| Cardiology Research, ISSN 1923-2829 print, 1923-2837 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, Cardiol Res and Elmer Press Inc |
| Journal website https://www.cardiologyres.org |
Original Article
Volume 12, Number 3, June 2021, pages 177-185
The Difference in Accuracy Between Global Registry of Acute Coronary Events Score and Thrombolysis in Myocardial Infarction Score in Predicting In-Hospital Mortality of Acute ST-Elevation Myocardial Infarction Patients
Januar Wibawa Marthaa, b, Teddy Arnold Sihitea, Desty Listinaa
aDepartment of Cardiology and Vascular Medicine, Faculty of Medicine, Universitas Padjadjaran, Hasan Sadikin General Hospital, Bandung, Indonesia
bCorresponding Author: Januar W. Martha, Department of Cardiology and Vascular Medicine, Fakultas Kedokteran, Universitas Padjadjaran, Dr. Hasan Sadikin General Hospital, Jl. Pasteur No. 38, Bandung 40161, Indonesia
Manuscript submitted February 28, 2021, accepted March 19, 2021, published online May 14, 2021
Short title: Accuracy of GRACE and TIMI Scores
doi: https://doi.org/10.14740/cr1247
| Abstract | ▴Top |
Background: In-hospital mortality of ST-elevation myocardial infarction (STEMI) patients varies between 1% and 19% in Asia. Global Registry of Acute Coronary Events (GRACE) score and Thrombolysis in Myocardial Infarction (TIMI) score are the most frequently used risk scores for predicting in-hospital mortality. These two scores have different accuracy depending on the risk profiles of each region. This study aimed to identify the difference in accuracy between GRACE and TIMI scores.
Methods: This was an observational cohort retrospective study on consecutive patients with STEMI admitted to Dr. Hasan Sadikin General Hospital Bandung between July 2018 and June 2019.
Results: The risk scores were evaluated in 255 patients with STEMI, whose data were collected from medical records. Patients in this study were 58 ± 11 years old, more often male (78.8%) and have smoking (65.5%), dyslipidemia (61%), hypertension (56.5%) and diabetes mellitus (21.6 %) as their risk factors. Forty-five patients died in hospitalization (17%). The TIMI and GRACE scores revealed a significant graded increase in mortality with a rising score. There was a statistically significant difference in accuracy between the scores of 0.082 (95% confidence interval (CI): 0.040 - 0.125; P < 0.001) with the GRACE score (C statistics of 0.91; P < 0.001) having better accuracy compared to TIMI score (C statistics of 0.83; P < 0.001). This might be due to the fact that the GRACE scoring system has more detail and complete variables than the TIMI score.
Conclusion: There is a significant difference between the accuracy of GRACE and TIMI scores in predicting in-hospital mortality in STEMI patients. The accuracy of the GRACE score is better than the TIMI score for predicting in-hospital mortality in STEMI patients.
Keywords: GRACE; In-hospital mortality; STEMI; TIMI
| Introduction | ▴Top |
Cardiovascular disease (CVD) is the primary cause of death around the world, with 17.9 million deaths or approximately 31% of the total global annual deaths. Of these, 85% are due to strokes and acute coronary syndrome (ACS), which underlines the fact that coronary artery disease (CAD) is still a challenging global health problem until now [1].
The variations in clinical features and risks across the ACS spectrum make the assessment of mortality risk important for the selection of both service level and management strategy [2, 3]. Patients with ST-elevation myocardial infarction (STEMI) may have a higher or lower risk; however, all of them require reperfusion therapy regardless of the risk stratification result. In contrast, patients with non-ST segment elevation acute cardiac syndrome (NSTEACS) totally rely on risk stratification for the decision whether revascularization is needed or not. Nevertheless, with the high risk of death among STEMI patients, the European Society of Cardiology (ESC) guideline still recommends risk stratification of STEMI for predicting the short- and long-term prognoses [4, 5].
Several validated risk scoring systems have been proposed to predict in-hospital mortality in ACS such as Global Registry of Acute Coronary Events (GRACE) score and Thrombolysis in Myocardial Infarction (TIMI) score [4, 6]. The mortality rate due to STEMI in Asia varies considerably between 1% to more than 19% and the accuracy of the GRACE score and the TIMI score on mortality also varies in this region [7-12]. Other factors beyond GRACE and TIMI score variables, including geographic variations in the risk profile, may influence mortality during treatment in Asia [13].
