Figures
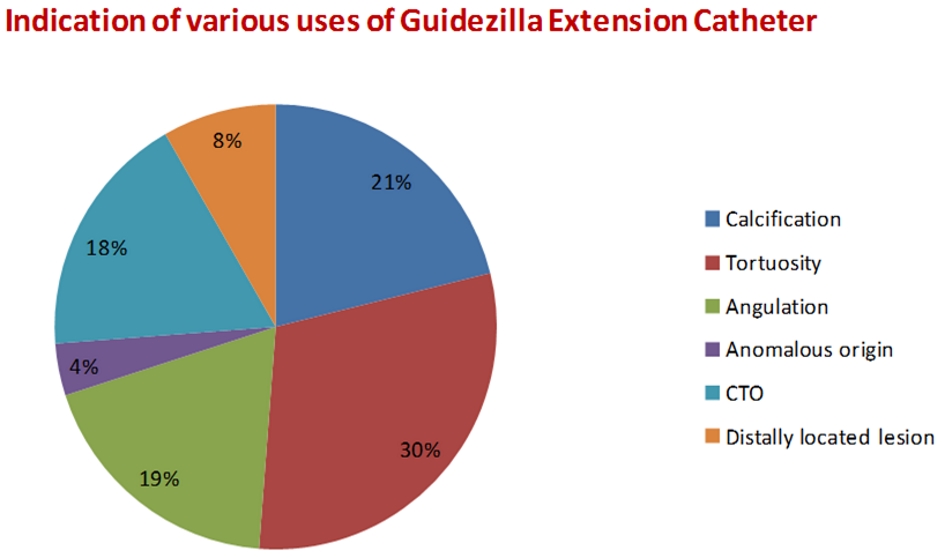
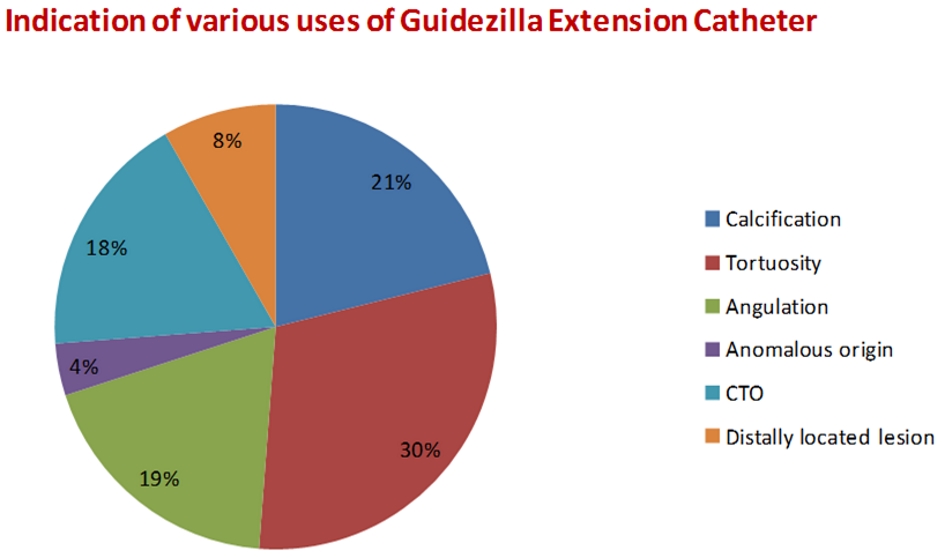
Figure 1. Indications for various uses of Guidezilla extension catheter in PCI. PCI: percutaneous coronary intervention.
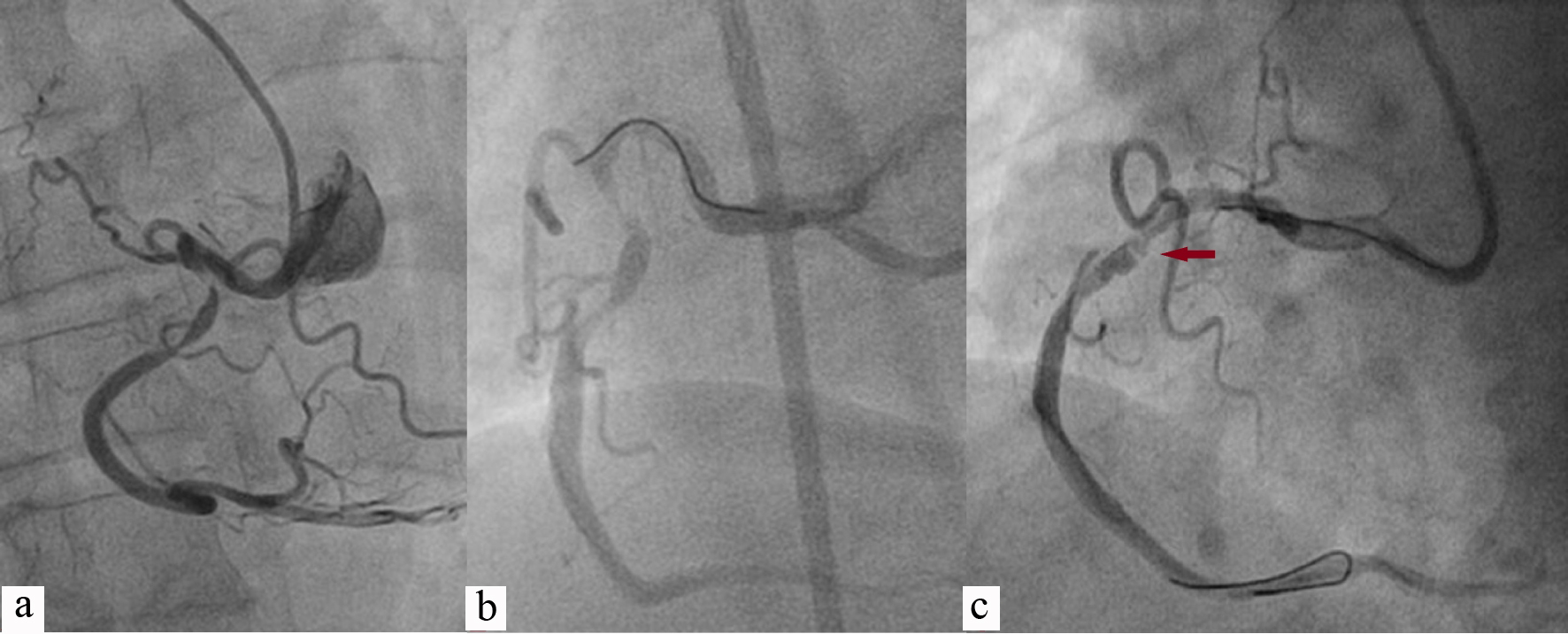
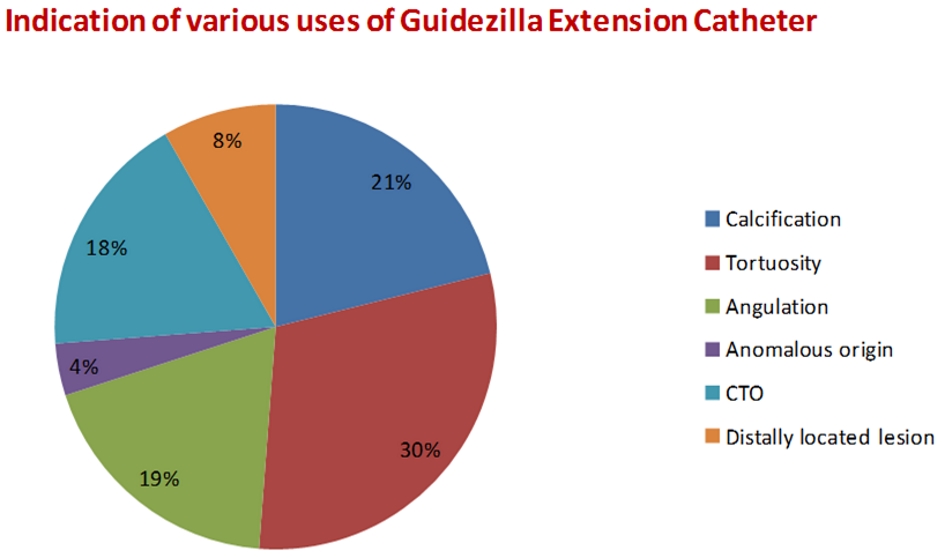
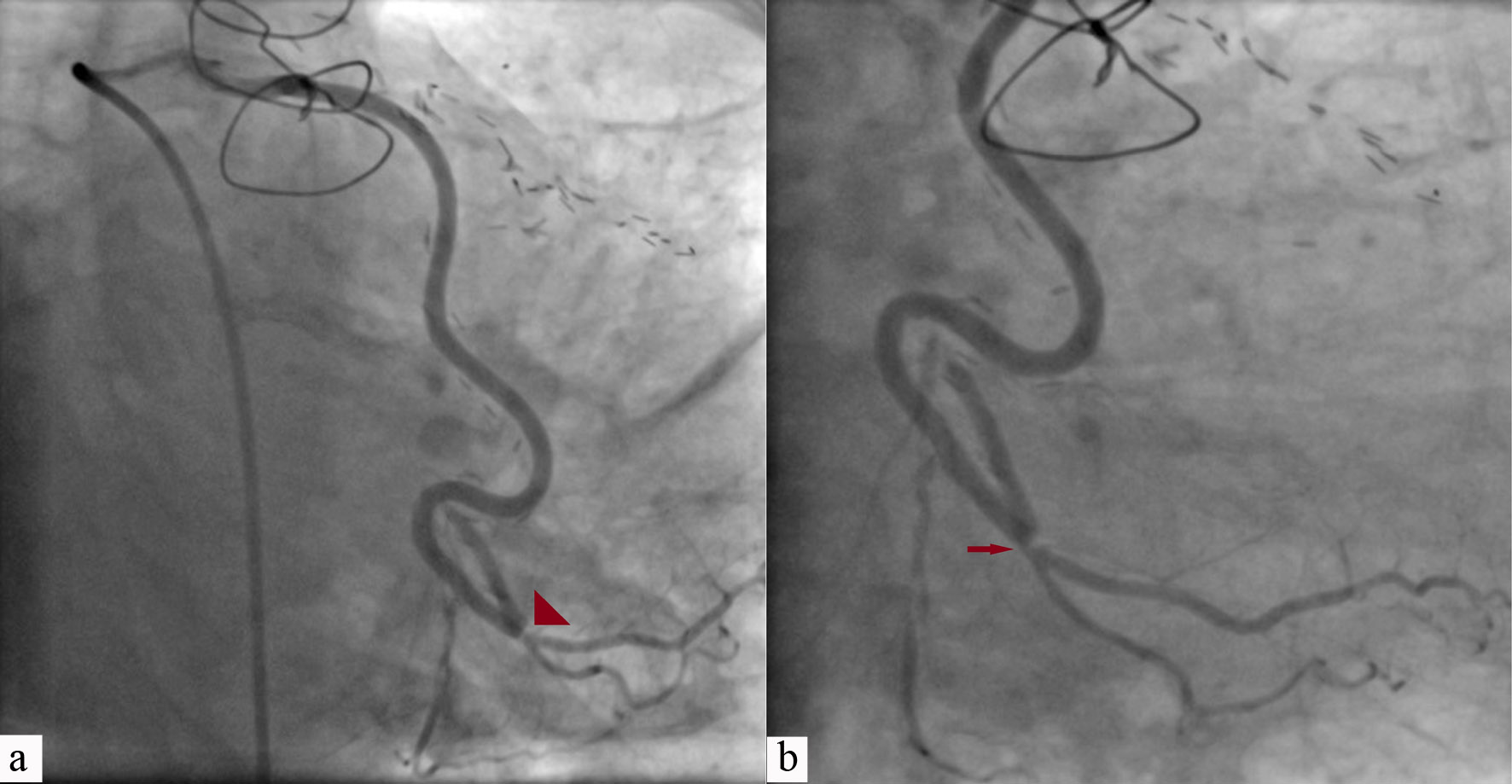
Figure 2. PCI of RCA having acute take-off origin (a); wired with Sion blue (Asahi, Japan) showing concertina effect (horizontal