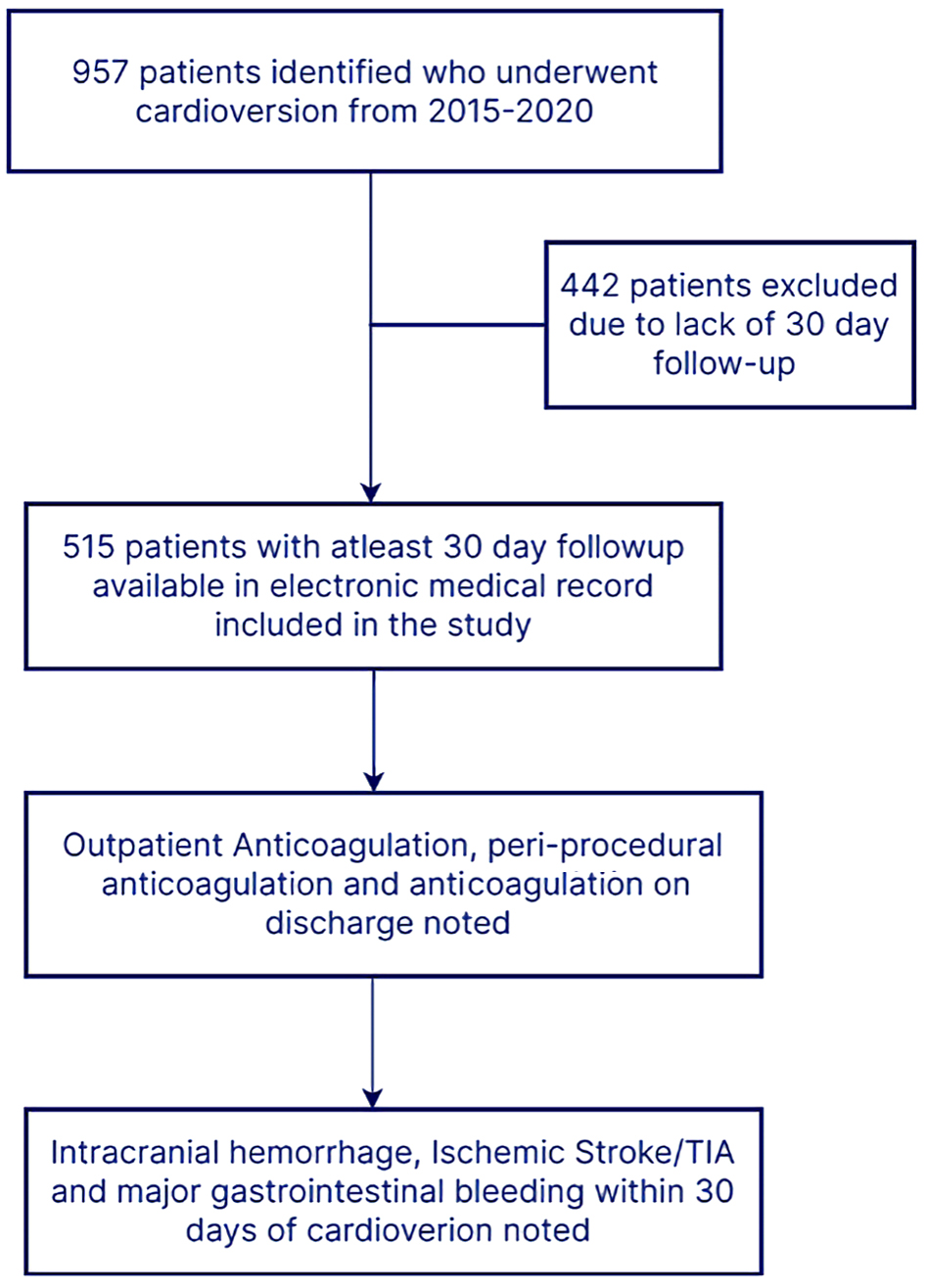
Figure 1. Study flowchart. TIA: transient ischemic attack.