This study was expected to identify the difference in accuracy between the GRACE score and TIMI score in predicting in-hospital mortality of STEMI in Dr. Hasan Sadikin General Hospital Bandung, a tertiary hospital in Indonesia.
| Materials and Methods | ▴Top |
This was an observational study with a retrospective cohort. Data were collected consecutively from the medical records of patients diagnosed with STEMI or with the ICD code of I21.0-I21.3 from July 2018 to June 2019 and included patient’s history, physical examination, laboratory results, electrocardiogram (ECG) record, TIMI score, GRACE score and reperfusion time. There were 255 of 341 patients with a medical record code of I21.0-I21.3 who met the inclusion criteria. Patients with I21.0-I21.3 code but with a diagnosis other than STEMI, such as NSTEACS and occlusion myocardial infarction (OMI), and those with incomplete or absent medical records, were excluded. The study has been approved by Hospital Ethics Committee.
The sample size was estimated using the Henley test with a β of 90% (α of 5%) and a ratio of 1:10 for the patient death outcome. The statistical models used were: 1) Baseline characteristics in numerical variables presented as mean ± standard deviation when normally distributed and median with range when abnormally distributed, and characteristics in categorical variables presented in numbers and percentages; 2) Distribution based on the level of GRACE and TIMI risks; 3) Evaluation of the discrimination performance of GRACE and TIMI scores using the receiver operator characteristic (ROC) plot; and 4) Comparison of the area under the curve (AUC) parameters for GRACE and TIMI scores using the Fisher’s z-test. Results were considered statistically significant when the P-value is ≤ 0.05. Data were recorded in a specific form and processed using the SPSS version 24.0 for Windows.
| Results | ▴Top |
There were 255 STEMI patients who met the inclusion criteria in our study. The mean age of the subjects was 58 ± 11 years with 78.8% of them being male. The most common traditional risk factors in the study subjects were smoking (65.5%), dyslipidemia (61%), hypertension (56.5%), diabetes mellitus (21.6%) and menopause (12.5%). The onset from symptoms to diagnosis (first medical contact) was 3 h (0 - 240 h) with the transfer time to the hospital of 6 h (0 - 142 h). Hence, the onset from symptoms to arrival at the hospital was 10 h (0.5 - 336 h) and the time to treatment was 9.5 h (0.1 - 216 h). Of all patients, 26.3% received pharmacological reperfusion and 39.6% received percutaneous coronary intervention (PCI), while 34.1% did not receive reperfusion. The median door to needle time was 60 min (6 - 541 min) and the median door to device time was 563 min (13 - 12,960 min). Almost all patients received antiplatelet therapy, statin and anticoagulant. Fifty-eight percent of patients received angiotensin-converting enzyme inhibitors (ACEis) and 55.3% received beta-blockers. There were 45 patients who died in hospitalization (case fatality rate (CFR) of 17%) caused by cardiogenic shock (44%), malignant arrhythmia (22%), respiratory failure (9%), septic shock (9%), stroke (7%), hemorrhagic shock (4%) and ventricular septal rupture (2%). The median length of stay for STEMI patients was 4 days (0 - 19 days) (Table 1).
 Click to view | Table 1. Patients Baseline Characteristics |
The results of the variable analysis of the GRACE score showed significant differences in age, heart rate, systolic blood pressure, Killip class and history of cardiac arrest at admission between those who died and those who survived (P < 0.05), while the results of the variable analysis of TIMI score showed significant differences in heart rate, systolic blood pressure and Killip class between those who died and those who survived (P < 0.05). Most patients who died were above 65 years old with a heart rate of < 60 or > 100 beats per minute and a systolic blood pressure of < 90 or > 180 mm Hg. These patients had Killip III or IV with a history of cardiac arrest at admission. Other variables such as troponin, creatinine, ST-segment deviation, myocardial infarction wall, body weight, risk factors (diabetes mellitus, hypertension and angina) and time to treatment of > 4 h were not different between survived and died patients (Table 2).
 Click to view | Table 2. Baseline Characteristics of GRACE and TIMI Variables |
The GRACE scores were normally distributed, but the TIMI scores were asymmetrically distributed. The mean GRACE score was 124 ± 36 and the median TIMI score was 4 (1 - 12). The GRACE score and TIMI score were higher in patients who died than in those who survived (P < 0.001). The total proportions of low, medium, high-risk patients in the GRACE score were 59.8%, 20.8% and 19.6%, respectively, while the same proportions for the TIMI scores were 42.8%, 39.2% and 18%, respectively. There were 75.6% of patients at high risk and 8.9% of patients with a low risk based on the GRACE score who died during hospitalization, whereas there were 60% of patients at high risk and 11.1% of patients with a low risk based on the TIMI score who died during hospitalization.
