| Cardiology Research, ISSN 1923-2829 print, 1923-2837 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, Cardiol Res and Elmer Press Inc |
| Journal website https://www.cardiologyres.org |
Original Article
Volume 12, Number 2, April 2021, pages 80-85
A Retrospective Chart Review of Patients Who Underwent Cardiac Evaluation Before Bariatric Surgery
Maher Nassera, Evelyn Calderonb, d, Miray Kurtcac
aBaylor College of Medicine; Baylor St. Luke’s Medical Center; CHI Health System; Texas Heart Institute; HCA Healthcare; Houston Methodist Hospital, Houston, TX, USA
bFaculty of Medicine, University of Guayaquil, Av. Delta y Av. Kennedy, Guayaquil, Guayas 090112, Ecuador
cFaculty of Medicine, Dokuz Eylul University, Dokuz Eylul Unv. Hst., Inciralti, Balcova/Izmir 35210, Turkey
dCorresponding Author: Evelyn Calderon, Faculty of Medicine, University of Guayaquil, Av. Delta y Av. Kennedy, Guayaquil, Guayas 090112, Ecuador
Manuscript submitted December 23, 2020, accepted January 12, 2021, published online January 24, 2021
Short title: Cardiac Evaluation Before Bariatric Surgery
doi: https://doi.org/10.14740/cr1214
| Abstract | ▴Top |
Background: Overweight and obesity are considered to be a global pandemic. Its associations with hypertension, diabetes and hyperlipidemia are important risk factors for cardiovascular diseases.
Methods: This was a retrospective, observational chart review of obese patients who were seen in our outpatient clinic for cardiovascular clearance prior to an intended bariatric surgery between 2004 and 2020. Data from patient’s demographics, risk factors, presence of coronary artery disease (CAD) and other cardiovascular diseases were collected from medical charts. They underwent clinical evaluation, non-invasive workup including electrocardiograms, echocardiograms, treadmill exercise tests and some of them myocardial perfusion studies and coronary angiograms when indicated, based on their symptoms and/or risk factors for CAD.
Results: From 761 patients studied, 7.6% (58 patients) underwent coronary angiograms, based on their non-invasive workup and their history. Among them, we found that 17 patients had significant CAD. It should be mentioned that this is a selected group of patients with the intention to undergo a bariatric surgical procedure, which this makes them somewhat different from the general population, and this could be considered among the limitations of our study.
Conclusions: Data from our selected population chart review showed that in this specific population, there was no high prevalence of cardiovascular disease, specifically coronary atherosclerosis, dilated cardiomyopathy, left ventricular hypertrophy, heart failure, atrial fibrillation, stroke, venous thrombosis and obstructive sleep apnea.
Keywords: Obesity; Cardiologic evaluation; Bariatric surgery; Chart review
| Introduction | ▴Top |
Obesity is a complicated, chronic health condition that was declared a global pandemic by WHO 20 years ago [1] and the numbers are increasing worldwide at an alarming rate, in both developed and developing countries, and in all age groups [2]. The Obesity Medicine Association defines obesity as a “chronic, relapsing, multifactorial, neurobehavioral disease, wherein an increase in body fat promotes adipose tissue dysfunction and abnormal fat mass physical forces, resulting in adverse metabolic, biomechanical and psychosocial health consequences” [3].
To categorize the overweight, the most common tool used is the WHO classification (Table 1), based on body mass index (BMI) which is calculated using the person’s weight in kilograms divided by the square of his or her height in meters [3].
 Click to view | Table 1. WHO Overweight Classification |
In 2016, 39% of the world’s adult population (more than 1.9 billion adults) were overweight, of whom 13% (over 650 million) had obesity [4]. Some studies predict that prevalence of world’s obese adults would increase from about 13% in 2016 to 51% in 2030 [5]. This rising trend means also that obesity-related comorbidities would increase as well, such as type 2 diabetes, hyperlipidemia, hypertension (HTN), obstructive sleep apnea (OSA), heart disease, stroke, etc. [6]. All have enormous impact on the quality of personal life, and they also contribute to higher healthcare costs and less work productiveness. Also these comorbidities lead up to more than 2.5 million deaths per year worldwide [7]. For this reason, the study of what causes obesity has become more important. Simplifying it, overweight and obesity develop when the amount of calories exceeds the expenditure over a long period of time, creating chronic positive energy balance [8]. The easy access to cheaper high-calorie, low-nutrient food and the increase in sedentary time have increased significantly all around the world and are great contributors to the obesity pandemic [8]. Some studies indicate that other elements could play a major role in susceptibility to obesity such as genetic factors [9], disrupted sleep, variation in appetite, mental stress, viral infections, etc.
