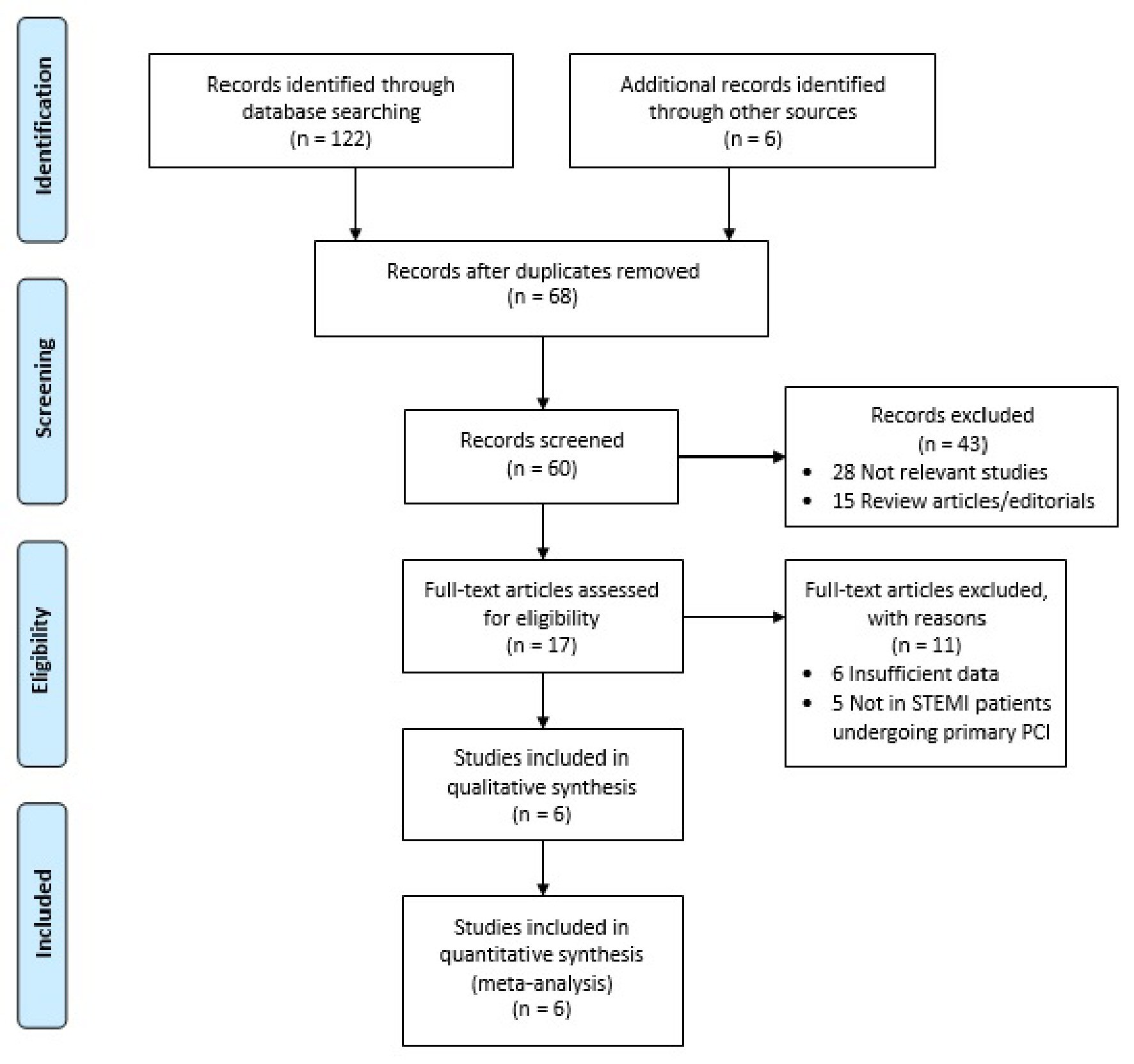
Figure 1. Literature search flow chart. PCI: percutaneous coronary intervention; STEMI: ST-segment elevation myocardial infarction.
| Cardiology Research, ISSN 1923-2829 print, 1923-2837 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, Cardiol Res and Elmer Press Inc |
| Journal website https://www.cardiologyres.org |
Original Article
Volume 12, Number 2, April 2021, pages 109-116
Platelet-to-Lymphocyte Ratio at Admission as a Predictor of In-Hospital and Long-Term Outcomes in Patients With ST-Segment Elevation Myocardial Infarction Undergoing Primary Percutaneous Coronary Intervention: A Systematic Review and Meta-Analysis
Figures
Tables
| Study, year | Country | Design | Sample size | Age (years) | Male (%) | Follow-up duration | PLR cut-off | Outcomes |
|---|---|---|---|---|---|---|---|---|
| PLR: platelet-to-lymphocyte ratio; RC: retrospective cohort; PC: prospective cohort; MACE: major adverse cardiac events. | ||||||||
| Ayca et al, 2014 [20] | Turkey | RC | 440 | 56 | 67 | During hospitalization | 137 | In-hospital MACE, in-hospital mortality |
| Ugur et al, 2014 [21] | Turkey | PC | 639 | 56 | 85 | 6 months | 175 | In-hospital MACE, in-hospital mortality, long-term MACE, long-term mortality |
| Cetin et al, 2015 [22] | Turkey | PC | 1,938 | 60 | 66 | 32 months | 147 | In-hospital MACE, in-hospital mortality, long-term MACE, long-term mortality |
| Toprak et al, 2015 [23] | Turkey | PC | 304 | 60 | 81 | 24 months | 217 | In-hospital MACE, in-hospital mortality, long-term MACE, long-term mortality |
| Hudzik et al, 2015 [24] | Poland | PC | 523 | 64 | 41 | 12 months | 124 | In-hospital mortality, long-term mortality |
| Maimati et al, 2019 [25] | China | RC | 445 | 61 | 65 | During hospitalization | 165 | In-hospital MACE, in-hospital mortality |
| Study, year | Selection | Comparability | Outcome | Total rating |
|---|---|---|---|---|
| Ayca et al, 2014 [20] | ★★★★ | ★★ | ★★ | 8★ |
| Ugur et al, 2014 [21] | ★★★★ | ★★ | ★★★ | 9★ |
| Cetin et al, 2015 [22] | ★★★★ | ★★ | ★★★ | 9★ |
| Toprak et al, 2015 [23] | ★★★★ | ★★ | ★★★ | 9★ |
| Hudzik et al, 2015 [24] | ★★★★ | ★★ | ★★ | 8★ |
| Maimati et al, 2019 [25] | ★★★★ | ★★ | ★★ | 8★ |