The AUC value of the GRACE score from the ROC curve was 0.917 and the AUC value of the TIMI score was 0.83. The comparison of the AUC score between the two scores demonstrated that the GRACE score had a larger AUC area than the TIMI score (Table 3 and Fig. 1).
 Click to view | Table 3. Comparison of Accuracy GRACE and TIMI Scores |
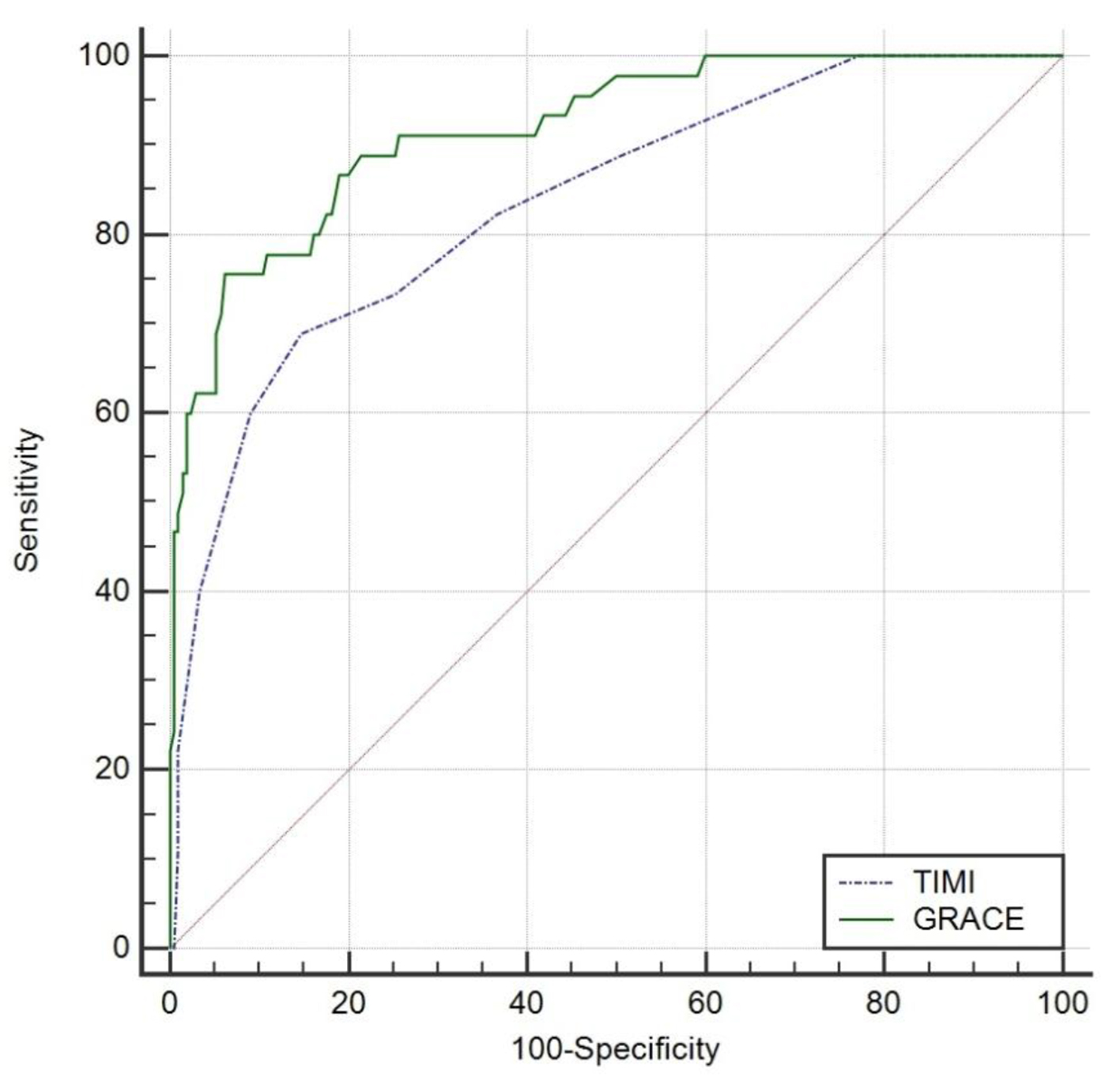 Click for large image | Figure 1. AUC of GRACE and TIMI scores in one plot ROC. GRACE: Global Registry of Acute Coronary Events; TIMI: Thrombolysis in Myocardial Infarction; AUC: area under the curve; ROC: receiver operator characteristic. |
When the AUC parameters of the GRACE score and TIMI score were compared, a statistically significant difference was seen (P < 0.001). Both scores presented a high accuracy value of 0.91 and 0.83, respectively (P < 0.001). The GRACE score had a higher accuracy compared to the TIMI score with a difference of 0.082 (95% confidence interval (CI): 0.040 - 0.125), which was statistically significant (P < 0.001).
