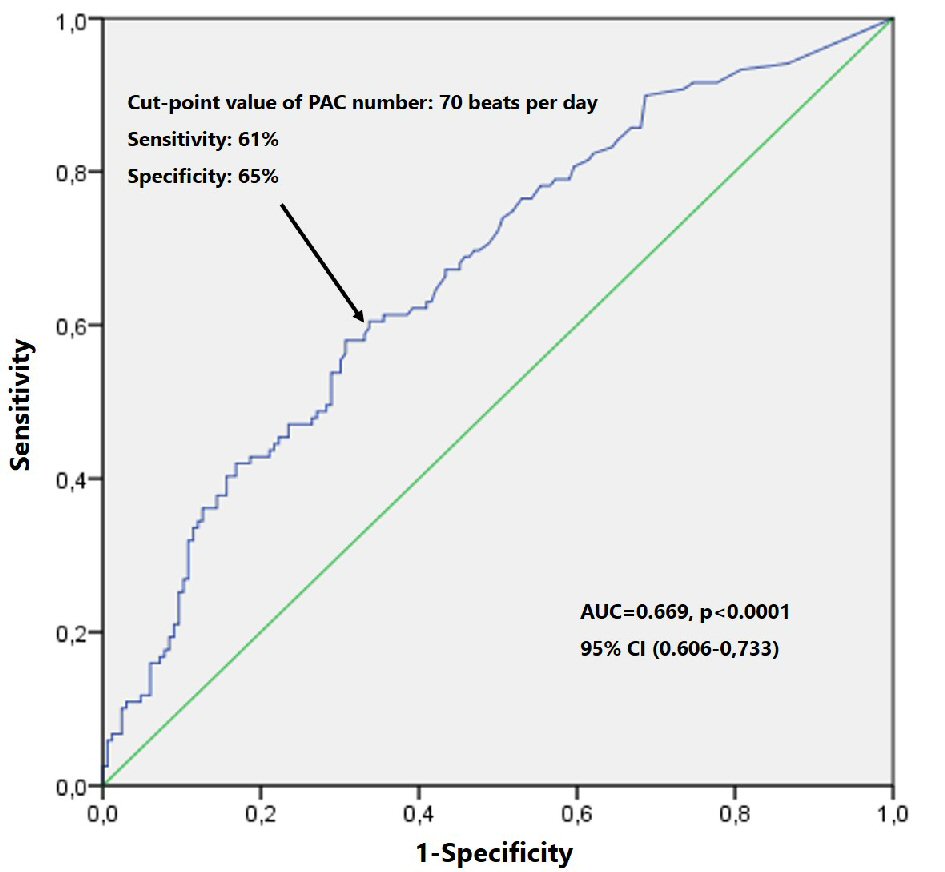
Figure 1. ROC curve survival analysis by PAC number. PAC: premature atrial contraction; ROC: receiver operator characteristic.
| Cardiology Research, ISSN 1923-2829 print, 1923-2837 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, Cardiol Res and Elmer Press Inc |
| Journal website http://www.cardiologyres.org |
Original Article
Volume 10, Number 5, October 2019, pages 268-277
Excessive Atrial Ectopic Activity Worsens Prognosis and Predicts the Type of Major Adverse Cardiac Events in Patients With Frequent Premature Ventricular Contractions
Figures
Tables
| Overall sample (n = 285) | EAEA (-) (n = 158) | EAEA (+) (n = 127) | P valuec | |
|---|---|---|---|---|
| Values are presented as median (interquartile range) or n (%). aThe CHA2DS2VASc score was calculated according to the presence of congestive heart failure/left ventricular dysfunction (1 point); hypertension (1 point); age ≥ 75 years (2 points); diabetes mellitus (1 point); history of stroke, transitory ischemic attack or thromboembolism (2 points); vascular disease (history of MI, vascular disease or aortic atherosclerosis) (1 point); age 65 - 74 years (1 point) and female gender (1 point). bClass I or class III antiarrhythmics. cP values were calculated using Mann-Whitney U test for continuous variables and the Chi-square test for categorical variables. EAEA: excessive atrial ectopic activity; NSVT: non-sustained ventricular tachycardia; PVC: premature ventricular contraction; PAC: premature atrial contraction; AV: atrioventricular; LAD: left atrium diameter; LVDD: left ventricular diastolic diameter; LVSD: left ventricular systolic diameter; LVFS: left ventricular fractional shortening. | ||||
| Demographic data | ||||
| Age (years) | 68 (60 - 76) | 62 (53 - 73) | 74 (66 - 79) | < 0.0001 |
| Male gender, n (%) | 171 (60) | 92 (58) | 79 (62) | 0.544 |
| Risk factors | ||||
| Diabetes, n (%) | 66 (26) | 35 (26) | 31 (27) | 0.887 |
