| Cardiology Research, ISSN 1923-2829 print, 1923-2837 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, Cardiol Res and Elmer Press Inc |
| Journal website http://www.cardiologyres.org |
Case Report
Volume 11, Number 1, February 2020, pages 61-65
Ventricular Tachycardia in an Infant Without Congenital Anomaly: A Case Report
Nouhad El Joueida, d, Marianne Touma Boulosa, Simon Abou Jaoudeb, Linda Daouc
aPediatric Department, Hotel-Dieu de France University Hospital, Saint Joseph University, Medical School, Alfred Naccache Boulevard, Achrafieh, Beirut, Lebanon
bCardiology Department, Hotel-Dieu de France University Hospital, Saint Joseph University, Medical School, Alfred Naccache Boulevard, Achrafieh, Beirut, Lebanon
cPediatric Cardiology Department, Hotel-Dieu de France University Hospital, Saint Joseph University, Medical School, Alfred Naccache Boulevard, Achrafieh, Beirut,Lebanon
dCorresponding Author: Nouhad El Joueid, Pediatric Department, Hotel-Dieu de France University Hospital, Saint Joseph University, Medical School, Alfred Naccache Boulevard, Achrafieh, Beirut, Lebanon
Manuscript submitted December 13, 2019, accepted January 8, 2020
Short title: Sustained VT in 4-Month-Old Infant
doi: https://doi.org/10.14740/cr1005
| Abstract | ▴Top |
Ventricular tachycardia (VT) is a serious form of arrhythmia that can be life-threatening; that’s why diagnosis and treatment are very important in order to avoid serious complications. We are reporting this case of VT which is a rare entity, especially, in healthy infants. This infant, without cardiac pathology known from birth, presented with poor food intake and grunting with hepatomegaly on clinical examination, and a heartbeat at 200/ min. The electrocardiogram (ECG) showed wide QRS complex tachycardia, and the echocardiogram showed a dilated and hypokinetic cardiomyopathy. The clinical signs and chest X-ray changes were consistent with mild cardiac failure. This presentation makes the diagnosis challenging, therefore, it is important to take a good history of the case with a complete clinical exam to achieve the correct diagnosis, and to avoid potential complications. VT of an infant may be benign but should not be diagnosed as such before eliminating serious causes.
Keywords: Infant; Ventricular tachycardia; Normal heart
| Introduction | ▴Top |
Ventricular tachycardia (VT) is uncommon in infant, with an incidence of around 1.1 in 100,000 children [1]. Although very rare, VT is a serious form of arrhythmia; may be life-threatening if degenerated to ventricular fibrillation (VF), and can lead to sudden cardiac arrest [2]. VT can be found in a normal heart or related with congenital heart disease or associated with genetic causes. VT can be present in utero, neonates, infants, children, adolescents and adult population. When VT is present initially in infants, the clinical presentation varies between asymptomatic and seriously ill patient with shock, congestive heart failure and cardiac arrest [3]. Most of VT in infant population occurs in patients with normal heart. The clinical presentation of VT, the rate of VT compared to the underlying sinus rate and the morphology of the tachycardia, are features helping the distinction between benign forms of VT and lethal ventricular arrhythmia. Further testings are often needed to complete this difficult distinction, especially when VT persists [3, 4]. The evaluation of infant VT first begins with a detailed family history, 12-lead electrocardiogram (ECG), echocardiogram, 24-h Holter monitor and magnetic resonance imaging (MRI) if indicated.
VT can be classified into VT associated with heart disease and idiopathic VT [5]. In contrast to adult population, pediatric idiopathic VT is the most common type of VT, with benign long-term outcomes [1, 6-9]. VT onset during infancy is frequently associated with spontaneous resolution of tachycardia [9, 10]. The prognosis of VT in pediatric population is dependent on the underlying etiology of VT, age and treatment method [1, 8]. The mortality rate of VT is higher in cardiomyopathies, long QT syndrome, myocarditis and cardiovascular collapse related to rapid VT due to tumors [3, 11]. Infants have a better prognosis than older children [10]. Treatment recommendations for pediatrics VT vary from conservative observation to antiarrhythmic drugs, invasive surgical procedures or radiofrequency catheter ablation [12-20].
