| Cardiology Research, ISSN 1923-2829 print, 1923-2837 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, Cardiol Res and Elmer Press Inc |
| Journal website http://www.cardiologyres.org |
Case Report
Volume 11, Number 2, April 2020, pages 129-133
Primary Cardiac Undifferentiated High-Grade Intimal Pleomorphic Sarcoma: A Case Series Report
Loba Alama, c, Kavita Agrawala, Vijaya Kankanalaa, Robert Fishbergb, David Powellb
aDepartment of Internal Medicine, Atlantic Health System, Overlook Medical Center, NJ 07901, USA
bDivision of Cardiology, Atlantic Health System, Overlook Medical Center, 99 Beauvoir Ave, Summit, NJ 07901, USA
cCorresponding Author: Loba Alam, Department of Internal Medicine, Atlantic Health System, Overlook Medical Center, 99 Beauvoir Ave, Summit, NJ 07901, USA
Manuscript submitted February 3, 2020, accepted February 15, 2020
Short title: A Case Series Report of PCS
doi: https://doi.org/10.14740/cr1029
| Abstract | ▴Top |
We report two patients with primary cardiac sarcomas. The first patient was admitted for dyspnea on exertion secondary to congestive heart failure. She was later diagnosed with intimal pleomorphic sarcoma involving the right ventricular outflow tract extending into the pulmonary artery, which was further complicated by metastasis to the lung. The second patient was admitted for left-sided weakness secondary to a right frontal lobe ischemic stroke. The patient was later diagnosed with left atrial intimal pleomorphic sarcoma, which was further complicated by metastasis to the small bowel and right femur.
Keywords: Imaging; Cardiac magnetic resonance; Echocardiography; Computed tomography; Thrombus; Cancer
| Introduction | ▴Top |
Primary cardiac sarcomas (PCSs) are extremely rare with only a few cases reported in the literature. About 25% of primary cardiac tumors are malignant, and of those 75% are sarcomas [1]. Radiologic similarities to benign myxomas/thrombus make PCSs a diagnostic challenge. Clinical presentations of PCSs include cerebrovascular accident, pulmonary embolism (PE), valvular dysfunctions, arrhythmias, and congestive heart failure. Imaging modalities such as transthoracic echocardiogram (TTE), transesophageal echocardiogram (TEE), cardiovascular magnetic resonance imaging (CMR), positron emission tomography (PET), and computed tomography (CT) can provide initial information about the tumor location, size and the need for surgery. Chemotherapy and immunotherapy are based on histologic subtype of the tumor. Here we report two cases of undifferentiated PCSs, its diagnostic dilemmas and therapeutic challenges.
| Case Reports | ▴Top |
Case 1
A 79-year-old female with past medical history of hypertension and hyperlipidemia presented with progressively worsening dyspnea on exertion and dry cough for 1 month. Electrocardiogram (ECG) showed normal sinus rhythm and left axis deviation. TTE revealed a large mobile echodensity in the right ventricular outflow tract (RVOT) measuring 6 × 2 cm (Fig. 1a, b). The peak RVOT velocity was elevated at 4.2 m/s, consistent with significant RVOT obstruction. The right ventricle was mildly enlarged and hypokinetic. CT angiogram of the chest showed intraluminal mass in the RVOT extending into the right pulmonary artery, with smaller filling defects in the distal segmental branches (Fig. 2a, b).