| Discussion | ▴Top |
The total number of STEMI patients investigated in our study is 255 with a total death of 45 (17%). A previous study by Chen et al investigated 404 patients with STEMI with a total of 27 deaths (6.7%), while Correia et al’s study involved 152 STEMI patients with a total death of 16 (11%) [9, 14]. The original large-scale GRACE study included 3,419 patients with a 6% mortality rate [15]. Another large-scale study, the InTIME II, involved a total of 14,114 STEMI patients who underwent fibrinolytic therapy with a mortality rate of 6.7% within 30 days. This is validated by the NRMI 3 study that shows a mortality rate of 12.6% from a total of 84,029 patients [16]. The baseline characteristics of our study demonstrated that the mean age of STEMI patients is 58 ± 11 years, which is younger than in studies by Chen et al (median, 68 years (55 - 75 years)) and Correia et al (average, 63 ± 13 years) as well as in the GRACE study (median, 66.3 years (56 - 75 years)) and the InTIME II study (median, 62 years (52 - 70 years)) [9, 14, 15, 17]. Male gender predominates in our study (78.9%) as also seen in studies by Chen et al (88.9%) and Correia et al (72%) as well as in the GRACE study (66.5%), and InTIME II study (76.3%) [9, 14, 15, 17]. The most common traditional risk factors identified are smoking (65.5%), dyslipidemia (61%), hypertension (56.5%), diabetes mellitus (21.6%) and menopause (12.5%) with smoking and dyslipidemia as the dominant risk factors. The composition of these risk factors is slightly different from those of Correia et al with hypertension being the most dominant risk factor but similar to that of the InTIME II study which identified smoking as the highest risk factor [9, 14, 18]. The difference in the composition of these risk factors may be caused by differences in population related to the geographic factors of each study.
Patients aged > 65 years have a different mortality outcome when compared to patients aged under 65 years in our study. Elderly patients tend to experience more complications and hemodynamic disturbances. Most patients are in the Killip I class (72.7%), followed by Killip II (12.1%), Killip IV (11.7%) and Killip III (3.5%) classes. The mortality rates of patients with Killip III class (13% versus 1.4%; P < 0.001) or IV (39.1% versus 5.7%; P < 0.001) are higher. The percentage of patients with Killip IV class is higher (11.7%) than in several other studies but almost similar with the study by Chen et al. Patients with Killip IV class have been shown to have a poor prognosis, which may be one of the causes of the high mortality of STEMI patients in our study.
The number of patients who experienced cardiac arrest in admission (14.5%) and later died is higher than those without cardiac arrest in admission (67.4% versus 2.9%; P < 0.001). Most patients (88%) with a history of cardiac arrest are admitted to our hospital < 48 h of onset and 84% of these patients died. No previous study mentioned history of cardiac arrest [9, 14]. The original GRACE study mentioned cardiac arrest in 1.5% and patients with prior cardiac arrest are a high-risk population [15]. The in-hospital mortality rate of ACS patients with a history of cardiac arrest is higher than that in those without cardiac arrest (40.4% versus 4.2%) and remains higher up to 1 year after the event (51.9% versus 12.1%; P < 0.001) [19-21].
This study demonstrates that the most affected myocardial wall is the anterior wall (50.2%), followed by the inferior wall (47.8%), lateral wall (1.8%) and others (0.8%). There are no significant differences in terms of the affected myocardial wall, troponin values, time to treatment of > 4 h and creatinine values between those who died during hospitalization and those who survived.
There is a significant difference in in-hospital mortality outcome in patients with a heart rate of < 60 or > 100 beats per minute (P < 0.001) in this study. The heart rate of < 60 beats per minute in this study is due to atrioventricular block and the heart rate of > 100 beats per minute is due to ischemia, impaired patient hemodynamics, or increased sympathetic activities.
