Ghalyoun, et al. Abstract 11626: faster recovery in Takotsubo with prior beta-blocker use. Circulation. 2019;140:A11626.
- Sattar Y, Siew KSW, Connerney M, Ullah W, Alraies MC. Management of Takotsubo Syndrome: A Comprehensive Review. Cureus. 2020;12(1):e6556.
doi - El-Battrawy I, Ansari U, Lang S, Behnes M, Schramm K, Fastner C, Zhou X, et al. Impact and management of left ventricular function on the prognosis of Takotsubo syndrome. Eur J Clin Invest. 2017;47(7):477-485.
doi pubmed - El-Battrawy I, Lang S, Ansari U, Tulumen E, Schramm K, Fastner C, Zhou X, et al. Prevalence of malignant arrhythmia and sudden cardiac death in takotsubo syndrome and its management. Europace. 2018;20(5):843-850.
doi pubmed - Yayehd K, N'Da N W, Belle L, Bataille V, Hanssen M, Leddet P, Aupetit JF, et al. Management of Takotsubo cardiomyopathy in non-academic hospitals in France: The Observational French SyndromEs of TakoTsubo (OFSETT) study. Arch Cardiovasc Dis. 2016;109(1):4-12.
doi pubmed - El-Battrawy I, Zhao Z, Lan H, Schunemann JD, Sattler K, Buljubasic F, Patocskai B, et al. Estradiol protection against toxic effects of catecholamine on electrical properties in human-induced pluripotent stem cell derived cardiomyocytes. Int J Cardiol. 2018;254:195-202.
doi pubmed - Kumar S, Kaushik S, Nautiyal A, Choudhary SK, Kayastha BL, Mostow N, Lazar JM. Cardiac rupture in takotsubo cardiomyopathy: a systematic review. Clin Cardiol. 2011;34(11):672-676.
doi pubmed - Medina de Chazal H, Del Buono MG, Keyser-Marcus L, Ma L, Moeller FG, Berrocal D, Abbate A. Stress cardiomyopathy diagnosis and treatment: JACC State-of-the-Art review. J Am Coll Cardiol. 2018;72(16):1955-1971.
doi pubmed - Silverio A, et al. Drug treatment with beta-blockers and long-term outcome in patients with takotsubo syndrome: results from the takotsubo Italian network. European Heart Journal. 2019;40:21.
doi - Santoro F, Ieva R, Musaico F, Ferraretti A, Triggiani G, Tarantino N, Di Biase M, et al. Lack of efficacy of drug therapy in preventing takotsubo cardiomyopathy recurrence: a meta-analysis. Clin Cardiol. 2014;37(7):434-439.
doi pubmed - Santoro F, Ieva R, Ferraretti A, Fanelli M, Musaico F, Tarantino N, Martino LD, et al. Hemodynamic effects, safety, and feasibility of intravenous esmolol infusion during Takotsubo cardiomyopathy with left ventricular outflow tract obstruction: results from a multicenter registry. Cardiovasc Ther. 2016;34(3):161-166.
doi pubmed - Singh K, Carson K, Usmani Z, Sawhney G, Shah R, Horowitz J. Systematic review and meta-analysis of incidence and correlates of recurrence of takotsubo cardiomyopathy. Int J Cardiol. 2014;174(3):696-701.
doi pubmed - Fazio G, Pizzuto C, Barbaro G, Sutera L, Incalcaterra E, Evola G, Azzarelli S, et al. Chronic pharmacological treatment in takotsubo cardiomyopathy. Int J Cardiol. 2008;127(1):121-123.
doi pubmed - Abanador-Kamper N, Kamper L, Wolfertz J, Pomjanski W, Wolf-Putz A, Seyfarth M. Evaluation of therapy management and outcome in Takotsubo syndrome. BMC Cardiovasc Disord. 2017;17(1):225.
doi pubmed - Templin C, Ghadri JR, Diekmann J, Napp LC, Bataiosu DR, Jaguszewski M, Cammann VL, et al. Clinical features and outcomes of Takotsubo (Stress) cardiomyopathy. N Engl J Med. 2015;373(10):929-938.
doi pubmed - Kim H, Senecal C, Lewis B, Prasad A, Rajiv G, Lerman LO, Lerman A. Natural history and predictors of mortality of patients with Takotsubo syndrome. Int J Cardiol. 2018;267:22-27.
doi pubmed - Isogai T, Matsui H, Tanaka H, Fushimi K, Yasunaga H. Early beta-blocker use and in-hospital mortality in patients with Takotsubo cardiomyopathy. Heart. 2016;102(13):1029-1035.
doi pubmed - Santoro F, Mallardi A, Leopizzi A, Vitale E, Rawish E, Stiermaier T, Eitel I, et al. Current knowledge and future challenges in Takotsubo syndrome: part 2-treatment and prognosis. J Clin Med. 2021;10(3):468.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cardiology Research is published by Elmer Press Inc.