| Hypertension, n (%) | 216 (86) | 108 (80) | 108 (93) | 0.003 |
| Dyslipidemia, n (%) | 143 (57) | 78 (58) | 65 (56) | 0.799 |
| High CHA2DS2VASca | 191(76) | 87 (64) | 104 (90) | < 0.0001 |
| Previous stroke, n (%) | 39 (14) | 19 (12) | 20 (15) | 0.390 |
| Etiology | ||||
| Structural heart disease, n (%) | 118 (41) | 67 (42) | 51 (40) | 0.718 |
| Ischemic heart disease n (%) | 86 (30) | 49 (73) | 37 (73) | 0.999 |
| Medications | ||||
| Beta-blockers, n (%) | 106 (37) | 67 (42) | 39 (31) | 0.049 |
| Antiarrhythmicsb, n (%) | 16 (6) | 8 (5) | 8 (6) | 0.797 |
| 24 - h Holter recording | ||||
| Maximal heart rate (bpm) | 113 (100 - 126) | 115 (102 - 126) | 109 (98 - 128) | 0.048 |
| Minimal heart rate (bpm) | 49 (43 - 54) | 49 (44 - 55) | 48 (42 - 53) | 0.153 |
| Mean heart rate (bpm) | 71 (64 - 79) | 73 (65 - 81) | 69 (63 - 78) | 0.035 |
| Number of PVCs/day | 2,776 (1,594 - 7,025) | 3,475 (1,623 - 8,402) | 2,461 (1,526 - 4,790) | 0.038 |
| Polymorphic morphology, n (%) | 192 (69%) | 94 (61) | 98 (81) | < 0.0001 |
| NSVT, n (%) | 54 (19) | 25 (16) | 29 (23) | 0.171 |
| Number of PACs/day | 48 (7 - 445) | 11 (1 - 29) | 636 (167 - 2,900) | < 0.0001 |
| Supraventricular runs, n (%) | 92 (32) | 22 (14) | 70 (55) | < 0.0001 |
| AV node conduction disease, n (%) | 49 (17) | 24 (15) | 25 (20) | 0.346 |
| Echocardiogram | ||||
| LAD (mm) | 37 (35 - 42) | 40 (35 - 45) | 38 (35 - 43) | 0.004 |
| LVDD (mm) | 53 (49 - 58) | 51 (48 - 56) | 55 (50 - 59) | 0.029 |
| LVSD (mm) | 34 (30 - 40) | 33 (30 - 40) | 35 (30 - 40) | 0.325 |
| LVFS (%) | 36 (30 - 40) | 36 (28 - 40) | 36 (30 - 40) | 0.975 |
| Follow-up in years | 8.4 (5.1 - 10) | 8.7 (7.6 - 10.3) | 7.6 (3.9 - 9.6) | < 0.0001 |
| Overall sample (n = 285) | NSVT (+) (n = 54) | NSVT (-) (n = 231) | P valuec | |
|---|---|---|---|---|