There is also a significant difference in the in-hospital mortality outcome between patients with systolic blood pressure of < 90 mm Hg and > 180 mm Hg (P < 0.001). A systolic blood pressure of < 90 mm Hg can be associated with cardiogenic shock complications and a systolic blood pressure of > 180 mm Hg is associated with malignant hypertension which increases the coronary artery oxygen demand and occurrence of pulmonary edema [22]. The median systolic blood pressure in our study was 120 mm Hg (60 - 209 mm Hg), which is lower than in other studies (Chen et al, 123 mm Hg (104 - 147 mm Hg); inTIME II study, 140 mm Hg (122 - 155 mm Hg); GRACE study, 140 mm Hg (120 - 160 mm Hg); and Correia et al study, 150 ± 31 mm Hg) [9, 14, 15, 17]. This may be related to hypertension which was not a dominant risk factor in our population.
This study compares the accuracy of the GRACE score and the TIMI score in predicting mortality in STEMI patients. The GRACE score classifies the probability for in-hospital mortality as low when the score is < 125 (< 2% risk of death), moderate when the score is 126 - 154 (2-5% risk of death) and high when the score is > 155 (> 5% risk of death). Meanwhile, the TIMI score classifies the probability for in-hospital mortality as low when the score is 0 - 3 (0.8-4.4%), moderate when the score is 4 - 7 (7.3-23.4%) and high when the score is > 8 (26.8-35.9%) [3, 18]. The GRACE score for high risk of > 155 has a sensitivity and specificity of 75.5% and 92.3%, respectively, in predicting mortality outcomes while the TIMI score for high risk of > 8 has a sensitivity and specificity of 40% and 96.67%, respectively. The accuracies of the GRACE score and the TIMI score are described in the AUC statistic of 0.91 (P < 0.001) and 0.83 (P < 0.001). Both scores have high accuracy. The difference between the GRACE score and the TIMI score is statistically significant (P < 0.001) with the GRACE score having more variables associated with in-treatment mortality and more details in each variable. The accuracy of GRACE and TIMI scores in Correia et al’s study is similar (AUC, 0.87 vs. 0.87; P = 0.71), maybe because both scores have the same dominant variables, such as age, systolic blood pressure, Killip class, risk factors (hypertension, diabetes mellitus and angina), reperfusion time of > 4 h and creatinine value. Nonetheless, the C statistical value of the GRACE score (0.766; 0.720 - 0.808) is better than the TIMI score (0.738; 0.690 - 0.782) in Chen et al’s study (P = 0.028) because of the dominant creatinine value. The original GRACE study has a fairly good accuracy value, with an AUC of 0.77 in European and American STEMI populations, as well as in a number of Asian countries. Meanwhile, the InTIME II study has an AUC value of 0.784 in the STEMI population that underwent fibrinolytic therapy in Europe and the USA [3, 15]. The AUC value of this study is higher than in the original GRACE and InTIME II studies. This can be due to the risk profile of the STEMI population at our hospital that fits better with the GRACE and TIMI scoring risk models.
The median score of this study is TIMI 4, which is a moderate risk associated with a probability of death of 7.3%. Meanwhile, the mean GRACE score is 124 ± 36, showing a mild risk with a probability of death < 2%. The distribution of the GRACE score is quite balanced with the proportion of values based on the low, moderate and high risk categories, i.e., 73.9%, 15.2% and 10.9%, respectively, while the TIMI score is asymmetrically distributed with a proportion of 58.7%, 28.3% and 13%, respectively. The proportion of low, moderate and high risk for death in the GRACE score is 8.9%, 15.5% and 75.6%, while the TIMI score has the proportion distribution of 11.1%, 28.9% and 60%. A previous study demonstrated a distribution of low, moderate and high risk for mortality in GRACE scores of 2.4%, 25% and 73% and 0%, 4.9% and 25% in TIMI score with an optimum threshold value of > 170 (81% sensitivity and 88% specificity) for GRACE score and > 5 (75% sensitivity and 86% specificity) for TIMI score [14].
There are five GRACE score variables in this study that are different between patients who died and survived, i.e., age, history of cardiac arrest at admission, systolic blood pressure, heart rate and Killip class. The ST-segment deviation variables, creatinine and troponin values are not different between the two groups. Meanwhile, there are four TIMI score variables in this study, namely age, systolic blood pressure, heart rate and Killip class, which are different between patients who died and survived. The variables of time to treatment of > 4 h, body weight, increased troponin value, anterior wall and having one of the risk factors for hypertension, diabetes, or angina are not significantly different.