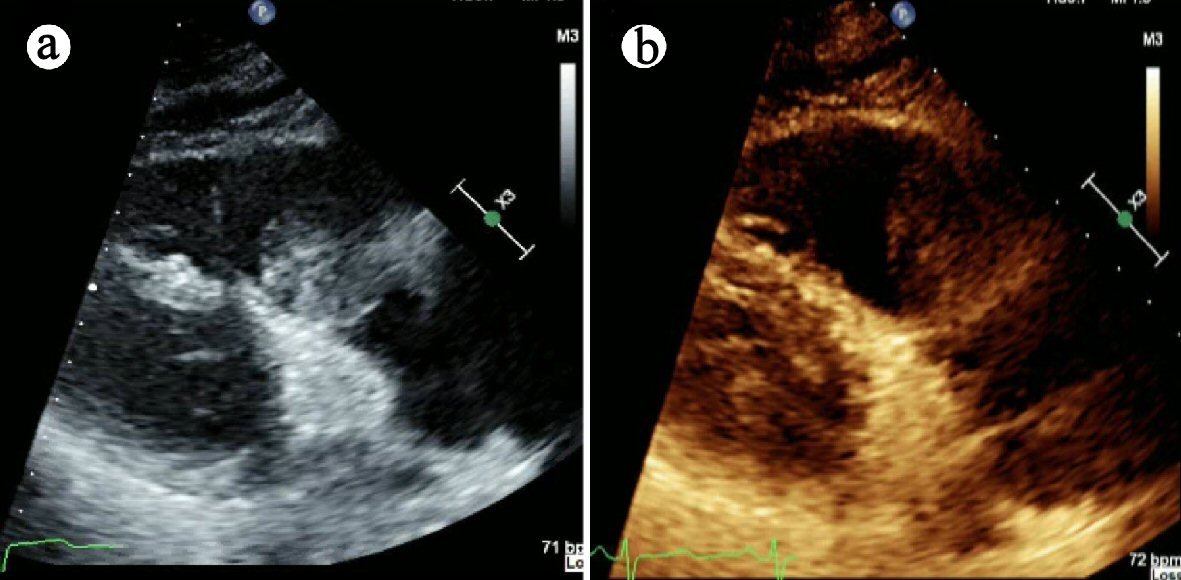 Click for large image | Figure 1. Case 1: TTE demonstrating large mobile, well circumscribed echo-density in the right ventricular outflow tract (RVOT) measuring 6 × 2 cm. TTE: transthoracic echocardiogram. |
 Click for large image | Figure 2. (a) Case 1: CT angiogram demonstrating large intraluminal mass centered in the RVOT. (b) Large eccentric mural thrombus in right main pulmonary artery with smaller filling defects in the distal segmental branches. CT: computed tomography; RVOT: right ventricular outflow tract. |
Differential diagnosis
Based on the clinical scenario, pulmonary thromboembolism was a possibility, and the patient was started on heparin infusion. However, the patient’s dyspnea on exertion could also have been attributed to RVOT obstruction which is rarely reported in the setting of PE. Furthermore, the well circumscribed appearance of the mass on TTE was more characteristic of a tumor. In addition, the right ventricular remodeling with global hypokinesis was consistent with right ventricular pressure overload rather than the characteristic McConnell’s sign seen in PE.
Diagnostic workup/interventions
Further workup included a cardiac magnetic resonance imaging (MRI) which showed an enhancing RVOT mass concerning for sarcoma or other malignancies. PET scan revealed these lesions to be hypermetabolic, increasing suspicion for malignancy. The decision was made for surgical resection of the mass. The patient underwent an incomplete surgical resection of the cardiac mass with positive tumor margins. Pathology confirmed undifferentiated intimal pleomorphic sarcoma with 90% tumor infiltrating immune cells positive for programmed death-ligand 1 (PD-L1). Postoperative complications included cardiogenic shock and acute kidney injury from which patient recovered and underwent physical rehabilitation. She was started on immunotherapy with pembrolizumab to target PD-L1+ tumor cells.
Patient outcome
Although the patient was clinically improving, a 4-month follow-up of chest CT revealed a new solid 12 mm right suprahilar pulmonary nodule concerning for metastatic disease. The decision was made to monitor the patient clinically with continued course of pembrolizumab immunotherapy and interval follow-up imaging. Further advancement in her disease or symptomatology would require consideration for a multidisciplinary treatment approach including surgical resection if appropriate, combined with chemotherapy and/or radiation therapy.
Case 2
A 55-year-old female with past medical history of hypertension presented with left-sided weakness after sustaining a fall. Physical examination revealed decreased motor strength and sensation on the left side. ECG showed new evidence of atrial fibrillation. CT head and MRI head confirmed a right frontal lobe ischemic stroke. Evaluation for the source of embolism included a TTE which demonstrated a 2.1 × 1.2 cm mass attached to the intraatrial septum just adjacent to the anterior mitral annulus (Fig. 3a).