Since it is a functional organ, the pathologic adipose tissue enlargement can directly and indirectly contribute to cause detrimental consequences for health. Directly, obesity promotes the expression of proinflammatory cytokines that lead to infiltration of macrophages in the subendotelium, especially in the coronary arteries. Fibrosis and decreased distensibility of heart chambers occur. It also increases stroke volume that over time causes left ventricular (LV) dilation and ends with remodeling and concentric LV hypertrophy with atrial enlargement causing diastolic dysfunction [10].
Obese population have an increased incidence of sleep apnea, HTN, diabetes mellitus, dyslipidemia and thromboembolic disease, which indirectly raises the risk for cardiovascular diseases [10].
| Materials and Methods | ▴Top |
Study design
A retrospective, observational chart review was performed on 761 patients who were seen at our clinic for cardiovascular clearance prior to an intended bariatric surgery between 2004 and 2020. Patients at the clinic were included according to decided inclusion criteria. The Ethics Committee of our outpatient clinic waived the need for ethics approval and the need to obtain consent for the collection, analysis and publication of this retrospect study given the data obtained were anonymized. This study was conducted in compliance with all the applicable institutional ethical guidelines for the care, welfare and use of animals.
Selection of participants
Inclusion criteria were: 1) Patients who were seen for cardiovascular clearance prior to an intended bariatric surgery between 2004 and 2020 with a BMI > 30 kg/m2; 2) Charts with complete information including demographics, height, weight, vital signs, electrocardiograms (ECGs) and echocardiograms. Exclusion criteria were charts with incomplete information.
Data collection
Data were retrospectively collected from medical charts. Information on the following variables was collected: age, gender, weight, height, social history, previous history of HTN, type 2 diabetes mellitus (T2MD), dyslipidemia, congestive heart failure (CHF), history of coronary artery disease (CAD), chronic kidney disease (CKD) and hypothyroidism. Echocardiograms, stress tests and Cath reports were reviewed. In addition, the BMI (weight (kg)/ height (m)2) was calculated and the WHO classification was used to evaluate BMI and types of obesity.
During the analysis of the social history of each patient, smoking status was determined based on the latest definition of the CDC for tobacco use/abuse [11]. For drinking status, we used the drinking levels published by The National Institute on Alcohol Abuse and Alcoholism (NIAAA) [12].
Among our study population, a group of patients underwent coronary angiograms based on their non-invasive workup and/or personal/family history of premature CAD. A positive Cath was defined as the presence of any stenotic lesion in one or more coronary arteries, or the presence of previous percutaneous coronary intervention (PCI).
Statistical methods
The study was descriptive, and no hypothesis testing was performed; therefore, no sample size calculation was made. Given the exclusion criteria, we did not have missing information. All the data were introduced in SPSS [13], and Microsoft Excel program and analyzed meticulously.
The quantitative variables are reported as median ± standard deviation (SD) and min.-max. ranges. The qualitative data were presented as frequency (n) and percentage (%) of prevalence. The population was divided into groups of age (less than 50 years old and more or equal to 50 years old) to assess the net prevalence of CAD in our population.
| Results | ▴Top |
A total of 761 patients were included in this study, of whom 208 (27.3%) were males, and 553 (76.7%) were females. Approximately three-quarters (78.4%) of them were in the morbid obesity category (BMI ≥ 40). The highest BMI found was 85.6.
The mean age was 44.8 ± 10.7 years, with more than half (61.9%) of them between ages 36 and 55. General characteristics of our population like age, BMI, weight, height, past medical history and family history are shown in Table 2. The results are expressed as descriptive statistics as mean ± SD.
 Click to view | Table 2. General Characteristics of the Study Population (n = 761) |
Type of obesity surgical procedure over a period of 16 years started with lap-band, evolved into gastric sleeve and gastric bypass surgery (Fig. 1).