Age, systolic blood pressure, heart rate and Killip class are variables that are included in both scores and affect mortality. Another variable that is worth to be considered is the high incidence of cardiac arrest on admission. The GRACE score is a score obtained from a large observational study in which the inclusion criteria are ACS patients (STEMI and NSTEACS) with various characteristics of patients who underwent reperfusion and those who do not get reperfusion. This makes the GRACE score have a higher ability to reflect the general ACS population. The TIMI score comes from a selected study of STEMI patients who underwent fibrinolytic therapy and has been validated in the NRMI 3 study in the general patient population with the TIMI score being less accurate in patients who do not undergo reperfusion (C statistic 0.65) compared to those who do (C statistics 0.79) [3, 15].
Studies that become the basis of the TIMI scoring system do not involve the population in Asian countries while the GRACE score only involves a small region in Asia. The accuracy value of the GRACE score and the TIMI score is a component of the validation of the GRACE score and TIMI score stratification in various parts of the world. Hence, this study is expected to contribute information on the GRACE score and TIMI score validation in Asia and also globally.
The high mortality rate in this study might also relate to the delay factor. Compared to other studies such as studies by Correia et al (CFR 11%), Chen et al (CFR 6.7%) and Dharma et al (CFR 6%), the mortality rate in our study is quite high. The onset from the occurrence of symptoms to diagnosis (first medical contact) is 3 h (0 - 240 h) and the transfer time is 6 h (0 - 142 h). Furthermore, the time from the occurrence of symptoms until the patient arrived at hospital is 10 h (0.5 - 336 h) and the onset to treatment was 9.5 h (0.1 - 216 h). The door to device time in our study is 563 min (13 - 12,960 min), which is longer than in a study by Dharma et al in Jakarta, Indonesia, of 102 ± 68 min and in a study by Correia et al of 132 min or 2.2 h (95 - 175 min) [23]. Most patients (73%) who came to our hospital and underwent PCI are late presenters (> 12 h from onset). Only 15.7% of patients received reperfusion in ≤ 4 h. The proportion of patients who underwent reperfusion in our study is higher than in Dharma et al’s study (65.6% versus 54%), albeit with a longer door to device time [24]. More patients (89%) underwent reperfusion in Luis et al’s study with PCI (77%) and thrombolytic (11%) therapies while 60.9% patients in Chen et al’s study underwent reperfusion with PCI (50.7%) and coronary artery bypass grafting (CABG) (10.2%). The proportion of patients who underwent pharmacological reperfusion, PCI and those who do not undergo reperfusion are 26.3%, 39.2% and 34.1%, respectively. The proportion of in-hospital mortality in patients who underwent pharmacological reperfusion, PCI and no reperfusion in this study were 4.4%, 15% and 29%, respectively, which are higher than in Dharma et al’s study of 3.8%, 3.2% and 9.1%, respectively [23]. The mortality outcome is lower in patients who underwent reperfusion either with fibrinolytic therapy (8.7% versus 30.5%; P < 0.001) or PCI (39.4% versus 40.5%; P < 0.001).
Almost all patients received antiplatelet (95.4%), anticoagulant (95.7%) and statin (94.5%). Half of the patients received ACEi (58%) or beta-blocker (55.3%). Irawati et al mentioned that adherence to preventive drugs such as ASA, clopidogrel, anticoagulants and statins during treatment in non-reperfused STEMI patients can reduce mortality but the reasons for not receiving these drugs were not explained [24]. Patients with mortality outcome tend to be less likely to receive dual antiplatelet therapy, ACEi, beta-blockers and statins, whereas the provision of anticoagulants are not different in this study. Patients who died tend to experience hemodynamic disorders such as shock, renal failure, atrioventricular block and heart failure; thus, the use of beta-blockers and ACEi is lower. Statin use is lower in patients who died because these patients died < 24 h before they were given statin or they had complications such as renal failure and hemodynamic disturbances.
The GRACE study emphasizes the importance of risk stratification for making an informed decision regarding referral to tertiary care centers, level of care, time of treatment, pharmacological therapy and intervention of choice. Patients with a high risk for death will benefit most from reperfusion and the benefits outweigh the risks associated with therapies such as fibrinolytic therapy [15]. Patient’s risk characteristics play a role in the choice of therapy in STEMI, including the presence of cardiogenic shock and left bundle branch block (LBBB). In addition, financial constraints may create the need for triage and diversion of resources, as well as referrals to the tertiary service center [3]. Patients with low risk can be discharged early and patients with high risk while hemodynamically unstable should cautiously use beta-blockers and receive complete revascularization [14]. The GRACE score and TIMI score in Asian STEMI patients have moderate to good accuracy in predicting in-hospital mortality with the GRACE score having superior accuracy than the TIMI score [9].