| Case Report | ▴Top |
At 4 months of life, an infant presented to his pediatrician’s clinic for signs of irritability, grunting, increase work of breathing and decreased oral intake for 2 days. The pediatrician notes at physical exam a hepatomegaly and tachycardia at 200 beats per minute. The infant was referred to pediatric cardiologist. The ECG showed wide QRS complex tachycardia at 200 beats per minute that could be corresponding to VT or supraventricular tachycardia with aberrant conduction (Fig. 1). The echocardiogram revealed a global dilatation of left ventricle without hypertrophy and with acceptable systolic function; a dilatation of the right ventricle with altered systolic function; mitral insufficiency grade II and tricuspid insufficiency grade I; pulmonary arterial hypertension (PAH); dilated inferior vena cava and dilated hepatic veins. At this stage two diagnostic hypotheses can be posed: dysrhythmic cardiomyopathy or a cardiac pathology complicated by tachycardia. The clinical signs and chest X-ray changes were consistent also with mild cardiac failure but preserved peripheral perfusion. No electrolyte or metabolic disturbances were found in her blood tests. Upon admission, the patient was given a bolus of adenosine without any change in her tachycardia. Given the sustained VT and the global cardiac failure, the patient was treated by amiodarone 500 mg/m2/day, spironolactone 2 mg/kg/day, furosemide 2 mg/kg/day and captopril 1 mg/kg/day. The tachycardia reverts to sinus rhythm few hours later. ECG after conversion showed normal sinus rhythm at 120/min, with frequent ventricular premature beats (VPBs) having the same morphology of the QRS during tachycardia (Fig. 2). Diagnosis of VT was then confirmed.
