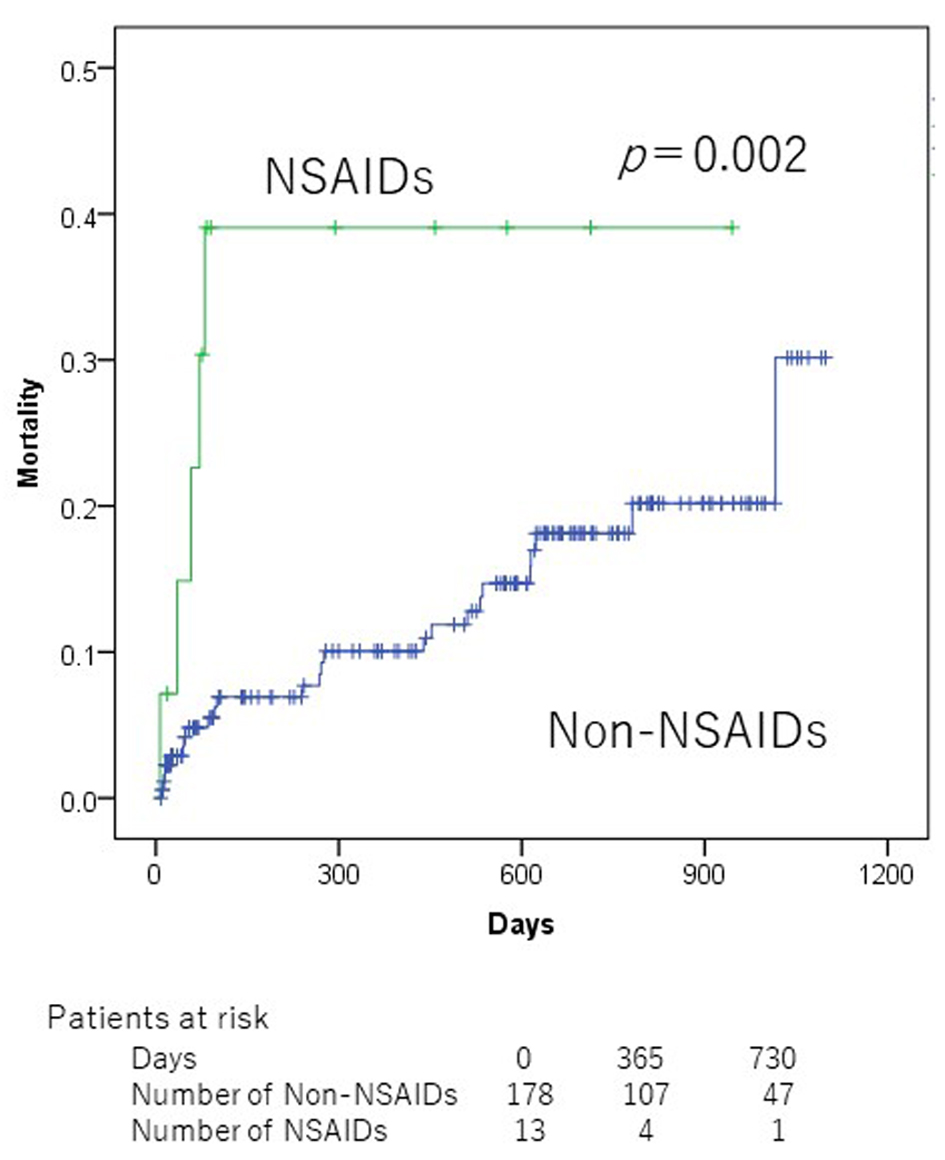
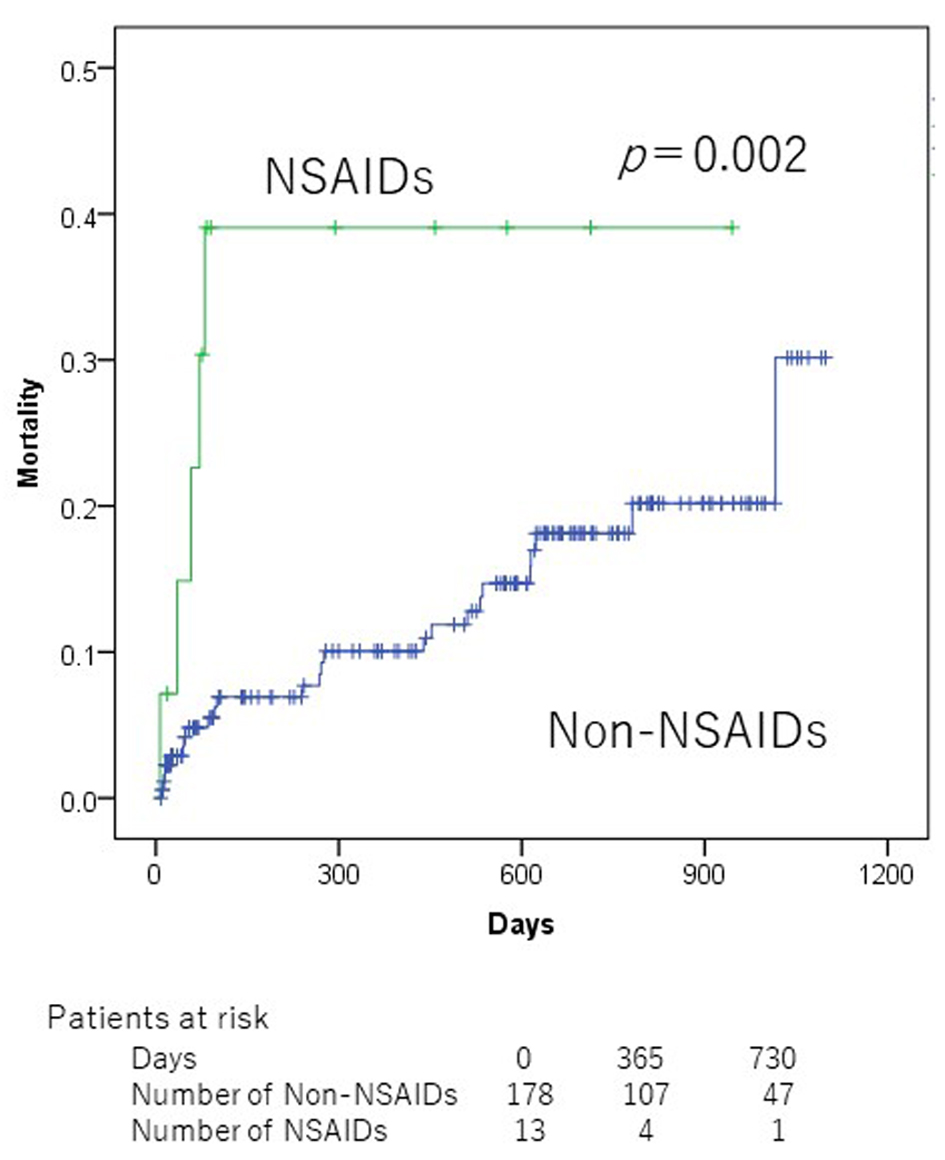
Figure 1. Kaplan-Meier mortality curves according to non-steroidal anti-inflammatory drug use at admission.