| Cardiology Research, ISSN 1923-2829 print, 1923-2837 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, Cardiol Res and Elmer Press Inc |
| Journal website https://www.cardiologyres.org |
Original Article
Volume 13, Number 2, April 2022, pages 88-96
Trends and Outcomes of Oral Anticoagulation With Direct Current Cardioversion for Atrial Fibrillation/Flutter at an Academic Medical Center
Figures
Tables
| Baseline patient characteristics | N = 515 |
|---|---|
| LVAD: left ventricular assist device; LVEF: left ventricular ejection fraction; TIA: transient ischemic attack. | |
| Males | 351 (68%) |
| Diabetes mellitus | 146 (28%) |
| Hypertension | 311 (60%) |
| Coronary artery disease | 153 (30%) |
| Hyperlipidemia | 172 (33%) |
| Chronic kidney disease | 47 (9%) |
| End-stage renal disease | 11 (2%) |
| Renal transplant | 6 (1%) |
| Heart failure | 266 (52%) |
| LVAD | 8 (1%) |
| Heart transplant | 2 (< 1%) |
| Liver cirrhosis | 9 (2%) |
| Body mass index | 32 (16 - 78) |
| Congestive heart failure | 266 (52%) |
| LVEF < 40% | 171 (33%) |
| CHA2DS2VASc | 2.6 ± 1.6 |
| 0 | 40 (8%) |
| 1 | 89 (17%) |
| 2 | 123 (24%) |
| 3 | 94 (18%) |
| 4 | 78 (15%) |
| 5 | 48 (9%) |
| 6 | 16 (3%) |
| 7 | 4 (< 1%) |
| 8 | 3 (< 1%) |
| Prior stroke/TIA | 38 (7%) |
| Prior major bleeding | 25 (5%) |
| Prior venous thromboembolism | 64 (12%) |
| Prior cardioversion | 140 (27%) |
| Prior ablation | 42 (8%) |
| Reason | N = 31 |
|---|---|
| CABG: coronary artery bypass graft; LAA: left atrial appendage. | |
| Cardioversion post CABG and anticoagulation deemed not necessary by surgeon | 5 |
| Recent surgery and anticoagulation deemed not safe | 1 |
| Significant thrombocytopenia (< 50,000) | 2 |
| Patient refusal | 1 |
| HAS-BLED score ≥ 3 | 1 |
| Recent gastrointestinal bleeding | 3 |
| LAA occlusion device with prior history of major bleeding | 3 |
| Multi-organ dysfunction | 4 |
| Indiscernible | 11 |
| Demographics | DOACs, n = 338 (65%) | Warfarin, n = 124 (24%) | P value |
|---|---|---|---|
| *P value < 0.05. EF: ejection fraction. | |||
| Age | 62 ± 13.073 | 61 ± 13.5 | 0.721 |
| CHA2DS2VASc | 2.65 ± 1.6 | 2.9 ± 1.4 | 0.037* |
| Body mass index | 32.1 ± 8.1 | 34.3 ± 11.1 | 0.017* |
| Male gender | 235 (70%) | 80 (65%) | 0.306 |
| Diabetes mellitus | 91 (27%) | 38 (31%) | 0.429 |
| Hypertension | 202 (60%) | 77 (62%) | 0.65 |
| Coronary artery disease | 96 (28%) | 43 (35%) | 0.193 |
| Hyperlipidemia | 109 (32%) | 49 (40%) | 0.145 |
| Chronic kidney disease stage 3 - 5 | 23 (7%) | 20 (16%) | 0.002* |
| End-stage renal disease | 5 (1%) | 5 (4%) | 0.08 |
| Congestive heart failure | 172 (51%) | 49 (40%) | 0.09 |
| Heart failure with reduced ejection fraction (EF < 40%) | 106 (31%) | 53 (43%) | 0.023* |
| History of prior stroke | 24 (7%) | 12 (10%) | 0.36 |
| History of venous thromboembolism | 34 (11%) | 21 (17%) | 0.043* |
| Prior history of major bleeding | 7 (2%) | 8 (6%) | 0.019* |
| Concomitant aspirin use | 78 (23%) | 48 (39%) | 0.001* |
| Concomitant clopidogrel use | 8 (2%) | 9 (7%) | 0.013* |
| Triple antithrombotic therapy | 1 (< 1%) | 5 (4%) | 0.002* |
| Transesophageal echocardiogram prior to cardioversion | 140 (41%) | 54 (44%) | 0.681 |
| Prior cardioversions | 94 (28%) | 36 (29%) | 0.796 |
| Atrial fibrillation | 218 (65%) | 71 (57%) | 0.154 |
| Atrial flutter | 120 (36%) | 53 (43%) | 0.154 |
| Anti-arrhythmic use prior to cardioversion | 137 (41%) | 53 (43%) | 0.686 |
| Age | Gender | CHA2DS2VASc | TEE | Anticoagulation | Comments |
|---|---|---|---|---|---|
| TEE: transesophageal echocardiography. | |||||
| 53 | Male | 0 | Not performed | Warfarin | Preceding surgery for ischemic bowel |
| 57 | Female | 2 | Not performed | Rivaroxaban | Seizure |
| 64 | Male | 3 | Not performed | None | Preceding liver transplant surgery |
| 61 | Female | 4 | Not performed | None | Recent gastrointestinal bleed |