arrow; b, c). PCI: percutaneous coronary intervention; RCA: right coronary artery.
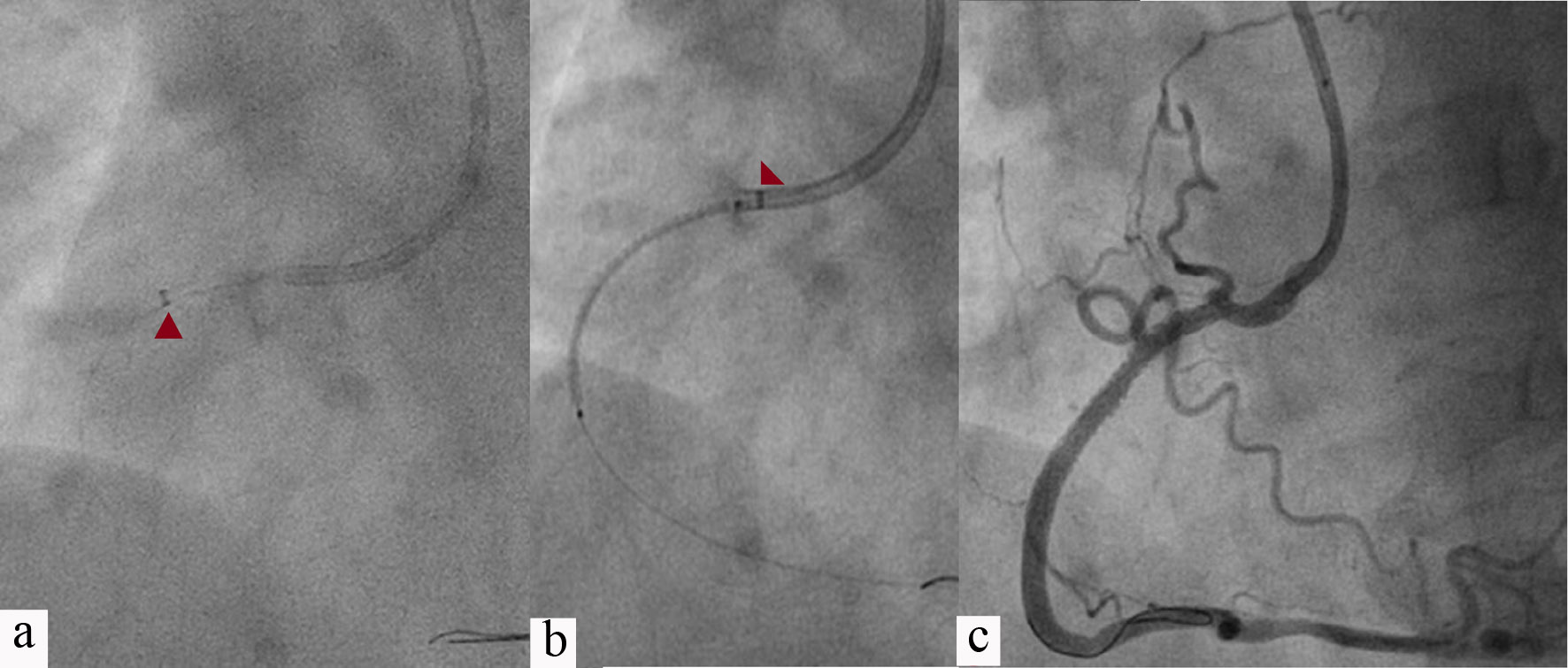
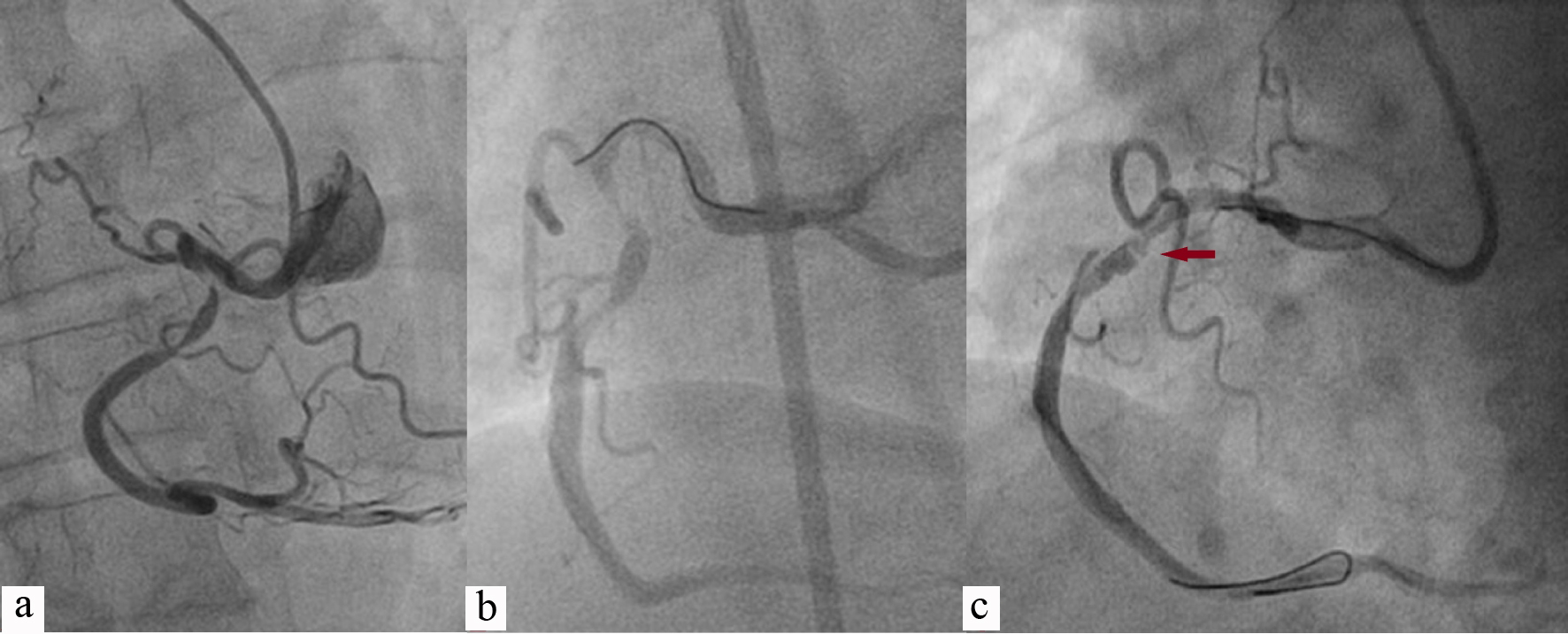
Figure 3. Guidezilla catheter was extended up to mid-RCA (red arrowhead; a); 3.5 × 38 Endeavour Resolute (Zotarolimus-eluting stent, Medtronic, CA, USA) was positioned across the lesion after pulling Guidezilla into guiding catheter (red arrowhead; b); Lesion was stented after deploying stent at 14 