The TIMI score is more practical than the GRACE score because the variables are easier to calculate. However, the GRACE score has more details in each variable, making the result more accurate. The GRACE score also stratifies age, heart rate and Killip class, adding the variable values and the risk of death can be calculated. The accuracy of the GRACE score and the TIMI score will vary depending on the population studied and may change according to the risk characteristics of the population. This study is a single-center study and only assesses the difference in performance. No comparison of calibration performance is made between the GRACE score and the TIMI score.
The strength of this study is that the sample size is large enough to assess the accuracy of the GRACE score and the TIMI score. The retrospective cohort design used is good for assessing the strength of patients’ independent and dependent variables, including the inclusion criteria of the study. Yet, there are patients that have to be excluded from the study due to incomplete data and false diagnosis. Nevertheless, the samples were derived from a single tertiary hospital; therefore the preliminary findings worth further multicenter observation.
Conclusion
There is a difference in the accuracy of the GRACE score and the TIMI score in predicting in-hospital mortality in STEMI patients at Dr. Hasan Sadikin General Hospital Bandung, Indonesia. The accuracy of the GRACE score (AUC 0.91; 0.877 - 0.948) is better than the TIMI score (AUC 0.835; 0.784 - 0.878) with P < 0.001 for predicting in-hospital mortality in STEMI patients in this hospital.
Acknowledgments
The authors wished to thank the Staff of Medical Records Department, Hasan Sadikin Hospital, Bandung, Indonesia for assisting retrieval of medical records and data acquisitions.
Financial Disclosure
None to declare.
Conflict of Interest
None to declare.
Informed Consent
Not applicable.
Author Contributions
Januar W. Martha: investigation, formal analysis, data curation, writing-original draft, writing review and editing, conceptualization, methodology, validation. Teddy A. Sihite: formal analysis, writing review and editing, conceptualization, methodology, validation. Desty Listina: writing review and editing, project administration.
Data Availability
The data supporting the findings of this study are available from the corresponding author upon reasonable request.
| References | ▴Top |
- Cardiovascular disease [Internet]. WHO. 2017. Available from: www.who.int/news-room/fact-sheet/detail/cardiovascular-diseases-cvds.
- Ryan TJ, Antman EM, Brooks NH, Califf RM, Hillis LD, Hiratzka LF, Rapaport E, et al. 1999 update: ACC/AHA guidelines for the management of patients with acute myocardial infarction. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on Management of Acute Myocardial Infarction). J Am Coll Cardiol. 1999;34(3):890-911.
doi - Morrow DA, Antman EM, Charlesworth A, Cairns R, Murphy SA, de Lemos JA, Giugliano RP, et al. TIMI risk score for ST-elevation myocardial infarction: A convenient, bedside, clinical score for risk assessment at presentation: An intravenous nPA for treatment of infarcting myocardium early II trial substudy. Circulation. 2000;102(17):2031-2037.
doi pubmed - Borja Ibanez SJ, Stefan Agewall, Manuel J. Antunes, Chiara Bucciarelli-Ducci, Hector Bueno. Esc guidelines for the management of acute myocardial infarction in patients presenting with st-segment elevation. European Heart Journal. 2017;00:1-66.
- Brogan RA, Malkin CJ, Batin PD, Simms AD, McLenachan JM, Gale CP. Risk stratification for ST segment elevation myocardial infarction in the era of primary percutaneous coronary intervention. World J Cardiol. 2014;6(8):865-873.
doi pubmed - Roffi M, Patrono C, Collet J-P, Mueller C, Valgimigli M, Andreotti F, Bax JJ, et al. 2015 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: Task Force for the Management of Acute Coronary Syndromes in Patients Presenting without Persistent ST-Segment Elevation of the European Society of Cardiology (ESC). Eur Heart J. 2016;37(3):267-315.
doi pubmed - Chan MY, Du X, Eccleston D, Ma C, Mohanan PP, Ogita M, Shyu KG, et al. Acute coronary syndrome in the Asia-Pacific region. Int J Cardiol. 2016;202:861-869.
doi pubmed - Prabhudesai AR, Srilakshmi MA, Santosh MJ, Shetty GG, Varghese K, Patil CB, Iyengar SS. Validation of the GRACE score for prognosis in Indian patients with acute coronary syndromes. Indian Heart J. 2012;64(3):263-269.
doi - Chen YH, Huang SS, Lin SJ. TIMI and GRACE risk scores predict both short-term and long-term outcomes in Chinese patients with acute myocardial infarction. Acta Cardiol Sin. 2018;34(1):4-12.