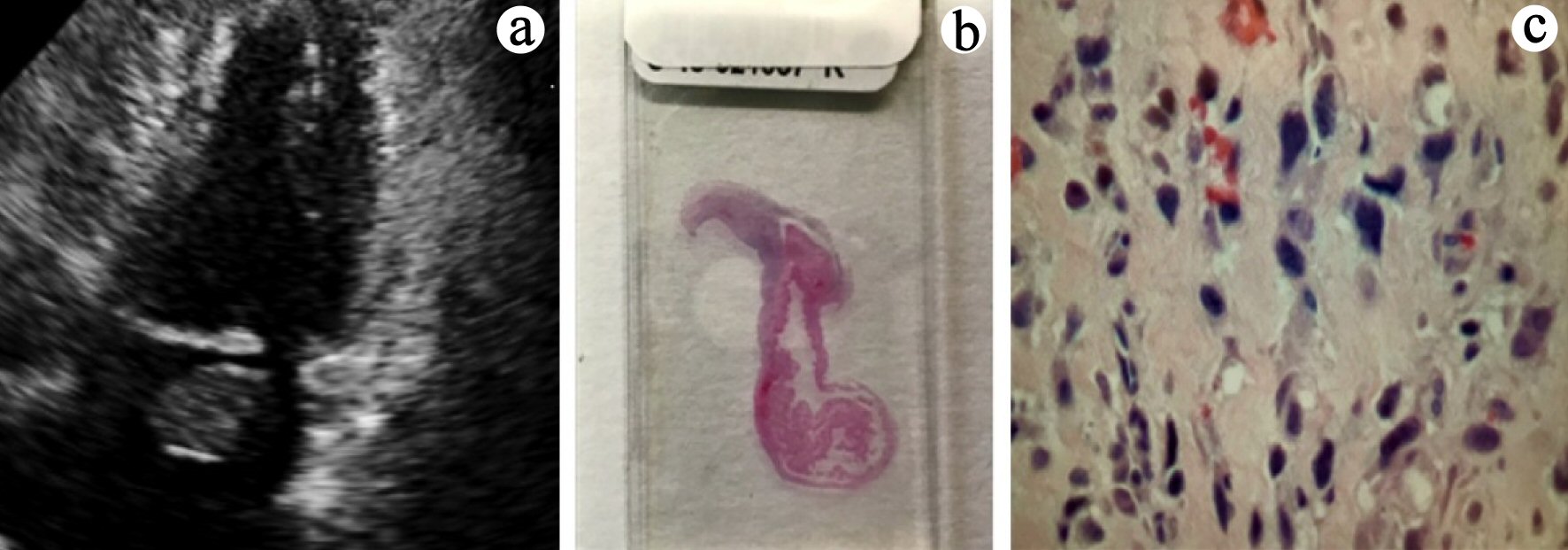 Click for large image | Figure 3. (a) Case 2: TTE demonstrating mass attached to the intraatrial septum adjacent to anterior mitral annulus. (b) Atrial tumor cross section. (c) Pleomorphic, spindle-shaped cells with hyper-chromatic nuclei and prominent mitotic figures. TTE: transthoracic echocardiogram. |
Differential diagnosis
Although the location was atypical, a presumptive diagnosis of left atrial myxoma was made. Myxomas are the most common benign cardiac tumors typically affecting middle aged women. It can occur in either atria but are most commonly attached to the fossa ovalis of the left atrium.
Diagnostic workup/interventions
The decision was made for surgical excision of the mass. The patient underwent resection of the mass with a bovine atrial patch repair. Pathology revealed pleomorphic, spindle-shaped cells with hyperchromatic nuclei and prominent mitotic figures consistent with high-grade intimal pleomorphic sarcoma with positive tumor margins (Fig. 3b, c). Immunophenotyping was positive for murine double minute 2 (MDM2) amplification. The patient underwent local radiotherapy with CyberKnife procedure given the positive tumor margin and no metastatic disease. She was followed-up closely with serial PET/CT and TTE every 3 months.