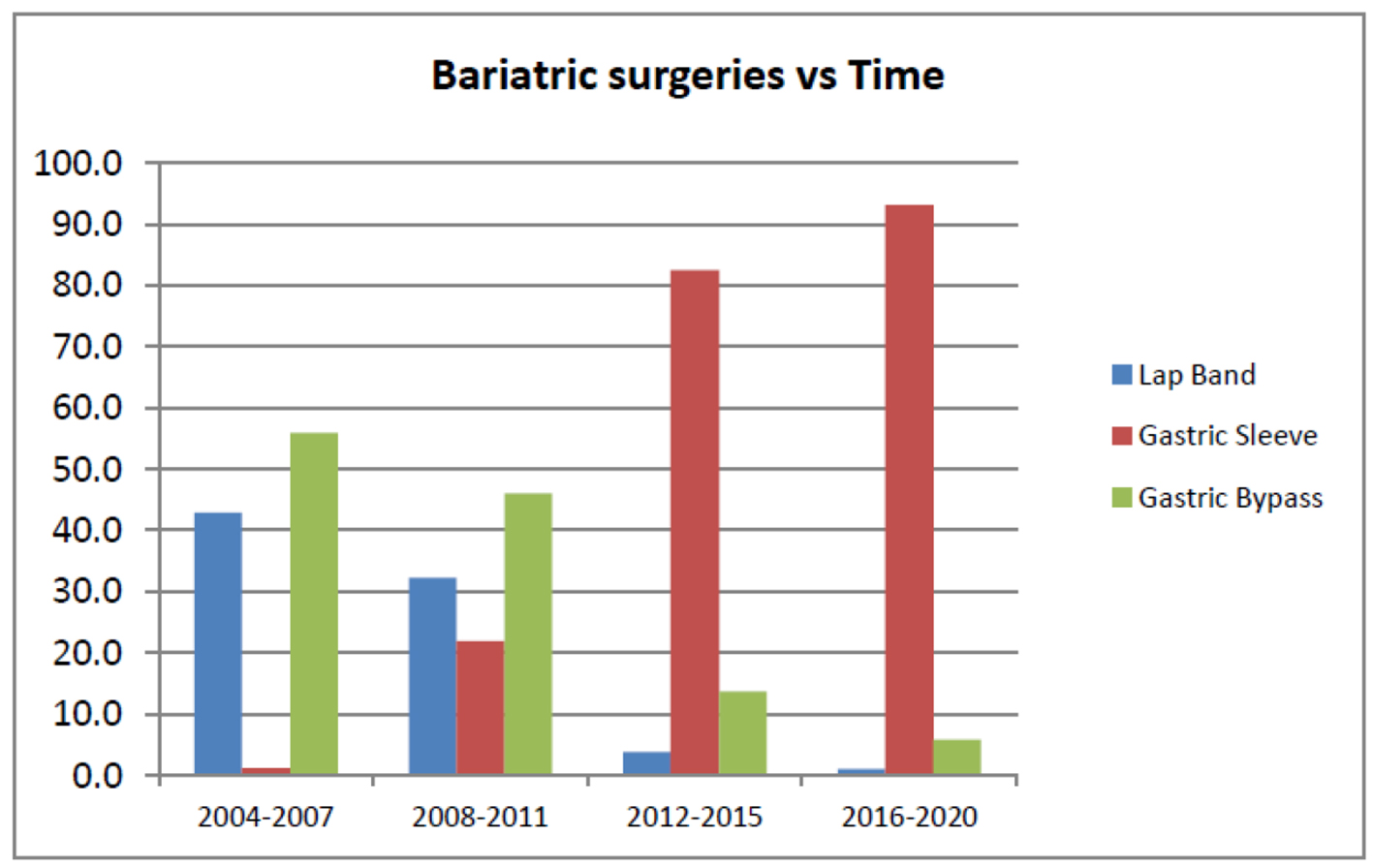 Click for large image | Figure 1. Change in type of bariatric surgery along time. |
Left ventricular ejection fraction (LVEF) by echocardiogram was normal in 95.7% (n = 728) of the total study population.
Left atrial (LA) diameter was measured by 2D echo, and we found that 269 patients (35.3%) had LA diameter > 4 cm. In terms of the variables measured between groups, it was found that there was no significant difference.
Of the patients, 72.9% (n = 585) had normal-mild LV septal wall thickness, 86.8 % (n = 661) had normal-mild LV posterior wall thickness.