| Values are presented as median (interquartile range) or n (%). aThe CHA2DS2VASc score was calculated according to the presence of congestive heart failure/left ventricular dysfunction (1 point); hypertension (1 point); age ≥ 75 years (2 points); diabetes mellitus (1 point); history of stroke, transitory ischemic attack or thromboembolism(2 points); vascular disease (history of MI, vascular disease or aortic atherosclerosis) (1 point); age 65 - 74 years (1 point) and female gender (1 point). bClass I or class III antiarrhythmics. cP values were calculated using Mann-Whitney U test for continuous variables and the Chi-square test for categorical variables. EAEA: excessive atrial ectopic activity (> 70 PACs/day); SHD: structural heart disease; IHD: ischemic heart disease; NSVT: non-sustained ventricular tachycardia; PVC: premature ventricular contraction; PAC: premature atrial contraction; AV: atrioventricular; LAD: left atrium diameter; LVDD: left ventricular diastolic diameter; LVSD: left ventricular systolic diameter; LVFS: left ventricular fractional shortening. | ||||
| Demographic | ||||
| Age (years) | 68 (60 - 76) | 68 (61 - 76) | 68 (60 - 76) | 0.986 |
| Male gender, n (%) | 171 (60) | 43 (80) | 128 (55) | 0.001 |
| Risk factors | ||||
| Diabetes, n (%) | 66 (26) | 11 (23) | 55 (27) | 0.715 |
| Hypertension, n (%) | 216 (86) | 41 (87) | 175 (86) | 0.9999 |
| Dyslipidemia, n (%) | 143 (57) | 27 (57) | 116 (57) | 0.9999 |
| High CHA2DS2VASca | 191(76) | 40 (87) | 151 (74) | 0.082 |
| Previous stroke, n (%) | 39 (14) | 7 (13) | 32 (14) | 0.999 |
| Etiology | ||||
| SHD, n (%) | 118 (41) | 19 (35) | 148 (64%) | < 0.0001 |
| IHD n (%) | 86 (30) | 23 (34) | 63 (76) | 0.266 |
| Medications | ||||
| Beta-blockers, n (%) | 106 (37) | 21 (39) | 85 (37) | 0.876 |
| Antiarrhythmicsb, n (%) | 16 (6) | 1 (2) | 15 (7) | 0.322 |
| 24 - h Holter recording | ||||
| Maximal heart rate (bpm) | 113 (100 - 126) | 113 (102 - 126) | 113 (100 - 125) | 0.573 |
| Minimal heart rate (bpm) | 49 (43 - 54) | 51 (44 - 56) | 48 (43 - 53) | 0.097 |