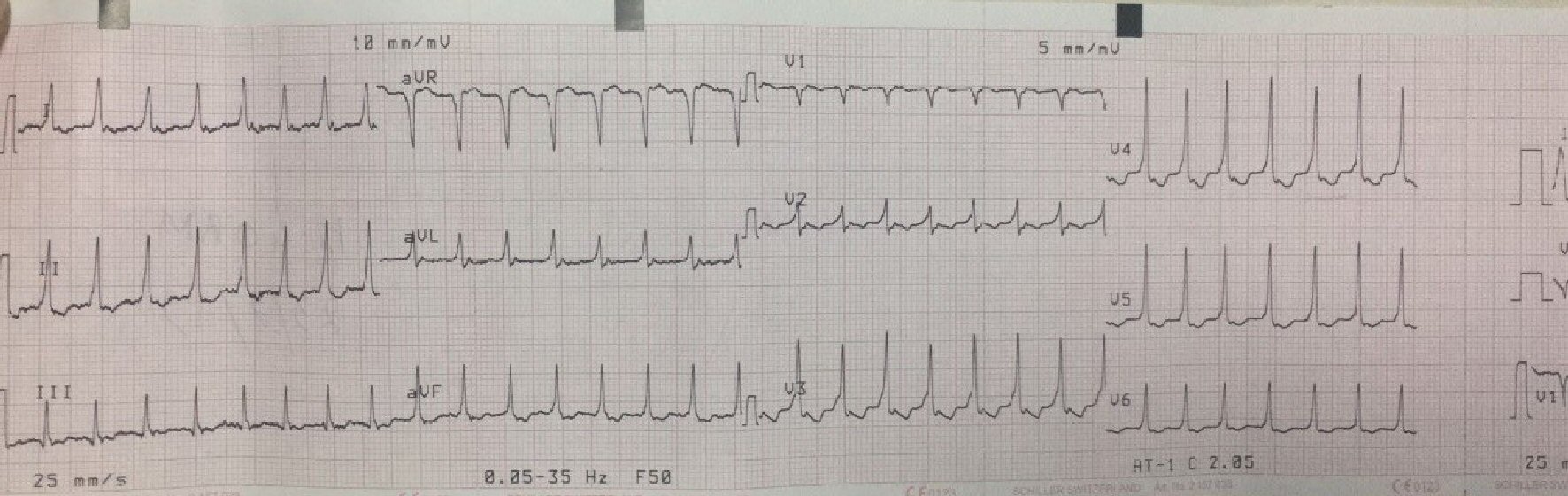 Click for large image | Figure 1. ECG showing wide QRS complex. |
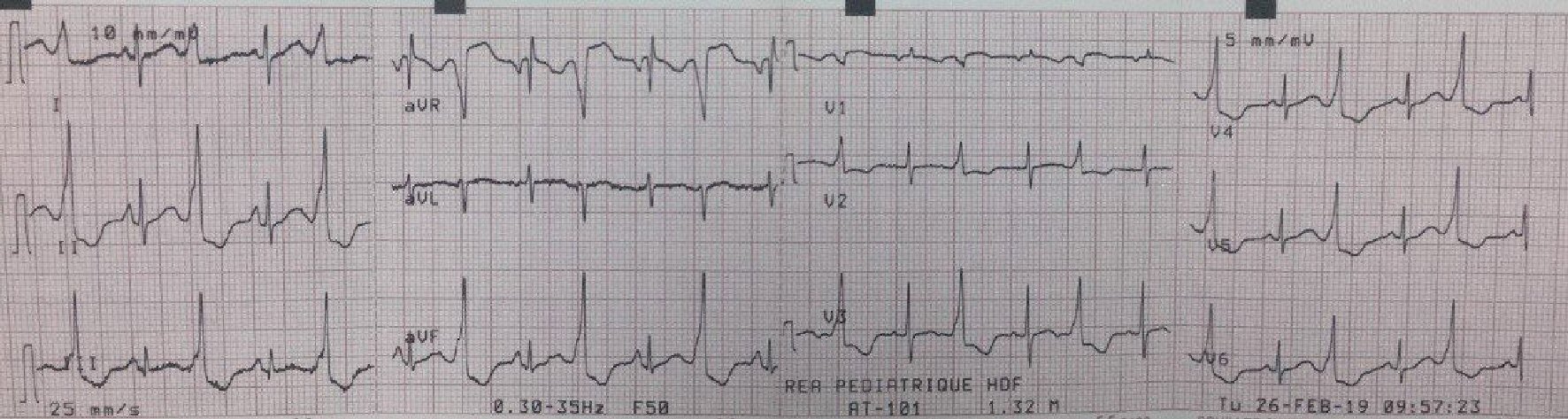 Click for large image | Figure 2. ECG after conversion showing normal sinus rhythm at 120/min, with frequent VPBs, having the same morphology of the QRS during tachycardia. |
Two days later, the echocardiogram shows amelioration in the systolic function of the left ventricle without any dilatation or hypertrophy, amelioration in the systolic function of the right ventricle with less dilatation and without hypertrophy. The 24-h Holter monitor described a sinus rhythm at an average of 129 beats per minute, absence of significant supraventricular hyper excitability, presence of frequent nocturnal and diurnal VPBs in bigeminy and monomorphic. No VT or conductive disorders were noted in the 24-h Holter monitor. After 6 days of monitoring in the hospital, the patient conserved a sinus rhythm without recurrence of the VT. The echocardiogram at day 5 of admission showed a normal function of left and right ventricles without any dilatation, absence of PAH, presence of trivial mitral regurgitation and physiological tricuspid regurgitation. The patient was then discharged on amiodarone 250 mg/m2/day, furosemide 2 mg/kg/day and captopril 1 mg/kg/day. One week after discharge the 24-h Holter monitor was normal. Two months later, the echocardiogram was normal, so furosemide and captopril were stopped, the patient continued amiodarone. Four months later, echocardiogram and the 24-h Holter monitor were also normal (Fig. 3).