We found that treadmill exercise test and myocardial perfusion results in those who were tested were mostly normal in 59.8%.
In 140 patients (18.4%), we were not able to perform the exercise or myocardial perfusion studies due to body habitus limitations.
Of the patients, 38 (5%) showed abnormal myocardial perfusion and required coronary angiograms.
In those with a strong family history of premature CAD, we found 17 of them were positive for variable degrees of CAD. Details of all non-invasive tests are shown in Table 3.
 Click to view | Table 3. Non-Invasive Workup |
Of 761 patients studied, 7.6% (58 patients) underwent coronary angiograms, based on their non-invasive workup and personal/family history of premature CAD. Among those who underwent catheterization, we found that 17 patients had significant CAD (2.23%).
From those 17 patients with CAD, 70.6% (n = 12) were morbidly obese patients, mean age was 57.4 ± 7.7, which revealed that a higher prevalence of cardiovascular risk factors in overweight people is present at older ages.
Of the patients, 76.5% (n = 13) had T2DM, 88.2% (n = 15) had dyslipidemia and 82.4% (n = 14) had HTN.
In the population with CAD, a history of previous tobacco abuse was found in 70.6% (n = 12) of patients and 64.7% (n = 11) reported a strong family history of CAD. Two out of the 17 patients required PCI on further evaluation. A complete description of the population diagnosed with CAD is given in Table 4.
 Click to view | Table 4. Patients With Coronary Angiogram Positive for CAD (n = 17) |
In our selected patient population, the low incidence of CAD may be related to patients’ age (mean age was 44.8). In Table 5, we divided them according to age.
 Click to view | Table 5. CAD Found According to Age Groups |
From 761 patients studied, 46 patients had follow-up cardiac evaluation. We found that 11 patients (30.9%) underwent lap-band surgery, 17 patients (48.7%) had gastric sleeve and 18 patients (53.8%) had gastric bypass surgery. We found that the highest mean weight loss was in patients who underwent gastric bypass surgery.
| Discussion | ▴Top |
The prevalence of morbid obesity is on the rise and epidemiologic studies show Houston among the top 10 cities in the country with a large prevalence of morbidly obese patients.
Over the years and since the research started on CAD risk factors in Framingham (1948), obesity was and has been considered as the sixth important risk factor after hyperlipidemia, diabetes mellitus, HTN, smoking, family history of premature CAD and other minor risk factors.
Obesity is a huge public health problem. It is estimated to affect more than 1 billion people in different continents. Obesity is defined as an excess fat mass (FM) that impairs health. Cardiovascular and metabolic effects are well described over the past 40 years.
Obesity is a risk factor for atherosclerosis and coronary heart disease (CHD). Adipose tissue produces pro-inflammatory cytokines which can induce cardiac dysfunction and the formation of atherosclerotic plaque. Cardiovascular effects include atrial and ventricular enlargement, HTN, atrial fibrillation, dilated cardiomyopathy, CHF, OSA and venous thromboembolism.
The first step in obesity treatment is usually changes in life and eating habits. Unfortunately, diet therapy is comparatively ineffective in treating obesity in the long term [11, 14]. Weight loss surgery is the most effective intervention for weight reduction particularly in patients with BMI ≥ 40, or a BMI ≥ 35 with comorbid conditions. Bariatric surgery is an effective weight-loss intervention for morbidly obese patients, and also a successful treatment for comorbidities such as T2DM and HTN [15]. From the current available types of bariatric surgeries, gastric sleeve is currently the most frequently performed bariatric procedure in the USA [13].
The medical literature has a wealth of research dedicated to obesity. In people with high BMI, it could be related to excess FM or lean mass (LM). The increase in LM may have a protective effect, a phenomenon described as the “obesity paradox” [16].
In our selected patient population, the low incidence of morbid cardiovascular effects may be related to patients’ age: female gender (72.7%) and the above described obesity paradox. Besides this, it was a selected group of patients with the intention to undergo a bariatric surgical procedure which makes them somehow different from the general population, which could be considered among the limitations of our study.
Obesity is consistently associated with an increased risk of metabolic and cardiovascular disease.
CHD is the leading cause of death in men and women in the US population. It increases the risk of fatal heart attacks even in the absence of HTN and DM. The average age of heart attack is 64.5 for men and 70.3 for women.