| Cardiology Research, ISSN 1923-2829 print, 1923-2837 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, Cardiol Res and Elmer Press Inc |
| Journal website http://www.cardiologyres.org |
Original Article
Volume 11, Number 4, August 2020, pages 239-246
Association of Potentially Inappropriate Medications With All-Cause Mortality in the Elderly Acute Decompensated Heart Failure Patients: Importance of Nonsteroidal Anti-Inflammatory Drug Prescription
Figures
Tables
| Variables | n (%), mean ± SD |
|---|---|
| SD: standard deviation; Hb: hemoglobin; Alb: albumin; BUN: blood urea nitrogen; GFR: glomerular filtration rate; HD: hemodialysis; COPD: chronic obstructive pulmonary disease; CS: clinical scenario; LVEF: left ventricular ejection fraction; PIM: potentially inappropriate medication; NSAIDs: non-steroidal anti-inflammatory drugs; PPIs: proton pump inhibitors. | |
| Age (years) | 80.7 ± 7.5, median: 81 (65 - 99) |
| 65 - 79 | 84 (43.5%) |
| ≥ 80 | 109 (56.5%) |
| Sex | |
| Male | 109 (56.5%) |
| Female | 84 (43.5%) |
| Clinical laboratory data on admission | |
| Hb (g/dL) | 11.2 ± 2.2 |
| Alb (g/dL) | 3.4 ± 0.5 |
| BUN (mg/dL) | 31.2 ± 18.1 |
| GFR (mL/min/1.73 m2) | 42.3 ± 21.3 |
| Type of comorbidity | |
| Hypertension | 156 (80.8%) |
| Dyslipidemia | 87 (45.1%) |
| Diabetes mellitus | 82 (42.5%) |
| Chronic renal disease on HD | 7 (3.6%) |
| Atrial fibrillation/flutter | 96 (49.7%) |
| Coronary artery disease | 64 (33.1%) |
| COPD | 15 (7.8%) |
| Cancer | 32 (16.6%) |
| Etiology | |
| Ischemic heart disease | 67 (34.7%) |
| Hypertensive disease | 29 (15.0%) |
| Valvular disease | 31 (16.1%) |
| Other | 66 (34.2%) |
| CS class | |
| 1 | 83 (43.0%) |
| 2 | 93 (48.2%) |
| Other | 17 (8.8%) |
| LVEF | |
| EF < 40% | 81 (42.0%) |
| EF ≥ 40% | 95 (49.2%) |
| Unkown | 17 (8.8%) |