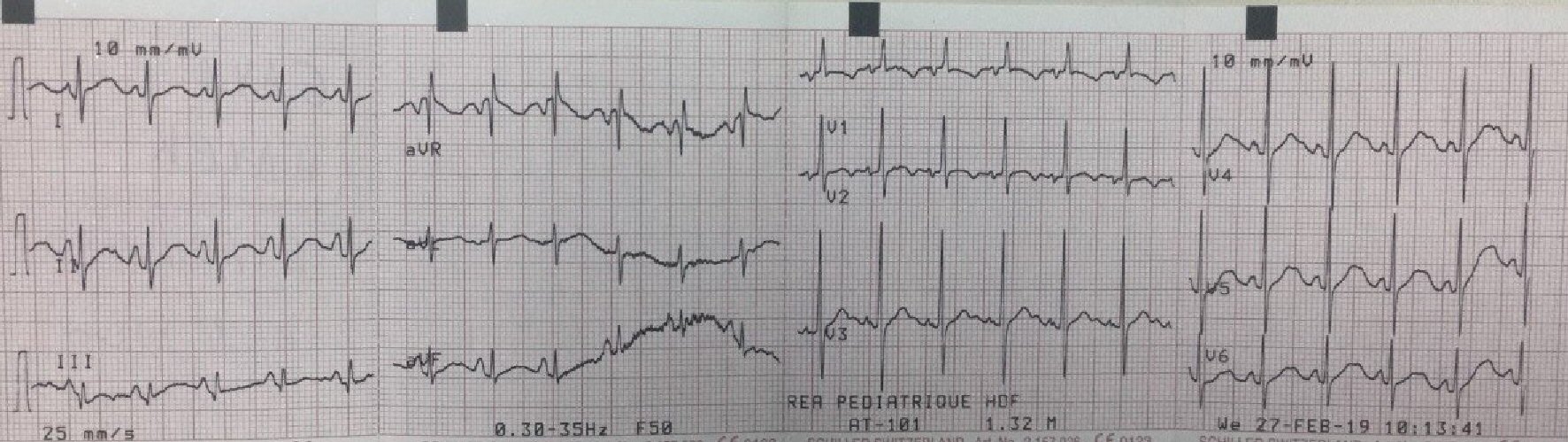 Click for large image | Figure 3. ECG showing normal sinus rhythm at 120/min without VPB. |
| Discussion | ▴Top |
We are reporting this case of VT which is a rare entity in healthy infants [7].VT can be a cause of sudden death in adults and children; that is why diagnosis and treatment are very important in order to avoid serious complications [21]. The etiology of VT in children are electrolyte/metabolic disturbances, myocarditis, long QT syndrome, Brugada syndrome, catecholaminergic polymorphic VT, arrhythmogenic right ventricular cardiomyopathy, dilated and hypertrophic cardiomyopathies, operated congenital heart disease, antiarrhythmic therapy, VT after myocardial infarction and cardiac tumor such as fibroids/myxomas/ teratomas/ lipomas [15, 22]. Another form of VT is idiopathic VT, especially in older children, in the absence of any detectable cause [23, 24]. So VT of an infant may be benign, but should not be diagnosed as such before eliminating serious causes.
This infant, without cardiac pathology known from birth, presented with poor food intake and grunting with hepatomegaly on clinical examination and a heartbeat at 200/min; this presentation of VT is known in the literature in this age group having a normal heart, with general, nonspecific signs related most often to the food intake of the child, and other digestive signs like vomiting and respiratory signs [3].This presentation makes the diagnosis challenging , therefore, it is important to take a good history of the case with a complete clinical exam to achieve the correct diagnosis and to avoid potential complications. The ECG shows a tachycardia at 200/min with wide QRS exceeding 80 ms which corresponds to VT or supraventricular tachycardia with aberrant conduction. Because of the severity of the VT this case of tachycardia with wide QRS should be considered as VT until proven otherwise. Urgent treatment requires an anti-arrhythmic or cardioversion. In the first intention, a test by adenosine is opted without response. So supraventricular tachycardia with aberrant conduction is less likely. Sotalol known for his effectiveness in the pediatric population with fewer side effects [25] is unfortunately not available in Lebanon. That is why amiodarone is then started at a dose of 500 mg/m2 with a gradual improvement of the rhythm, disappearance of the VT on the same day of admission, confirmed by rhythmic Holter showing VPBs after 2 days of admission. Premature ventricular contractions (PVCs) have disappeared with a Holter after 10 days returning normal without disorders of hyperexcitability or conduction disorder.
Concerning the etiological investigation of this case, after stabilization of the infant, the electrolytic problems such as hyperkalemia, hypomagnesemia and hypocalcemia were eliminated. Long genetic QT syndrome is also eliminated by ECG. Also, there is no history of sudden death or syncope [11]. Catecholaminergic polymorphic VT that occurs after stress or physical activity is unlikely in our patient’s age, because the ECG corresponds to sustained monomorphic VT and not to polymorphic VT, furthermore exercise intensity is limited in infants resulting in very rare cases of this type of VT in this age [11, 26]. Regarding primary cardiac tumors that can induce arrhythmias in one third of cases, with the most common being VT [27], the diagnosis can be made by ultrasound, but the final diagnosis is made by cardiac MRI. In this case the MRI has not been done because of the difficulty of a safe simple sedation in this small age.