Patient outcome
Unfortunately, 20 months later the patient presented with small bowel obstruction and pathologic right femur fracture secondary to metastases. Pathology of metastatic lesions were consistent with initial intimal tumor. TEE, CMR and PET/CT revealed recurrence of tumor in the left atrium (Fig. 4a-d). The patient was started on palliative chemotherapy with doxorubicin and olaratumab to target local tumor recurrence and metastasis. Unfortunately, the patient expired 3 years after the initial diagnosis.
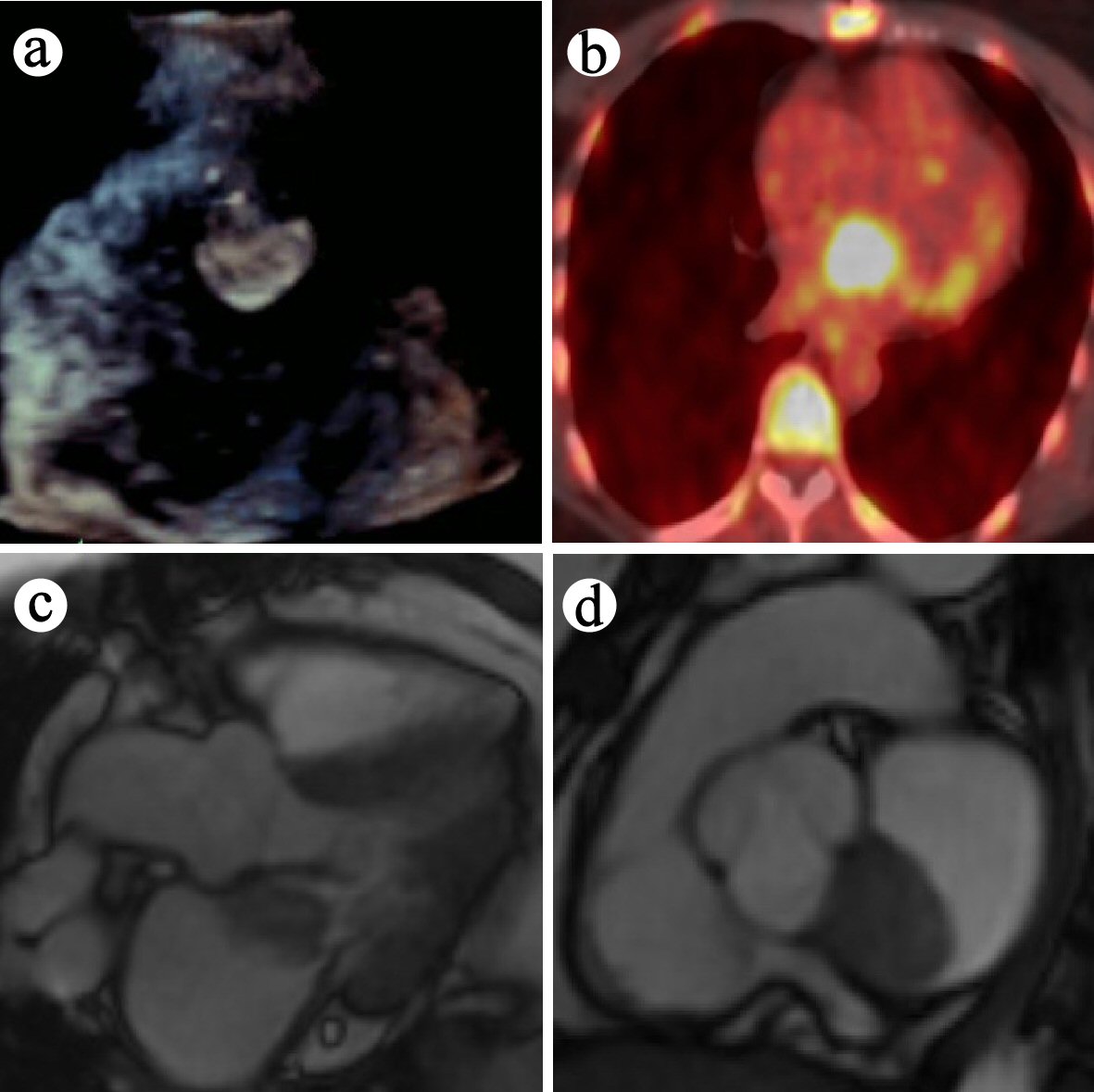 Click for large image | Figure 4. (a) Case 2: TEE demonstrating recurrence of mobile heterogenous echodense mass in left atrium at 20-month interval. (b) Hypermetabolic left atrial lesion on PET/CT. (c) Mass adjacent to anterior mitral leaflet (and prolapses into left ventricle) on CMR. (d) Mass within the left atrium on CMR. TEE: transesophageal echocardiogram; PET/CT: positron emission tomography/computed tomography; CMR: cardiovascular magnetic resonance imaging. |
| Discussion | ▴Top |
Primary cardiac sarcomas are extremely rare neoplasms arising from mesenchymal cells. We present two female patients with undifferentiated intimal pleomorphic sarcoma, previously named malignant fibrous histiocytoma. Intimal pleomorphic sarcomas have a female predominance, with mean presenting age of 47, and involve the posterior wall of the left atrium in > 80% of reported cases [2]. The most common reported symptom of undifferentiated intimal pleomorphic sarcomas includes dyspnea (74%), followed by chest pain and palpitations (40%) [2]. Embolic phenomena have also been reported in organs including brain, lungs, bones, and adrenal glands [2]. Presenting symptoms of primary cardiac sarcomas depend on the location and the size of the tumor rather than the tumor histology. Left heart sarcomas are broad based and abnormally located which differentiates them from myxomas, and commonly present with dyspnea on exertion due to congestive heart failure from obstruction of intracardiac blood flow [3]. Right heart tumors are bulkier and exophytic in nature, commonly presenting with non-specific symptoms [3].