atm pressure showing TIMI 3 flow (c). RCA: right coronary artery; atm: atmospheric pressure; TIMI: thrombolysis in myocardial infarction.
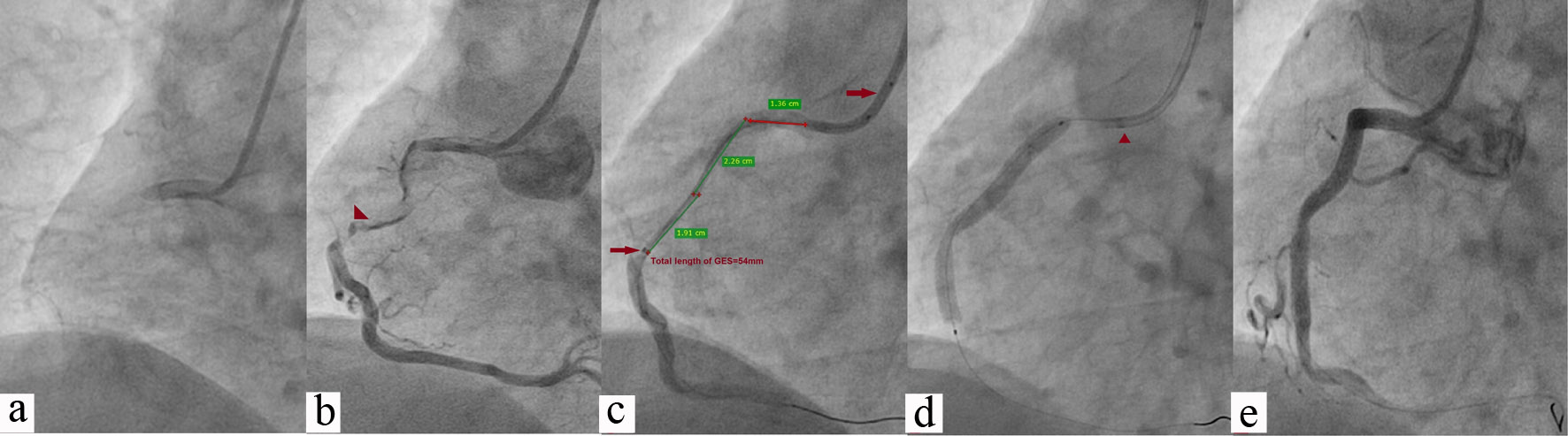
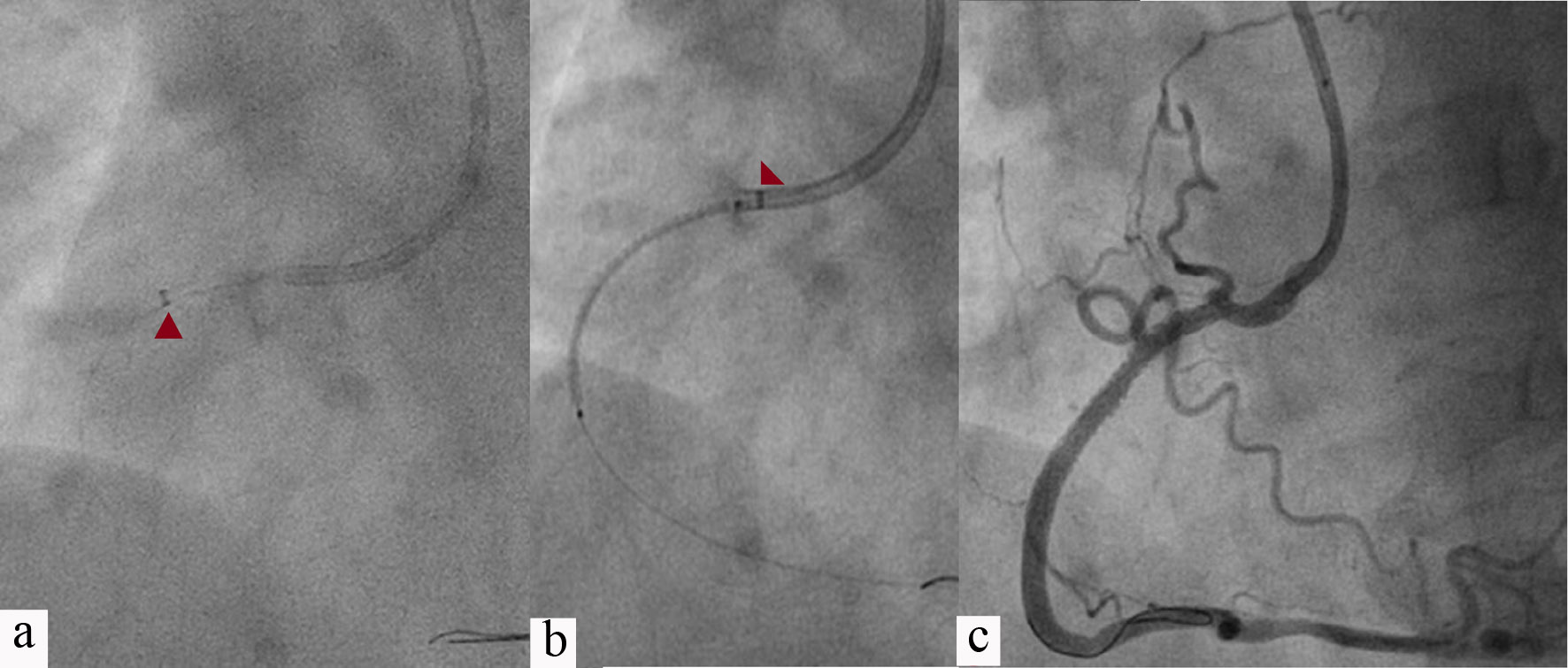
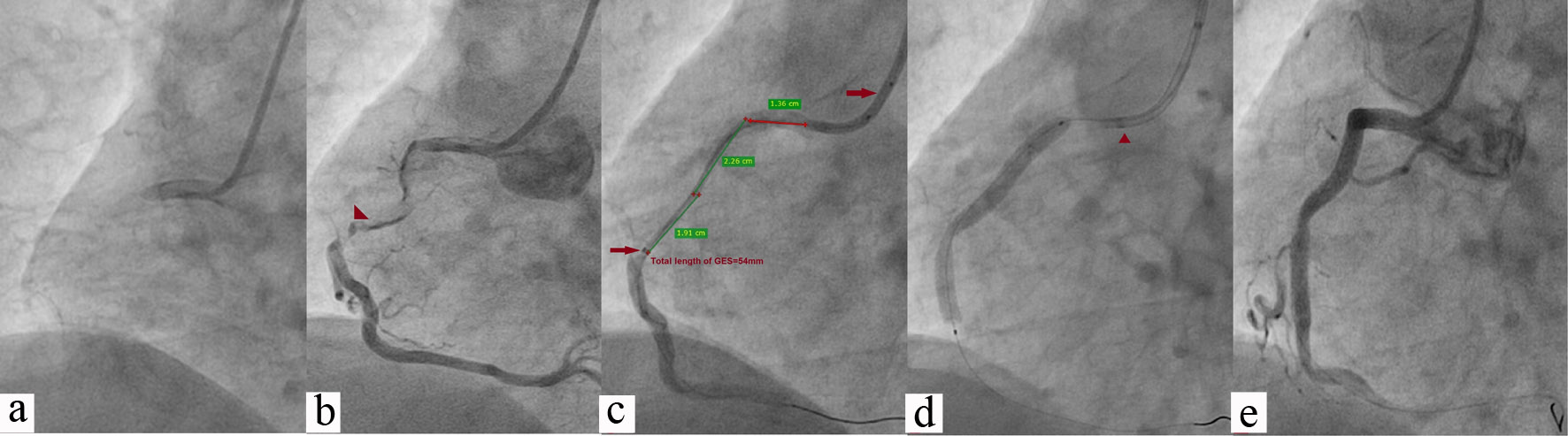
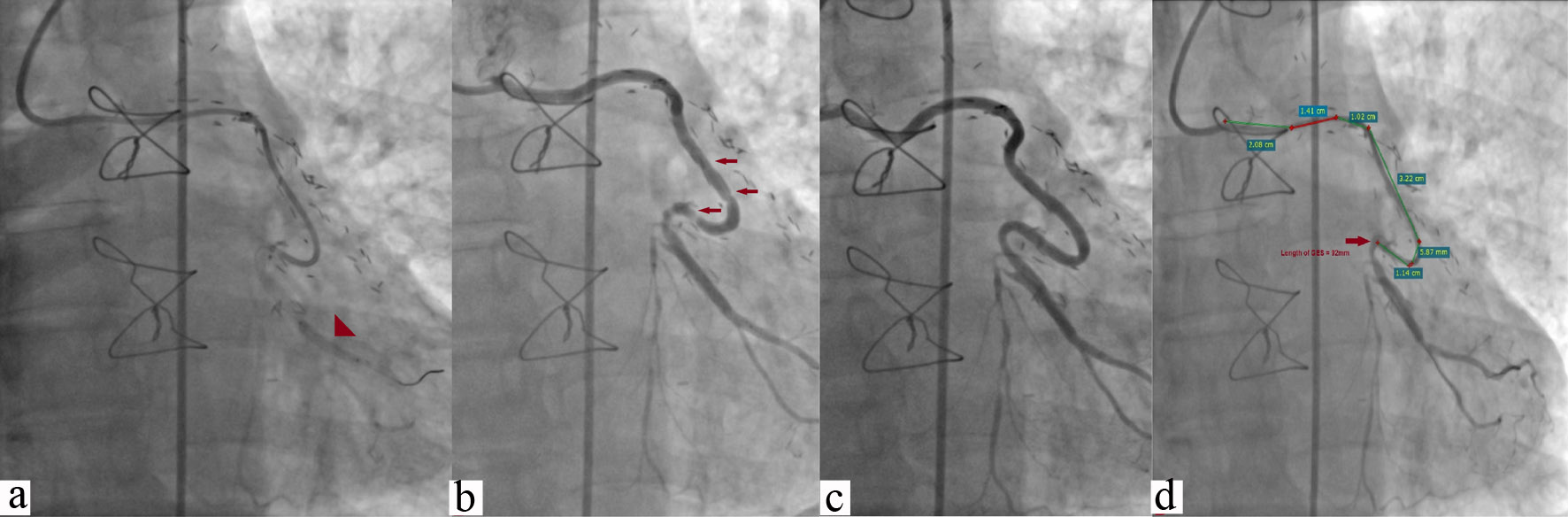
Figure 4. Chronic total occlusion of RCA (a); It was wired with Fielder XT with caravel microcatheter support (Asahi, Japan) (b); GEC was pushed beyond the lesion with balloon anchoring technique (54 mm, red arrowhead; c); 3.5 × 42 Supralimus Grace (Sirolimus-eluting stent, Sajahanand Medical, Gujarat, India) was positioned across lesion after pulling Guidezilla into guiding catheter (red arrowhead; d); Lesion was stented after deploying stent at 14 atm pressure showing TIMI 3 flow (e). RCA: right coronary artery; GEC: Guidezilla extension catheter; atm: atmospheric pressure; TIMI: thrombolysis in myocardial infarction.