The dilated and hypokinetic cardiomyopathy seen on admission ultrasound matches the “tachycardia-induced cardiomyopathy”, which is a reversible form of heart failure after arrhythmia [28]. It is sometimes difficult to find if the heart failure is the trigger or the result of arrhythmia. Studies suggest that MRI may be used in litigation cases where the “late gadolinium enhancement” may facilitate the differentiation between the two cases [29]. In our case, VT was present at the same time of the diagnosis of heart failure, with a marked improvement in cardiac function after restoration of a normal rhythm, even stopping treatment with diuretics and angiotensin-converting enzyme inhibitors (ACEIs) after almost 40 days.
Regarding the follow-up of this case, it is important to evaluate the heart rate by rhythmic Holter. The Holter after 10 days returns normal as well as the one done after 5 months. Cardiac MRI will be necessary to evaluate the case of this infant because there was a heart failure at the time of the presentation of the VT, which was therefore symptomatic in our case. It is then suggested to complete in a second time the evaluation by an MRI in order to eliminate an underlying cardiac pathology. In the absence of an obvious cause of the VT shown by this MRI, and a good evolution without recurrence of VT, the most likely diagnosis will be idiopathic VT, which is a benign pathology with good prognosis especially that it occurs before the first 1 year of life [10].
Acknowledgments
None to declare.
Financial Disclosure
No funding to declare.
Informed Consent
Not applicable.
Author Contributions
Nouhad El Joueid provided the conception and design of the study, and contributed to analysis and interpretation of data, drafting the article, and drafting of manuscript. Marianne Touma Boulos supplied the acquisition of data, and contributed to analysis and interpretation of data, and drafting the article. Simon Abou Jaoude involved in the analysis of data, and revised it critically for important intellectual content, and gave final approval of the version to be submitted. Linda Daou supplied the acquisition of data, and involved in the analysis of data; and was responsible for the article critically for important intellectual content, and gave final approval of the version to be submitted.
Data Availability
The authors declare that data supporting the findings of this study are available within the article.
| References | ▴Top |
- Roggen A, Pavlovic M, Pfammatter JP. Frequency of spontaneous ventricular tachycardia in a pediatric population. Am J Cardiol. 2008;101(6):852-854.
doi pubmed - Atkins DL, Everson-Stewart S, Sears GK, Daya M, Osmond MH, Warden CR, Berg RA, et al. Epidemiology and outcomes from out-of-hospital cardiac arrest in children: the Resuscitation Outcomes Consortium Epistry-Cardiac Arrest. Circulation. 2009;119(11):1484-1491.
doi pubmed - Perry JC. Ventricular tachycardia in neonates. Pacing Clin Electrophysiol. 1997;20(8 Pt 2):2061-2064.
doi pubmed - Allen NM, Azam M, Dunne KP, Walsh KP. Idiopathic ventricular tachycardia in a newborn: immediate response to lidocaine. Pediatr Cardiol. 2011;32(5):706-707.
doi pubmed - Crosson JE, Callans DJ, Bradley DJ, Dubin A, Epstein M, Etheridge S, Papez A, et al. PACES/HRS expert consensus statement on the evaluation and management of ventricular arrhythmias in the child with a structurally normal heart. Heart Rhythm. 2014;11(9):e55-78.
doi pubmed - Okumura K, Tsuchiya T. Idiopathic left ventricular tachycardia: clinical features, mechanisms and management. Card Electrophysiol Rev. 2002;6(1-2):61-67.
- Iwamoto M, Niimura I, Shibata T, Yasui K, Takigiku K, Nishizawa T, Akaike T, et al. Long-term course and clinical characteristics of ventricular tachycardia detected in children by school-based heart disease screening. Circ J. 2005;69(3):273-276.
doi pubmed - Song MK, Baek JS, Kwon BS, Kim GB, Bae EJ, Noh CI, Choi JY. Clinical spectrum and prognostic factors of pediatric ventricular tachycardia. Circ J. 2010;74(9):1951-1958.
doi pubmed - Levin MD, Stephens P, Tanel RE, Vetter VL, Rhodes LA. Ventricular tachycardia in infants with structurally normal heart: a benign disorder. Cardiol Young. 2010;20(6):641-647.
doi pubmed - Pfammatter JP, Paul T. Idiopathic ventricular tachycardia in infancy and childhood: a multicenter study on clinical profile and outcome. Working Group on Dysrhythmias and Electrophysiology of the Association for European Pediatric Cardiology. J Am Coll Cardiol. 1999;33(7):2067-2072.