Due to the rareness of primary cardiac sarcomas and consequent lack of randomized controlled trials, no standard treatment protocol has been established. Currently, in addition to surgical resection, two trends are at the frontier of cardiac sarcoma treatment: molecular agents that target genomic alterations and immunotherapy that target immune mediated cancer cells. Based on tumor pathology, our patients demonstrated two different molecular tumor subtypes: case 1 had PD-L1+ tumor cells, and case 2 had MDM2+ amplification. PD-L1 is a key immune checkpoint protein that plays a significant role in sarcomagenesis [4]. Upregulation of PD-L1 is associated with increased tumor aggressiveness [4]. PD-L1+ sarcomas can be targeted with single agent immunotherapy such as pembrolizumab, as seen in our first case.
MDM2 is a proto-oncogene, which is one of the most frequently mutated genes in cardiac intimal sarcomas [5]. Upregulation of MDM2 results in loss of p53-dependent activities, such as apoptosis and cell cycle arrest. There are no established guidelines for chemotherapy targeting MDM2. Newer agent such as olaratumab, a monoclonal antibody that targets platelet-derived growth factor receptor (PDGFR)-α, combined with doxorubicin has limited data to show drug efficacy against soft tissue sarcomas [6].
The overall prognosis of malignant primary cardiac tumors remains poor despite early detection and surgical resection [7]. Patients who receive multimodality treatment with any combination of surgery, chemotherapy, immunotherapy, and radiation have better outcome compared to any single treatment modality alone [8, 9]. Adjuvant treatment needs to be individualized based on the patient’s clinical course and depends on residual disease after initial surgical resection and specific tumor variants.
Learning objectives
There are several learning objectives involved in this study: 1) Left heart sarcomas are broad based and commonly located along the posterior wall of the left atrium, while right heart sarcomas are bulkier and exophytic in nature; 2) Left heart sarcomas commonly present with dyspnea on exertion due to congestive heart failure from obstruction of intracardiac blood flow, and right heart sarcomas commonly present with non-specific symptoms; 3) Multimodality imaging including TTE/TEE, PET, cardiac CT and cardiac MRI can characterize benign versus malignant primary cardiac tumors based on tumor invasion across tissue planes, associated effusions and lymphadenopathy, and visible metastasis; 4) Prompt referral to experienced centers for multidisciplinary approach to surgical resection combined with adjuvant chemotherapy, immunotherapy and radiotherapy can improve outcome; 5) Advancements and better understanding of tumor immunologic and molecular markers can further improve targeted treatment plan in the future.