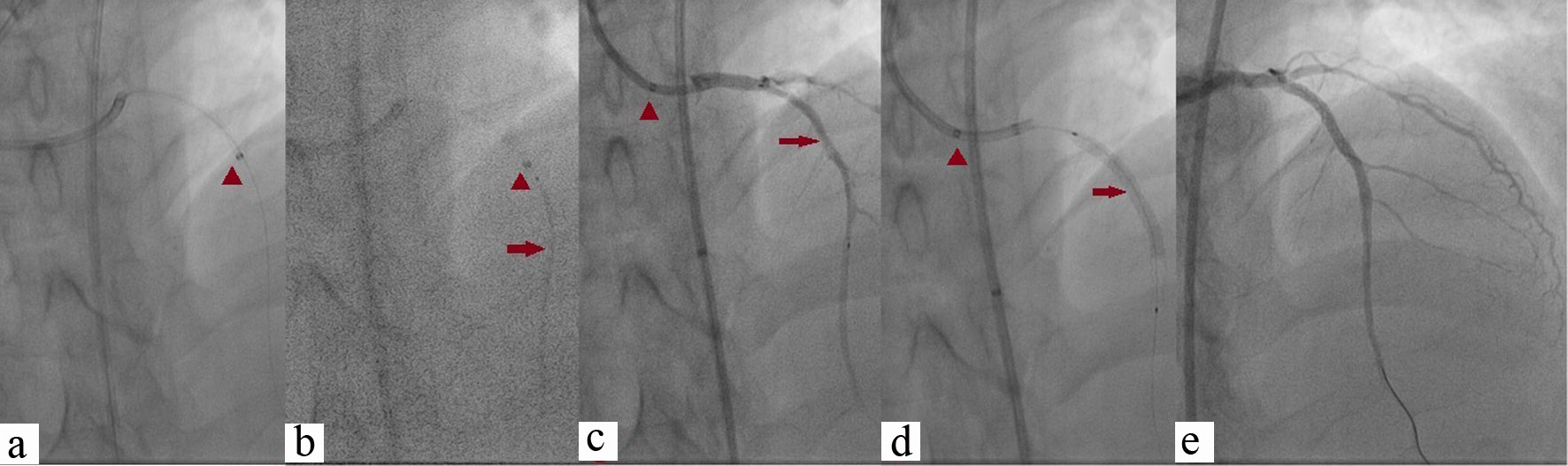
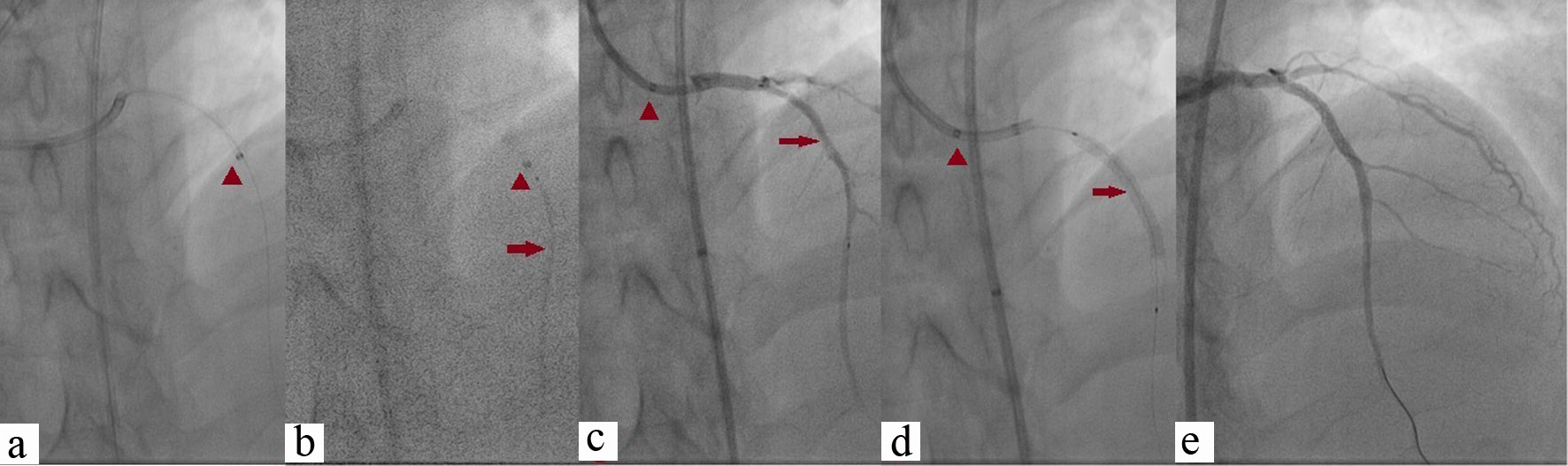
Figure 5. Chronic total occlusion of ostial LAD which was wired with Conquest-Pro 12 with caravel microcatheter support. Lesion was predilated and GEC was pushed beyond the lesion (red arrowhead; a, b); 3.5 × 42 Supralimus Grace was positioned across the lesion (red arrow; b, c) after pulling Guidezilla into guiding catheter (red arrowhead; c, d); Lesion was stented at 14 atm pressure showing TIMI 3 flow by pulling it further and properly positioned across the lesion (d, e). LAD: left anterior descending; GEC: Guidezilla extension catheter; atm: atmospheric pressure; TIMI: thrombolysis in myocardial infarction.
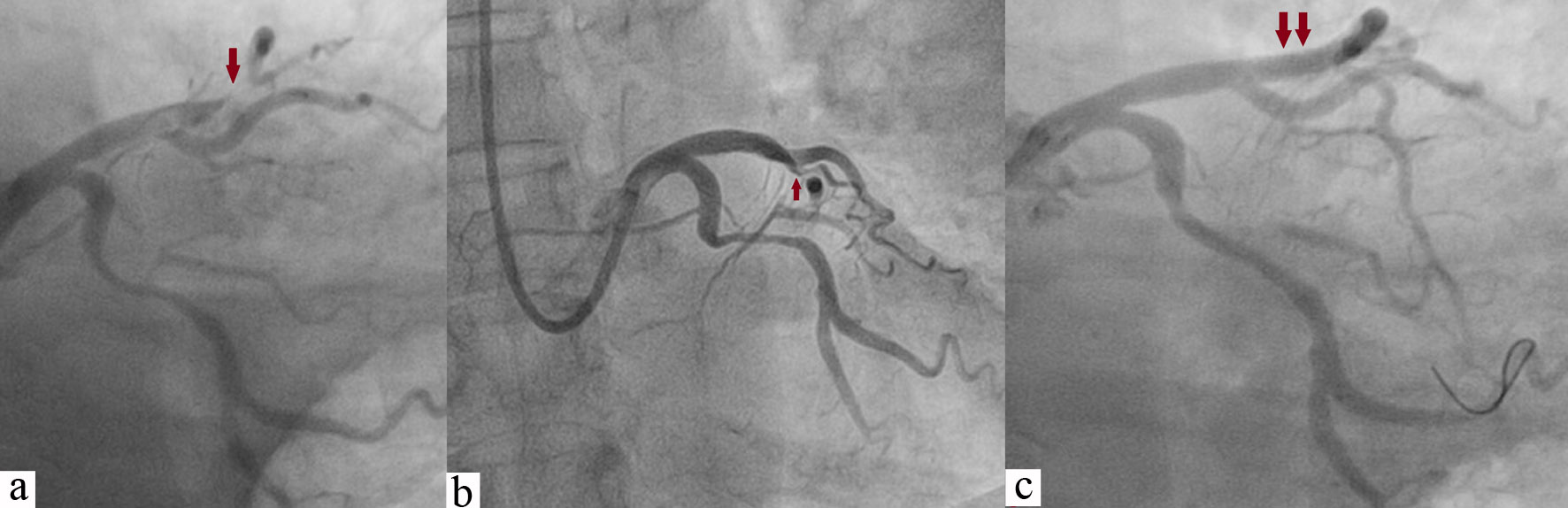
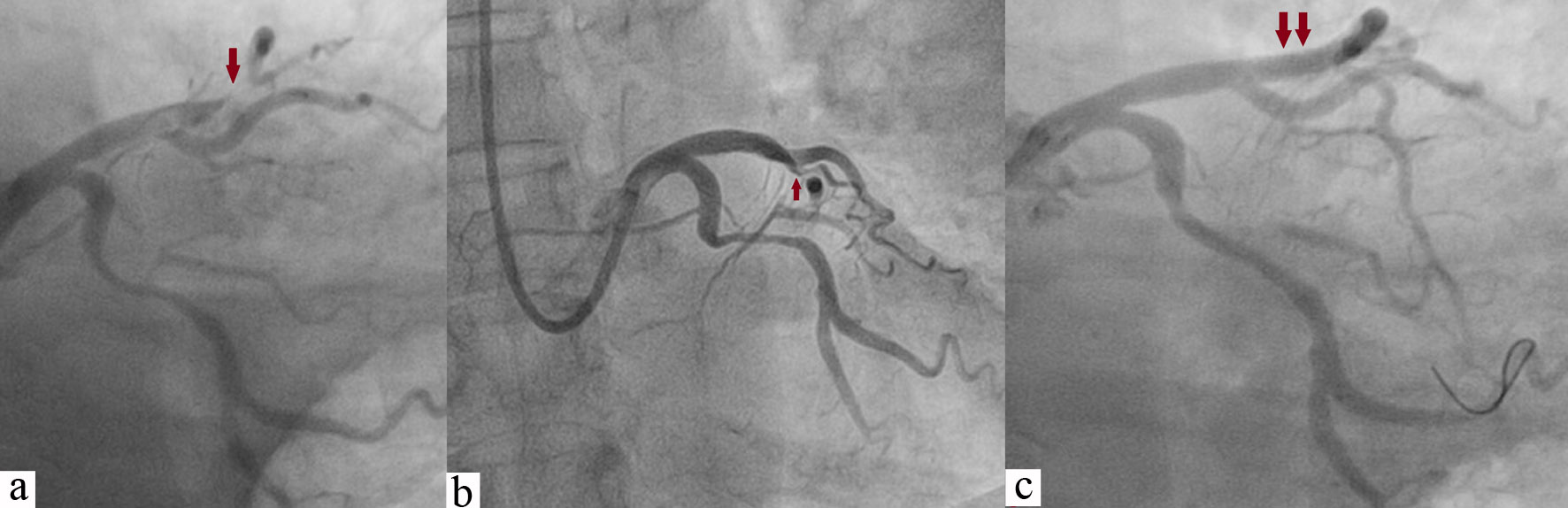