doi - Chiu SN, Wu WL, Lu CW, Tseng WC, Wu KL, Wang JK, Wu MH. Primary ventricular tachycardia in paediatric population in a tertiary centre. Arch Dis Child. 2017;102(12):1137-1142.
doi pubmed - Davis AM, Gow RM, McCrindle BW, Hamilton RM. Clinical spectrum, therapeutic management, and follow-up of ventricular tachycardia in infants and young children. Am Heart J. 1996;131(1):186-191.
doi - Deal BJ, Miller SM, Scagliotti D, Prechel D, Gallastegui JL, Hariman RJ. Ventricular tachycardia in a young population without overt heart disease. Circulation. 1986;73(6):1111-1118.
doi pubmed - Fulton DR, Chung KJ, Tabakin BS, Keane JF. Ventricular tachycardia in children without heart disease. Am J Cardiol. 1985;55(11):1328-1331.
doi - Van Hare GF, Stanger P. Ventricular tachycardia and accelerated ventricular rhythm presenting in the first month of life. Am J Cardiol. 1991;67(1):42-45.
doi - Garson A, Jr., Gillette PC, Titus JL, Hawkins E, Kearney D, Ott D, Cooley DA, et al. Surgical treatment of ventricular tachycardia in infants. N Engl J Med. 1984;310(22):1443-1445.
doi pubmed - O'Connor BK, Case CL, Sokoloski MC, Blair H, Cooper K, Gillette PC. Radiofrequency catheter ablation of right ventricular outflow tachycardia in children and adolescents. J Am Coll Cardiol. 1996;27(4):869-874.
doi - Silka MJ, Kron J. Radiofrequency catheter ablation for idiopathic right ventricular tachycardia: first, last or only therapy - who decides? J Am Coll Cardiol. 1996;27(4):875-876.
doi - Garson A, Jr., Smith RT, Jr., Moak JP, Kearney DL, Hawkins EP, Titus JL, Cooley DA, et al. Incessant ventricular tachycardia in infants: myocardial hamartomas and surgical cure. J Am Coll Cardiol. 1987;10(3):619-626.
doi - Kehr J, Binfield A, Maxwell F, Hornung T, Skinner JR. Fascicular tachycardia in infancy and the use of verapamil: a case series and literature review. Arch Dis Child. 2019;104(8):789-792.
doi pubmed - Bigger JT, Jr., Fleiss JL, Kleiger R, Miller JP, Rolnitzky LM. The relationships among ventricular arrhythmias, left ventricular dysfunction, and mortality in the 2 years after myocardial infarction. Circulation. 1984;69(2):250-258.
doi pubmed - Iwamoto M. Idiopathic ventricular tachycardia in children. Circ J. 2011;75(3):544-545.
doi pubmed - Brooks R, Burgess JH. Idiopathic ventricular tachycardia. A review. Medicine (Baltimore). 1988;67(5):271-294.
doi pubmed - Snyder C, Bishara J, Darling R, Lucas V. Verapamil-sensitive ventricular tachycardia in an infant. Congenit Heart Dis. 2006;1(3):124-126.
doi pubmed - Li X, Zhang Y, Liu H, Jiang H, Ge H, Zhang Y. Efficacy of Intravenous Sotalol for Treatment of Incessant Tachyarrhythmias in Children. Am J Cardiol. 2017;119(9):1366-1370.
doi pubmed - Lee SY, Kim JB, Im E, Yang WI, Joung B, Lee MH, Kim SS. A case of catecholaminergic polymorphic ventricular tachycardia. Yonsei Med J. 2009;50(3):448-451.
doi pubmed - Miyake CY, Del Nido PJ, Alexander ME, Cecchin F, Berul CI, Triedman JK, Geva T, et al. Cardiac tumors and associated arrhythmias in pediatric patients, with observations on surgical therapy for ventricular tachycardia. J Am Coll Cardiol. 2011;58(18):1903-1909.
doi pubmed - Umana E, Solares CA, Alpert MA. Tachycardia-induced cardiomyopathy. Am J Med. 2003;114(1):51-55.
doi - Hasdemir C, Yuksel A, Camli D, Kartal Y, Simsek E, Musayev O, Isayev E, et al. Late gadolinium enhancement CMR in patients with tachycardia-induced cardiomyopathy caused by idiopathic ventricular arrhythmias. Pacing Clin Electrophysiol. 2012;35(4):465-470.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cardiology Research is published by Elmer Press Inc.