Conclusions
Non-specific presentations, rarity, and radiologic similarity to benign myxoma or thrombus makes PCSs a diagnostic challenge preoperatively. Advanced imaging modalities (TTE/TEE, CMR, PET/CT) can identify tumors as malignant based on characteristics such as tumor invasion across tissue planes, associated effusions and lymphadenopathy, or visible metastasis. Advanced imaging is further helpful in demonstrating tumor location and staging, anticipating complications, and planning surgical interventions. With promising advancements and better understanding of targeted adjuvant therapies, clinicians may find hope for improved long-term prognosis.
Acknowledgments
We thank Dr. Gregg Rosner from the Division of Cardiology, Columbia University, for his valuable insights on cardiac sarcoma management.
Financial Disclosure
None to declare.
Conflict of Interest
There are no conflicts of interest associated with this manuscript.
Informed Consent
Informed consents were obtained from each patient.
Author Contributions
Loba Alam, Kavita Agrawal, Vijaya Kankanala contributed to conception and design of the study, and acquisition of the data. Robert Fishberg and David Powell were involved in analysis and interpretation of data, and contributed to drafting and revising the article.
Data Availability
The data supporting the findings of this study are available from the corresponding author upon reasonable request.
Abbreviations
PCS: primary cardiac sarcoma; TTE: transthoracic echocardiogram; TEE: transesophageal echocardiogram; CMR: cardiovascular magnetic resonance imaging; CT: computed tomography; PET: positron emission tomography; RVOT: right ventricular outflow tract; PD-L1: programmed death-ligand 1; MDM2: murine double minute 2
| References | ▴Top |
- Hudzik B, Miszalski-Jamka K, Glowacki J, Lekston A, Gierlotka M, Zembala M, Polonski L, et al. Malignant tumors of the heart. Cancer Epidemiol. 2015;39(5):665-672.
doi pubmed - Maleszewski JJ, Bois MC, Bois JP, Young PM, Stulak JM, Klarich KW. Neoplasia and the heart: pathological review of effects with clinical and radiological correlation. J Am Coll Cardiol. 2018;72(2):202-227.
doi pubmed - Simpson L, Kumar SK, Okuno SH, Schaff HV, Porrata LF, Buckner JC, Moynihan TJ. Malignant primary cardiac tumors: review of a single institution experience. Cancer. 2008;112(11):2440-2446.
doi pubmed - Zheng C, You W, Wan P, Jiang X, Chen J, Zheng Y, Li W, et al. Clinicopathological and prognostic significance of PD-L1 expression in sarcoma: A systematic review and meta-analysis. Medicine (Baltimore). 2018;97(25):e11004.
doi pubmed - Oliner JD, Saiki AY, Caenepeel S. The role of MDM2 amplification and overexpression in tumorigenesis. Cold Spring Harb Perspect Med. 2016;6(6):a026336.
doi pubmed - Pender A, Jones RL. Olaratumab: a platelet-derived growth factor receptor-alpha-blocking antibody for the treatment of soft tissue sarcoma. Clin Pharmacol. 2017;9:159-164.
doi pubmed - Elbardissi AW, Dearani JA, Daly RC, Mullany CJ, Orszulak TA, Puga FJ, Schaff HV. Survival after resection of primary cardiac tumors: a 48-year experience. Circulation. 2008;118(14 Suppl):S7-15.
doi pubmed - Ramlawi B, Leja MJ, Abu Saleh WK, Al Jabbari O, Benjamin R, Ravi V, Shapira OM, et al. Surgical treatment of primary cardiac sarcomas: review of a single-institution experience. Ann Thorac Surg. 2016;101(2):698-702.
doi pubmed - Abu Saleh WK, Ramlawi B, Shapira OM, Al Jabbari O, Ravi V, Benjamin R, Durand JB, et al. Improved outcomes with the evolution of a neoadjuvant chemotherapy approach to right heart sarcoma. Ann Thorac Surg. 2017;104(1):90-96.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cardiology Research is published by Elmer Press Inc.