Figure 6. Tortuous diffuse lesion of LCX along with focal lesion of LAD (red arrow; a, b); LAD was stented with 3.5 × 18 mm Endeavour Resolute at 13 atm pressure achieving TIMI 3 flow (double arrow; c), and LCX was wired with Sion blue wire (c). LCX: left circumflex; LAD: left anterior descending; atm: atmospheric pressure; TIMI: thrombolysis in myocardial infarction.
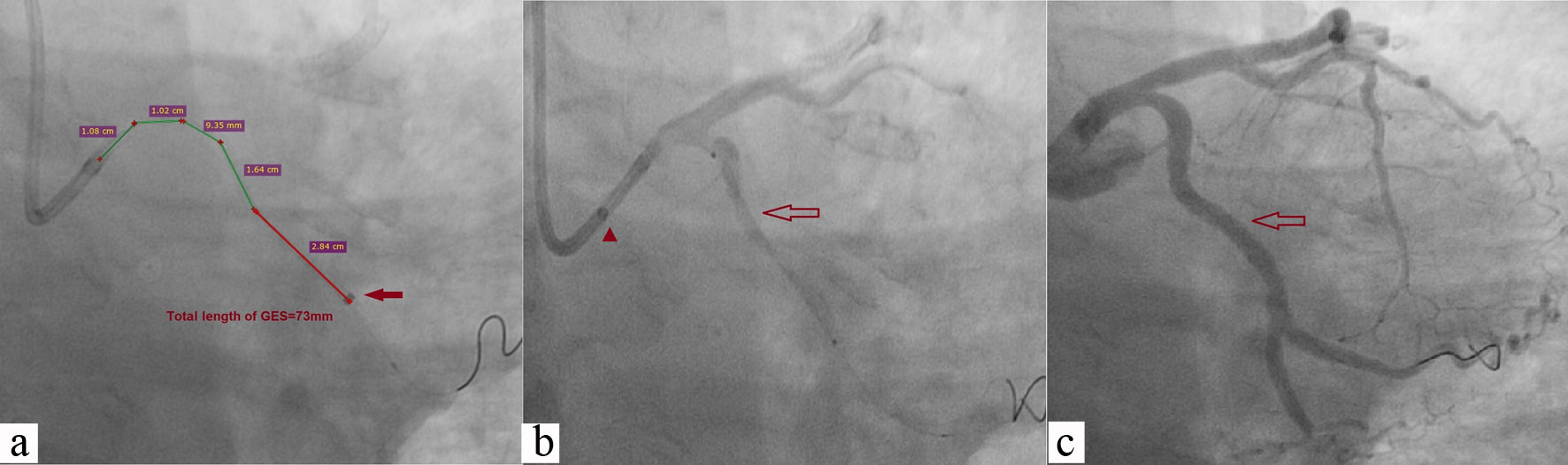
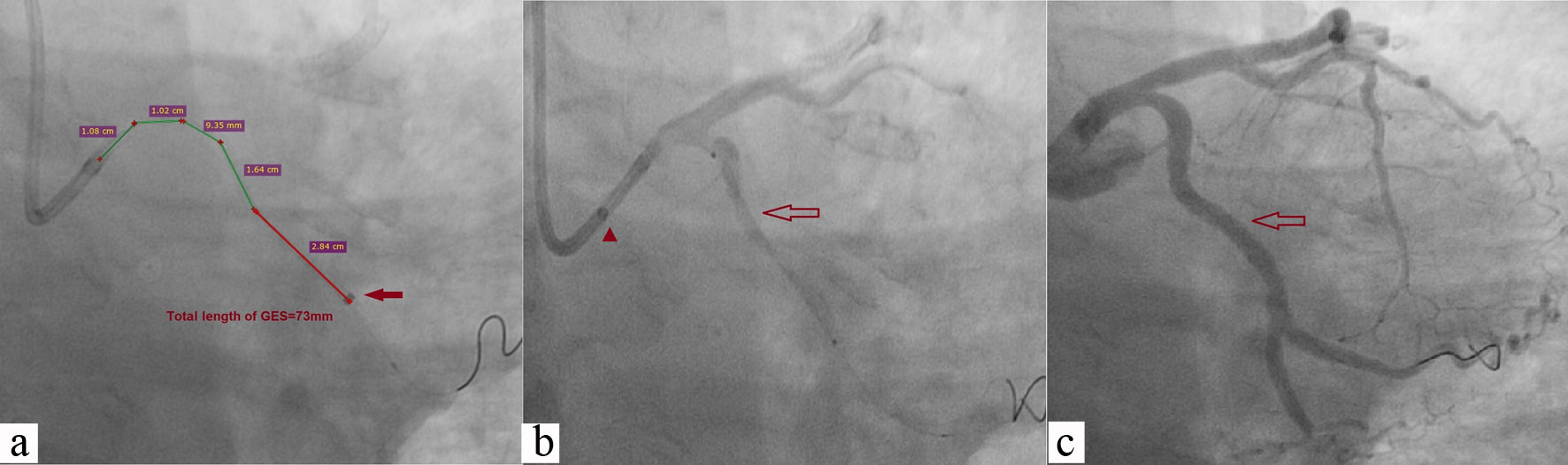
Figure 7. After adequate predilatation, GES was pushed beyond the lesion (73 mm, red arrow; a); 3.5 × 46 Supralimus Grace stent was positioned across the lesion after pulling Guidezilla into guiding catheter (red arrowhead; b); Lesion was stented after deploying stent at 14 atm pressure showing TIMI 3 flow (c). GEC: Guidezilla extension catheter; atm: atmospheric pressure; TIMI: thrombolysis in myocardial infarction.