- Koonsiripaiboon E, Tungsubutra W. Validation of the GRACE risk score to predict in-hospital mortality in patients with ST segment elevation myocardial infarction in Thailand. J Med Assoc Thai. 2013;96(Suppl 2):S139-145.
- Furnaz S, Karim M, Ashraf T, Ali S, Shahid I, Ali S, Khawaja UA, et al. Performance of the TIMI risk score in predicting mortality after primary percutaneous coronary intervention in elderly women: Results from a developing country. PLoS One. 2019;14(7):e0220289.
doi pubmed - Selvarajah S, Fong AY, Selvaraj G, Haniff J, Uiterwaal CS, Bots ML. An Asian validation of the TIMI risk score for ST-segment elevation myocardial infarction. PLoS One. 2012;7(7):e40249.
doi pubmed - Chan MY, Shah BR, Gao F, Sim LL, Chua T, Tan HC, Yeo TC, et al. Recalibration of the global registry of acute coronary events risk score in a multiethnic Asian population. Am Heart J. 2011;162(2):291-299.
doi pubmed - Correia LC, Garcia G, Kalil F, Ferreira F, Carvalhal M, Oliveira R, Silva A, et al. Prognostic value of TIMI score versus GRACE score in ST-segment elevation myocardial infarction. Arq Bras Cardiol. 2014;103(2):98-106.
doi pubmed - Granger CB, Goldberg RJ, Dabbous O, Pieper KS, Eagle KA, Cannon CP, Van De Werf F, et al. Predictors of hospital mortality in the global registry of acute coronary events. Arch Intern Med. 2003;163(19):2345-2353.
doi pubmed - Morrow DA, Antman EM, Parsons L, de Lemos JA, Cannon CP, Giugliano RP, McCabe CH, et al. Application of the TIMI risk score for ST-elevation MI in the National Registry of Myocardial Infarction 3. JAMA. 2001;286(11):1356-1359.
doi pubmed - In, Time- I. I. Investigators. Intravenous NPA for the treatment of infarcting myocardium early; InTIME-II, a double-blind comparison of single-bolus lanoteplase vs accelerated alteplase for the treatment of patients with acute myocardial infarction. Eur Heart J. 2000;21(24):2005-2013.
doi pubmed - GRACE. Grace acs risk score 2.0 2003. Tersedia dari: www.outcomes-umassmed.org/grace.
- McManus DD, Aslam F, Goyal P, Goldberg RJ, Huang W, Gore JM. Incidence, prognosis, and factors associated with cardiac arrest in patients hospitalized with acute coronary syndromes (the Global Registry of Acute Coronary Events Registry). Coron Artery Dis. 2012;23(2):105-112.
doi pubmed - Benito B, Josephson ME. Ventricular tachycardia in coronary artery disease. Rev Esp Cardiol (Engl Ed). 2012;65(10):939-955.
doi pubmed - Salam AM, AlHabib KF, Almahmeed W, Alsheikh-Ali A, Sulaiman K, Amin H, Al-Lawati J, et al. Abstract 11181: Presentation with cardiac arrest in patients with acute coronary syndromes: Insights from the second gulf registry of acute coronary events. Circulation. 2014;130(suppl_2):A11181.
- Zipes DP, Libby P. Braunwald's heart disease: A textbook of cardiovascular medicine, eleventh edition. Philadelphia: Elsevier; 2019.
- Dharma S, Andriantoro H, Purnawan I, Dakota I, Basalamah F, Hartono B, Rasmin R, et al. Characteristics, treatment and in-hospital outcomes of patients with STEMI in a metropolitan area of a developing country: an initial report of the extended Jakarta Acute Coronary Syndrome registry. BMJ Open. 2016;6(8):e012193.
doi pubmed - Irawati S, Dharma S, Taxis K, Nguyen T, Nursyarofah N, Wilffert B, Hak E. Association between adherence to guideline-recommended preventive medications and in-hospital mortality among non-reperfused ST-elevation myocardial infarction patients admitted to a tertiary care academic center in a developing country. Glob Heart. 2020;15(1):8.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cardiology Research is published by Elmer Press Inc.