| Mean heart rate (bpm) | 71 (64 - 79) | 76 (65 - 82) | 70 (64 - 78) | 0.088 |
| Number of PVC/day | 2,776 (1,594 - 7,025) | 3,573 (1,758 - 11,600) | 2,589 (1,564 - 6,172) | 0.068 |
| Polymorphic, n (%) | 192 (69%) | 46 (89) | 146 (66) | 0.001 |
| PAC > 70/day n (%) | 127 (44) | 29 (54) | 98 (43) | 0.171 |
| Number of PACs/day | 48 (7 - 445) | 86 (6 - 1,092) | 46 (7 - 382) | 0.587 |
| Supraventricular runs, n (%) | 92 (32) | 16 (30) | 76 (33) | 0.447 |
| AV node disease, n (%) | 49 (17) | 12 (22) | 37 (16) | 0.316 |
| Echocardiogram | ||||
| LAD (mm) | 37 (35 - 42) | 41 (36 - 45) | 38 (35 - 44) | 0.007 |
| LVDD (mm) | 53 (49 - 58) | 55 (52 - 63) | 51 (48 - 57) | < 0.0001 |
| LVSD (mm) | 34 (30 - 40) | 35 (30 - 48) | 33 (30 - 39 | 0.004 |
| LVFS (%) | 36 (30 - 40) | 34 (24 - 40) | 36 (30 - 40) | 0.081 |
| Follow-up in years | 8.4 (5.1 - 10) | 7.8 (3.8 - 9.5) | 8.6 (5.5 - 10) | 0.026 |
| Overall sample | EAEA (-) | EAEA (+) | P valuea | ||||||
|---|---|---|---|---|---|---|---|---|---|
| 2,158 person-years | 1,305 person-years | 853 person-years | |||||||
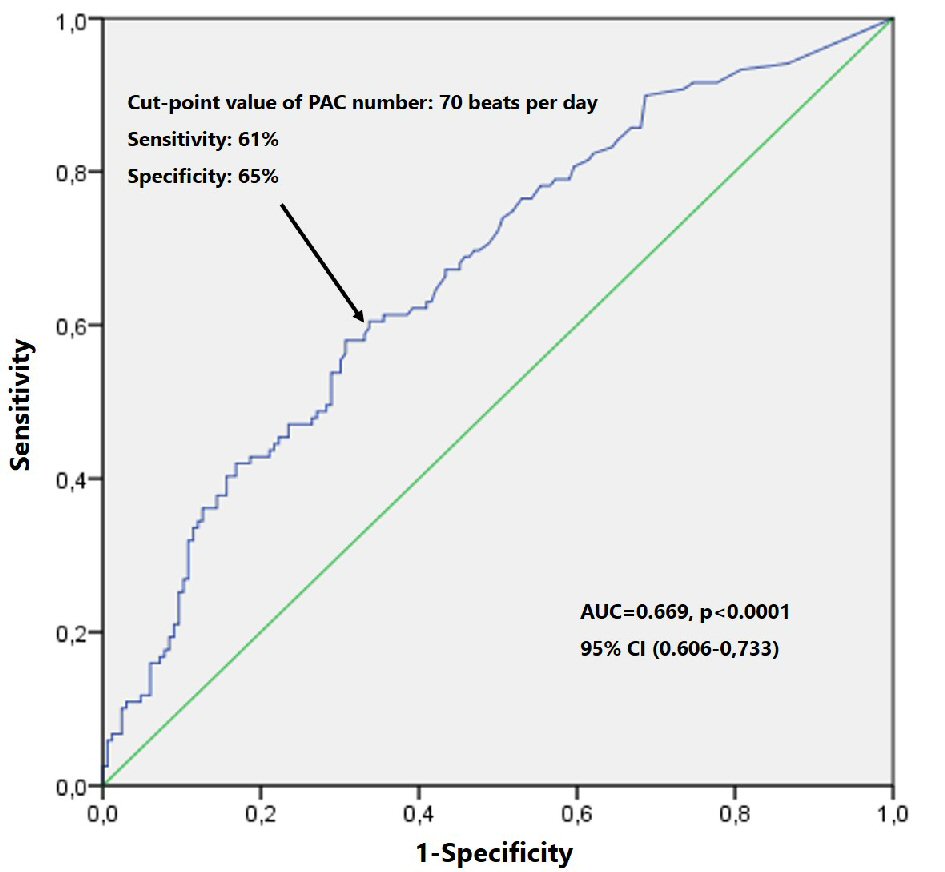
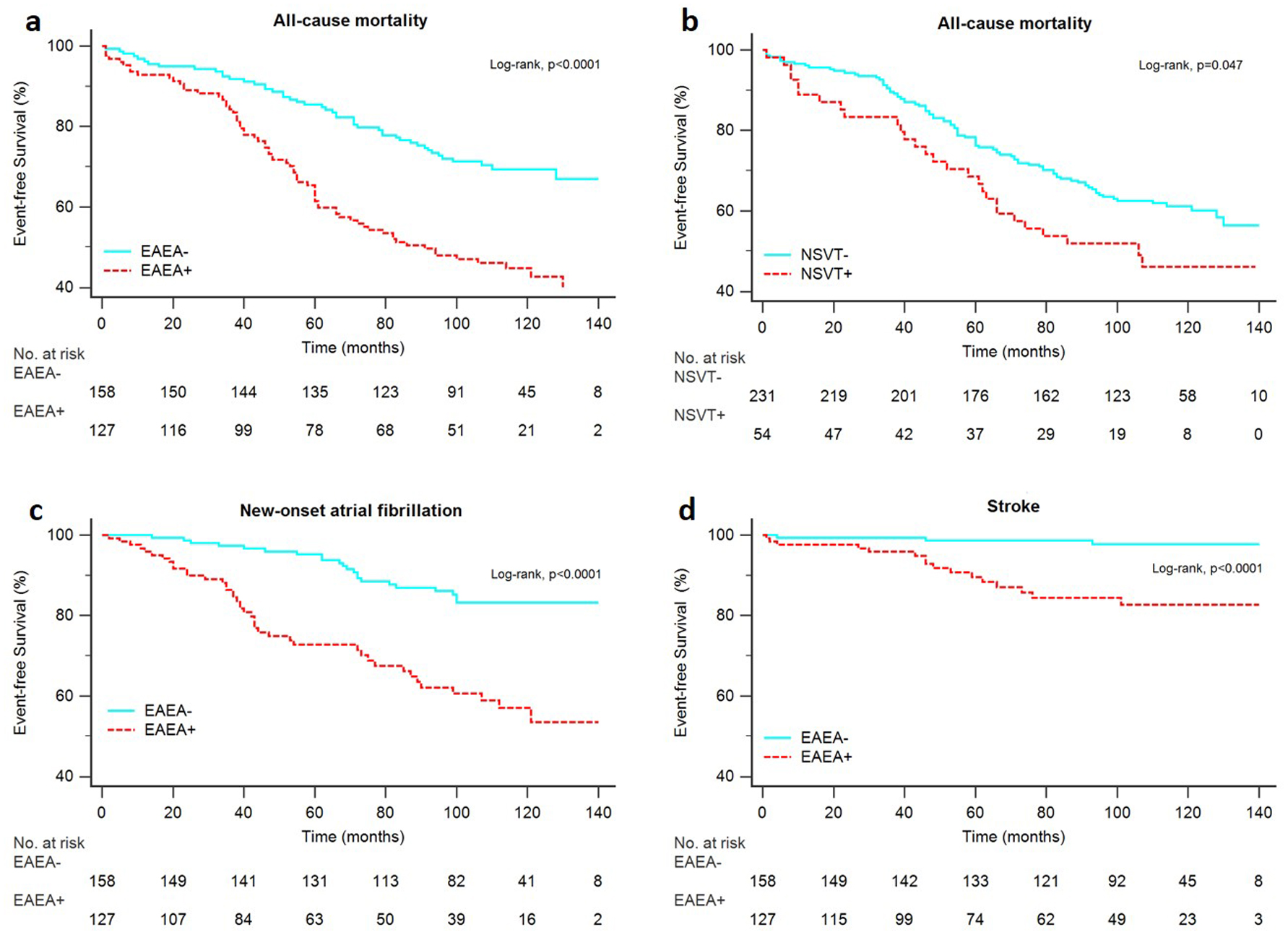
| All-cause death | 55 | 36.8 | 83.2 | < 0.0001 | |||||
| Stroke | 8.8 | 2.3 | 18.8 | < 0.0001 | |||||
| New-onset AF | 29.7 | 16.9 | 49.2 | < 0.0001 | |||||
| HF death or HF hospitalizations | 7 | 0.8 | 16.4 | < 0.0001 | |||||
| Arrhythmic death or VA hospitalizations | 6 | 5.4 | 7 | 0.661 | |||||
| Overall sample | NSVT (-) | NSVT (+) | P valuea | ||||||
| 2,158 person-years | 1,800 person-years | 358 person-years | |||||||
| Values are presented in number of events per 1,000 person-years. AF; atrial fibrillation; HF: heart failure; VA: ventricular arrhythmia; EAEA: excessive atrial ectopic activity; EAEA excessive atrial ectopic activity; NSVT: non-sustained VT episodes; NSVT: non-sustained VT episodes. aP values were calculated using the Log-rank test. | |||||||||
| All-cause death | 55 | 50.5 | 78 | 0.047 | |||||