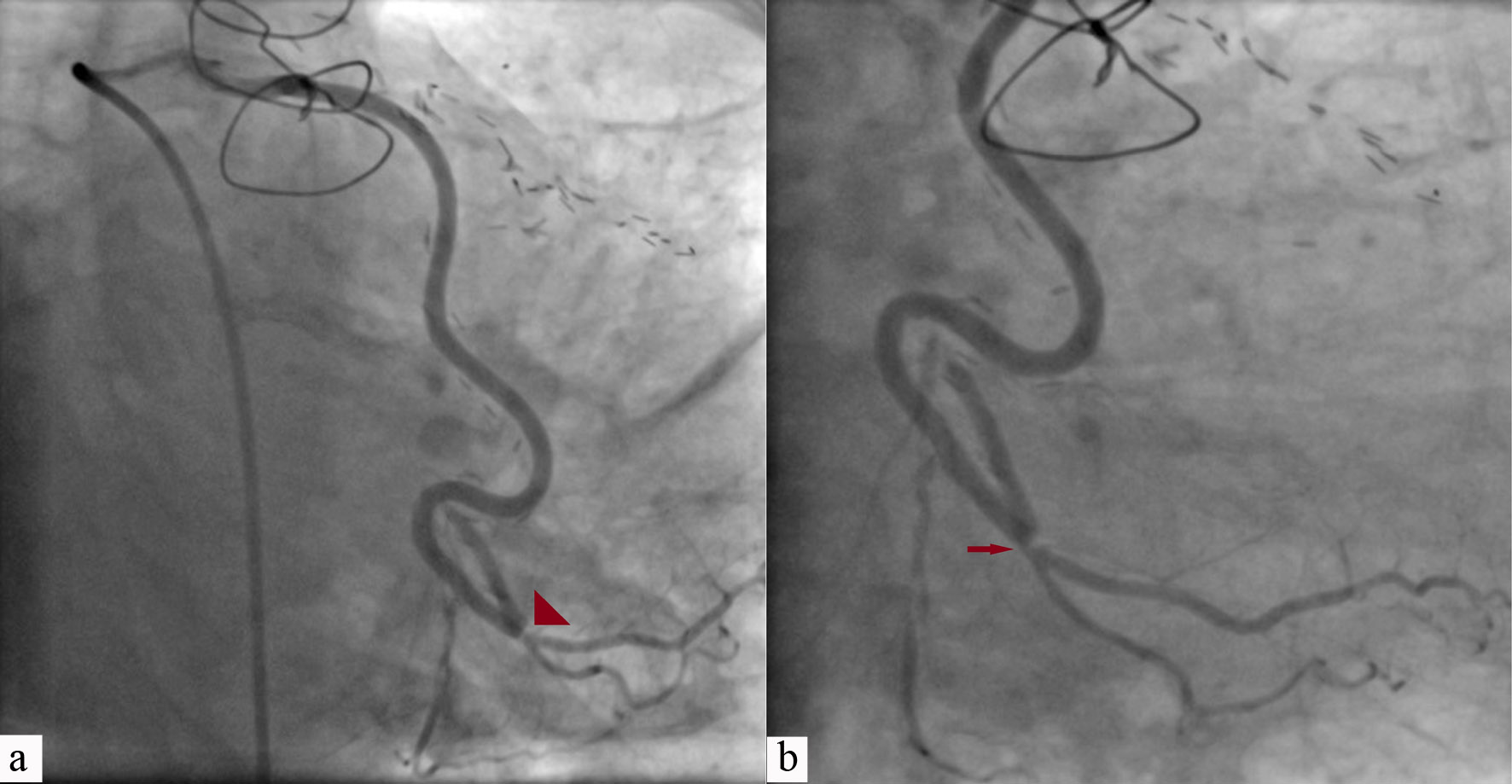
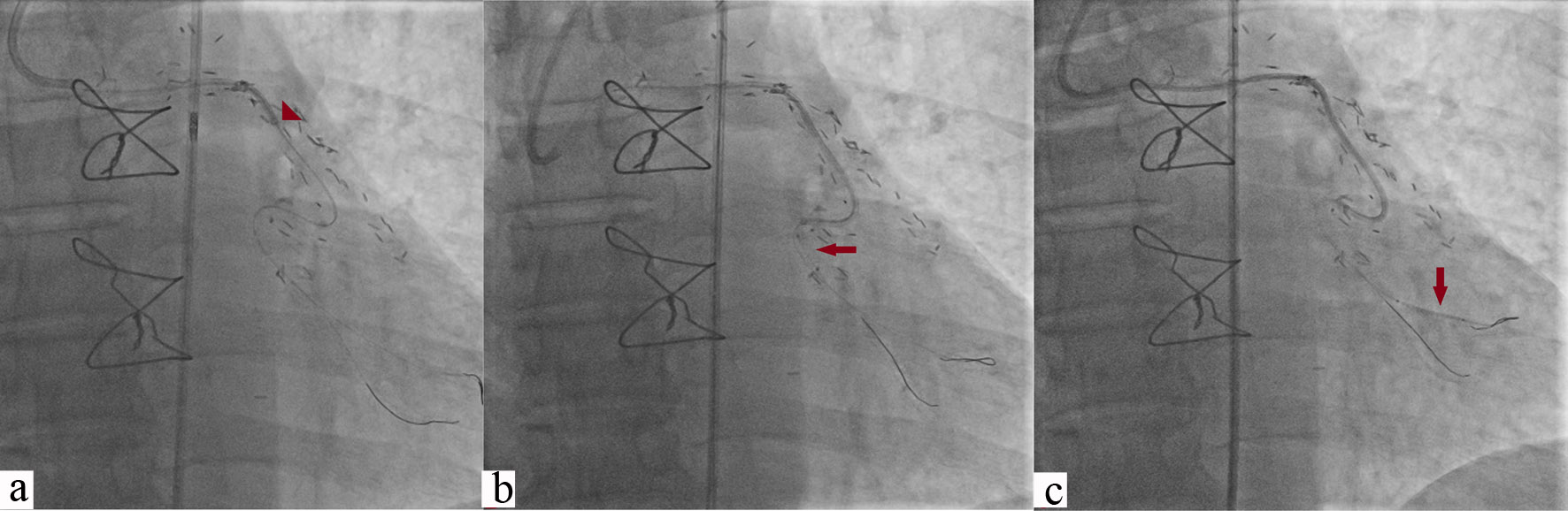
Figure 8. Critical stenosis of SVG to obtuse marginal branch of LCX at anastomotic site in a post-CABG patient who presented with stable angina of CCS class III (red arrowhead, a; red arrow, b). SVG: saphenous vein graft; LCX: left circumflex; CABG: coronary artery bypass graft; CCS: Canadian Cardiovascular Society.