Conclusion
Although in the general population, obesity and, especially, morbid obesity are associated with a higher risk of CVD and mortality, we found only a small number of patients with CAD, heart failure, stroke and cardiomyopathy in our study population. Female gender (76.7%), age and obesity paradox are the three major factors to explain the low prevalence of cardiovascular disease in our study group.
Acknowledgments
None to declare.
Financial Disclosure
The authors declare that they do not have a financial relationship with any commercial entity that has an interest in the subject of this manuscript.
Conflict of Interest
The authors declare that they do not have a conflict of interest.
Informed Consent
Not applicable.
Author Contributions
Maher Nasser: concieved and design the review, provided the patient’s charts, reviewed the results and writed the discussion of the paper. Evelyn Calderon: collected the data, was involved in the analysis of the information and writing and revising the article prior to submission. Miray Kurtca: collected the data, was involved in the analysis of the information and writing and revising the article prior to submission.
Data Availability
The authors declare that data supporting the findings of this study are available within the article.
| References | ▴Top |
- World Health Organization. Obesity: preventing and managing the global epidemic (World Health Organization Technical Report Series 894). Geneva: WHO, 2000.
- Ng M, Fleming T, Robinson M, Thomson B, Graetz N, Margono C, Mullany EC, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2014;384(9945):766-781.
doi - Hales CM, Fryar CD, Carroll MD, Freedman DS, Ogden CL. Trends in obesity and severe obesity prevalence in us youth and adults by sex and age, 2007-2008 to 2015-2016. JAMA. 2018;319(16):1723-1725.
doi pubmed - World Health Organization. Obesity and overweight [Internet]. 2020 [cited 05 May 2020]. Available from: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight.
- Finkelstein EA, Khavjou OA, Thompson H, Trogdon JG, Pan L, Sherry B, Dietz W. Obesity and severe obesity forecasts through 2030. Am J Prev Med. 2012;42(6):563-570.
doi pubmed - Global Burden of Metabolic Risk Factors for Chronic Diseases C, Lu Y, Hajifathalian K, Ezzati M, Woodward M, Rimm EB, Danaei G. Metabolic mediators of the effects of body-mass index, overweight, and obesity on coronary heart disease and stroke: a pooled analysis of 97 prospective cohorts with 1.8 million participants. Lancet. 2014;383(9921):970-983.
doi - World Health Organization. World Health Report 2002 [Internet]. 2002 [cited May 5, 2020]. Available from: http://www.iotf.org. Accessed January 13, 2004.
- Jackson SE, Llewellyn CH, Smith L. The obesity epidemic - Nature via nurture: A narrative review of high-income countries. SAGE Open Med. 2020;8:2050312120918265.
doi pubmed - Frayling TM, Timpson NJ, Weedon MN, Zeggini E, Freathy RM, Lindgren CM, Perry JR, et al. A common variant in the FTO gene is associated with body mass index and predisposes to childhood and adult obesity. Science. 2007;316(5826):889-894.
doi pubmed - American College of Cardiology. Obesity and cardiovascular disease risk. Cardiology. 2018;47(7):16-19.
- National Center for Health Statistics. Adult tobacco use information. 2017. [cited May 5, 2020]. Available from: https://www.cdc.gov/nchs/nhis/tobacco/tobacco_glossary.htm.
- NIAAA. Drinking levels defined [Internet]. 2020 [cited 05 May 2020]. Available from: https://www.niaaa.nih.gov/alcohol-health/overview-alcohol-consumption/moderate-binge-drinking.
- SPSS I. n.d. IBM SPSS software. [cited May 5, 2020]. Available from: https://www.ibm.com/analytics/spss-statistics-software.
- Apovian CM, Aronne LJ, Bessesen DH, McDonnell ME, Murad MH, Pagotto U, Ryan DH, et al. Pharmacological management of obesity: an endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2015;100(2):342-362.
doi pubmed - North American Association for the Study of Obesity and the National Heart, Lung, and Blood Institute. The practical guide: identification, evaluation, and treatment of overweight and obesity in adults. Bethesda, Md: National Institutes of Health; 2000.
- Vecchie A, Dallegri F, Carbone F, Bonaventura A, Liberale L, Portincasa P, Fruhbeck G, et al. Obesity phenotypes and their paradoxical association with cardiovascular diseases. Eur J Intern Med. 2018;48:6-17.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cardiology Research is published by Elmer Press Inc.