| Stroke | 8.8 | 7.2 | 16.6 | 0.670 | |||||
| New-onset AF | 29.7 | 27.2 | 42 | 0.052 | |||||
| HF death or HF hospitalizations | 7 | 4.4 | 19.5 | 0.002 | |||||
| Arrhythmic death or VA hospitalizations | 6 | 5.5 | 16.8 | 0.003 | |||||
| End points | Unadjusted | Adjusted | ||
|---|---|---|---|---|
| HR (95% CI) | P value | HR (95% CI) | P valuef | |
| aHR adjusted to age, CHA2DS2VASc score, presence of SHD, beta-blocker therapy,new-onset AF, LAD and LVFS. bHR adjusted to age, CHA2DS2VASc score, previous stroke, LAD and new-onset AF. cHR adjusted to age, hypertension, diabetes, beta-blocker therapy, presence of SHD and LAD. dHR adjusted to the presence of age, SHD, beta-blocker therapy, new-onset AF and LVFS. eHR adjusted to the presence of age, beta-blocker therapy, structural heart disease and LVFS. fP values were calculated using the Cox proportional-hazards model. PAC: premature atrial contraction; AF: atrial fibrillation; HF: heart failure; VA: ventricular arrhythmia; NSVT: non-sustained ventricular tachycardia; LAD: left atrium diameter; LVFS: left ventricular fractional shortening; SHD: structural heart disease. | ||||
| Log2 number of PACs/day | ||||
| All - cause death | 1.131 (1.080 - 1.084) | < 0.0001 | 1.077 (1.014 - 1.145)a | 0.017 |
| Stroke | 1.321 (1.163 - 1.501) | < 0.0001 | 1.250 (1.080 - 1.447)b | 0.003 |
| New-onset AF | 1.193 (1.117 - 1.275) | < 0.0001 | 1.090 (1.006 - 1.181)c | 0.036 |
| HF death or HF hospitalizations | 1.287 (1.119 - 1.482) | < 0.0001 | 1.376 (1.128 - 1.679)d | 0.002 |
| Arrhythmic death or VA hospitalizations | 1.080 (0.941 - 1.240) | 0.273 | - | |
| NSVT | ||||
| All - cause death | 1.530 (1.001 - 2.337) | 0.049 | 1.584 (0.990 - 2.534)a | 0.055 |
| HF death or HF hospitalizations | 4.255 (1.542 - 11.74) | 0.005 | 1.519 (0.497 - 4.643)c | 0.464 |
| Arrhythmic death or VA hospitalizations | 4.424 (1.484 - 13.19) | 0.008 | 3.644 (1.147 - 11.57)e | 0.028 |