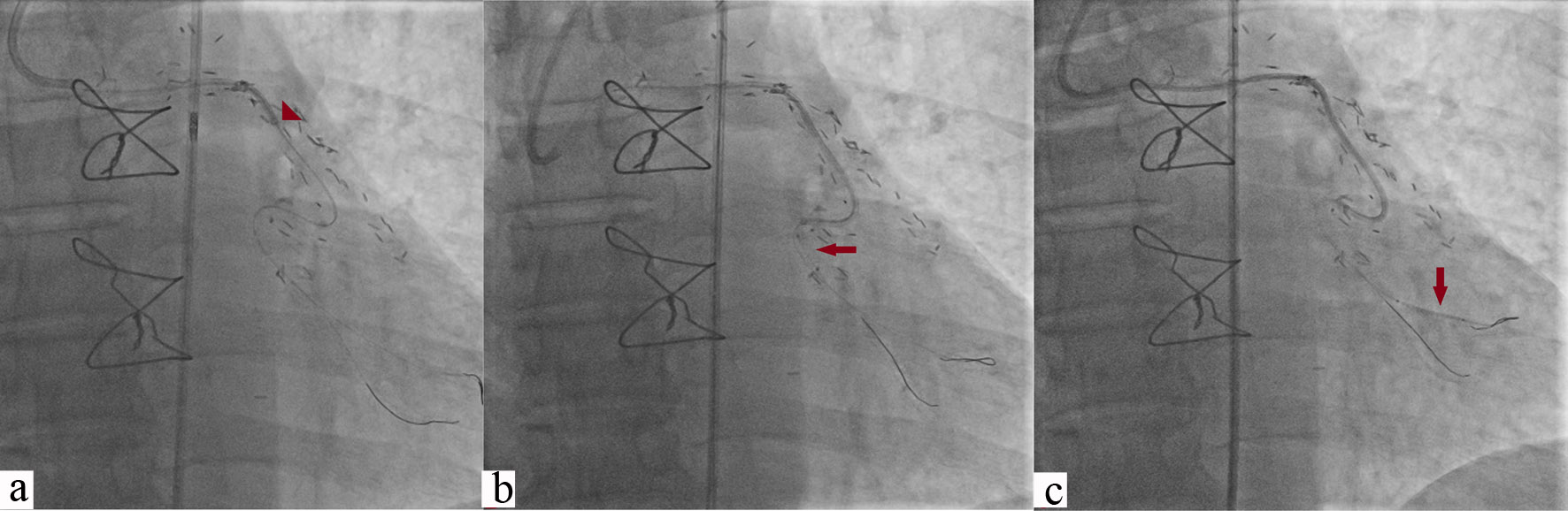
Figure 9. Lesion was wired using Sion blue wire and Guidezilla (red arrowhead) was advanced using buddy wire technique (a); Great difficulty was encountered to push GES which was further advanced with 2.5 × 10 mm sprinter legend balloon (red horizontal arrow, Medtronic, CA, USA) using BAT (b); 3 × 18 mm Endeavour Resolute stent (vertical arrow) was pushed beyond lesion by keeping buddy wire to garner adequate support (c). GEC: Guidezilla extension catheter; BAT: balloon-assisted tracking.
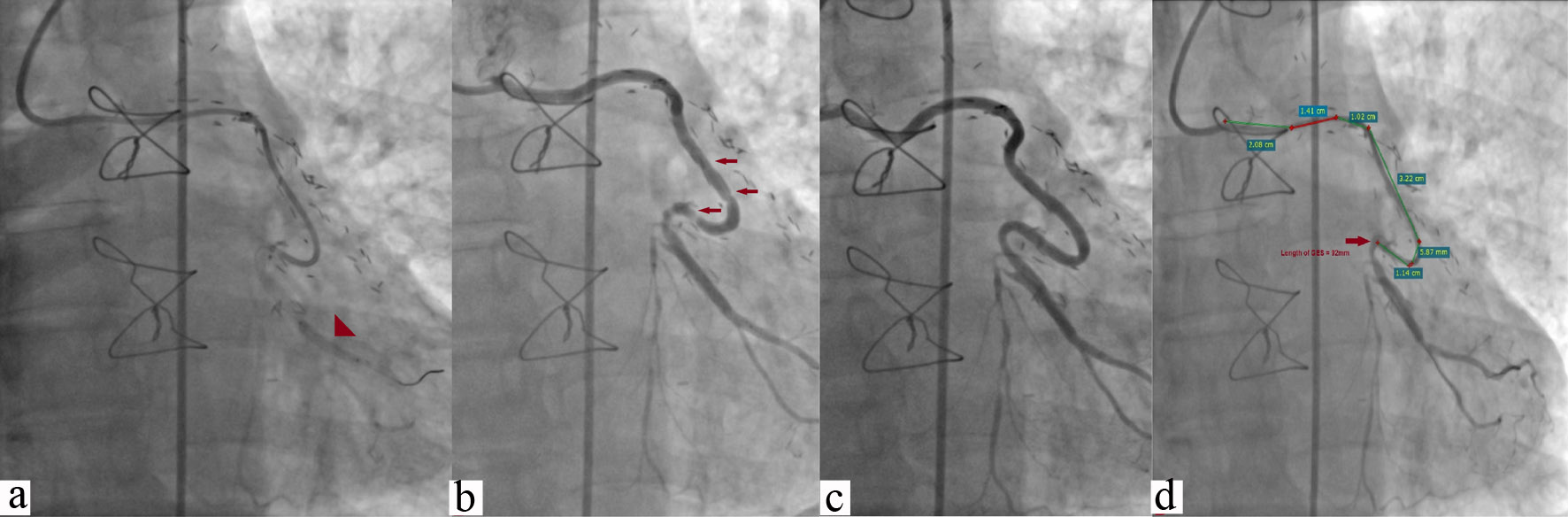
Figure 10. Stent was pulled to position across the lesion after removing buddy wire and deployed at 13 atm pressure (arrowhead) (a); TIMI 3 flow was achieved along with concertina effect (multiple horizontal arrows) after withdrawing GEC (b); Smooth flow after removing the wire which removed concertina effect which was wire bias effect (c); Deep intubation of Guidezilla catheter (92 mm) (d). atm: atmospheric pressure; GEC: Guidezilla extension catheter; TIMI: thrombolysis in myocardial infarction.
Tables
Table 1. Baseline Characteristics of Patients (n = 156)
| Variable | N (%) |
|---|
| STEMI: ST-segment elevation myocardial infarction; NSTEMI: non-ST-segment elevation myocardial infarction; UA: unstable angina; CSA: chronic stable angina. |
| Age (years) | 61.2 ± 8.67 |
| Male/female | 118 (75.6)/38 (24.3) |
| Hypertension | 52 (33.4) |
| Diabetes mellitus | 37 (23.7) |
| Dyslipidemia | 28 (17.9) |
| Smoking | 39 (25) |
| STEMI | 40 (25.6) |
| NSTEMI | 51 (32.7) |
| UA | 45 (28.9) |
| CSA | 20 (12.8) |
Table 2. Clinical and Procedural Data of Patients Who Underwent PCI Using Guidezilla Catheter (n = 156)
| Variable | N (%) |
|---|
| PCI: percutaneous coronary intervention; TRI: transradial intervention; TFI: transfemoral intervention; LAD: left anterior descending artery; LCX: left circumflex coronary artery; RCA: right coronary artery; SVG: saphenous vein graft; CTO: chronic total occlusion; PCI: percutaneous coronary intervention; GC: Guidezilla catheter; GEC: Guidezilla extension catheter; BAT: balloon anchoring technique; BLAST: balloon-assisted sliding and tracking. |
| Success/failure | 151 (96.7)/5 (3.2) |
| TRI/TFI | 54 (34.6)/102 (65.4) |
| Target vessel |
| LAD | 48 (30.8) |
| LCX | 31 (19.9) |
| RCA | 61 (39.2) |
| Multivessel | 12 (7.6) |
| SVG | 4 (2.5) |
| Lesion characteristics |
| Calcification | 33 (21.1) |
| Tortuosity | 47 (30.1) |
| Angulation | 29 (18.8) |
| Anomalous origin | 6 (3.8) |
| CTO | 28 (17.9) |
| Distally located lesion | 13 (8.3) |
| Type of lesion |
| B1 | 12 (7.7) |
| B2 | 35 (22.4) |
| C | 109 (69.9) |
| Mean diameter of the stents | 3.4 ± 1.2 mm |
| Mean length of stents | 34.2 ± 14.4 mm |
| Mean distance of intubation of GC into the target vessel | 4.2 ± 1.9 cm |
| Delivery of GEC catheter |
| Aggressive pre-dilatation | 137 (87.8) |
| Cutting balloon modification of the lesion | 17 (10.9) |
| Buddy wire technique | 15 (9.6) |
| BAT | 47 (30.1) |
| BLAST | 7 (4.5) |
| Complications (dissection, stent dislodgement) | 3 (1.9) |