| PIMs | |
| Benzodiazepine | 26 (13.5%) |
| Non-benzodiazepine hypnotics | 16 (8.3%) |
| Sulfonylurea | 18 (9.3%) |
| Thiazolidinediones | 3 (1.6%) |
| Metformin | 7 (3.6%) |
| Steroid | 7 (3.6%) |
| NSAIDs | 14 (7.3%) |
| H2 antagonists | 19 (9.8%) |
| PPIs | 87 (45.1%) |
| Non-dihydropyridine calcium channel blockers | 10 (5.2%) |
| Pregabalin | 2 (1.4%) |
| Decongestants | 0 |
| Medicinal formulations with high sodium content | 0 |
| Beta2-agonists | 0 |
| Itraconazole | 0 |
| Variables | 2-year (%) | P valuea |
|---|---|---|
| aLog-rank test. HD: hemodialysis; COPD: chronic obstructive pulmonary disease; SBP: systolic blood pressure; PIM: potentially inappropriate medication; NSAIDs: non-steroidal anti-inflammatory drugs; PPIs: proton pump inhibitors; Hb: hemoglobin; Alb: albumin; eGFR: estimated glomerular filtration rate. | ||
| Age ≥ 80 years | 20.6 | 0.378 |
| Male sex | 19.2 | 0.711 |
| Hypertension | 15.3 | < 0.001 |
| Diabetes mellitus | 18.5 | 0.660 |
| Dyslipidemia | 18.8 | 0.229 |
| Chronic renal disease on HD | 35.7 | 0.156 |
| Atrial fibrillation/flutter | 20.2 | 0.672 |
| Coronary artery disease | 28.1 | 0.420 |
| COPD | 43.4 | 0.028 |
| Cancer | 27.1 | 0.173 |
| SBP < 100 mm Hg | 59.2 | < 0.001 |
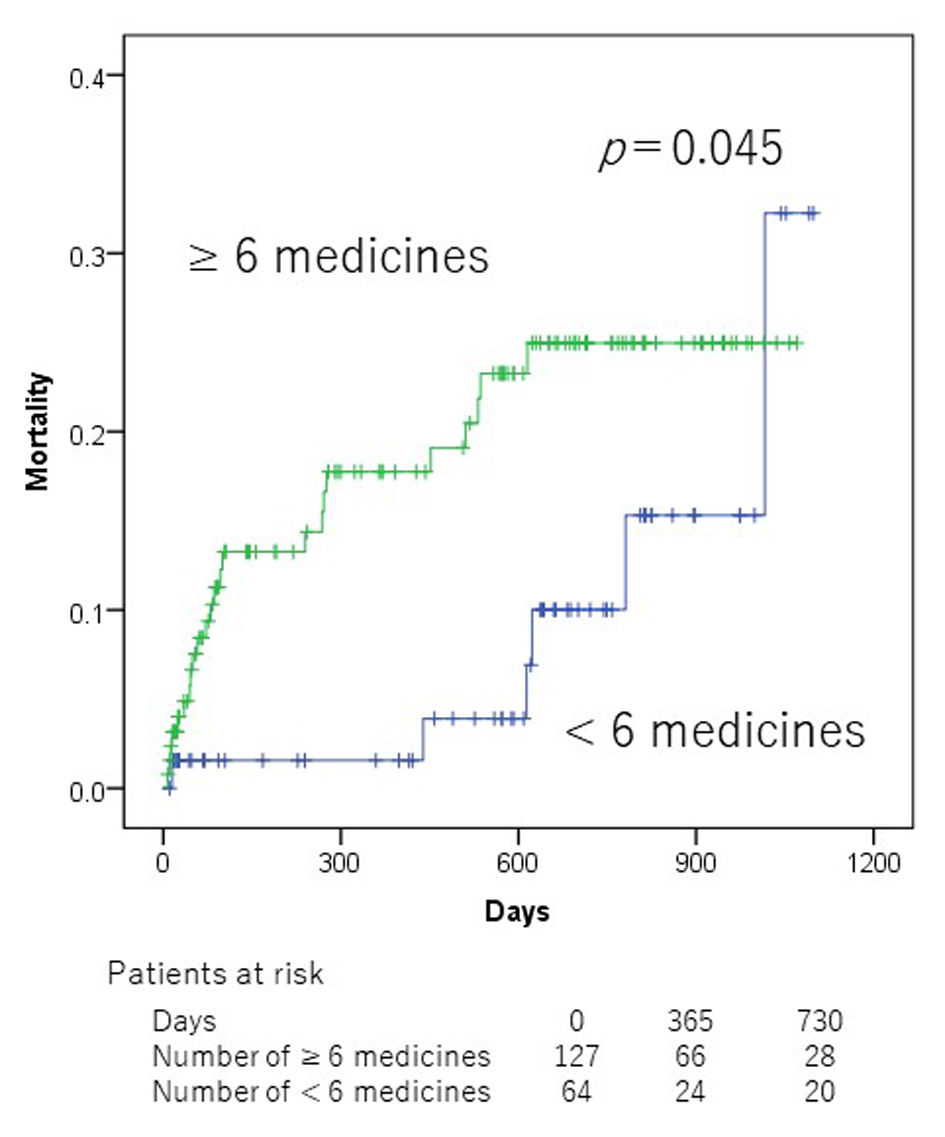
| Number of medication ≥ 6 at admission | 25.0 | 0.045 |
| Common PIMs | ||
| Benzodiazepines | 13.6 | 0.970 |
| Other than benzodiazepines | 15.4 | 0.867 |
| Sulfonylurea | 13.4 | 0.482 |
| Thiazolidinediones | 0.0 | 0.415 |
| Metformin | 16.7 | 0.806 |
| Steroid | 57.1 | 0.197 |
| NSAIDs | 39.1 | 0.002 |
| H2 antagonists | 33.9 | 0.252 |
| PPIs | 28.8 | 0.080 |
| Hb < 12 g/dL | 22.7 | 0.900 |
| Alb < 3.5 g/dL | 26.6 | 0.011 |
| eGFR < 45 mL/min/1.73 m2 | 21.5 | 0.323 |
| Prognosis factors | β | HR (95% CI) | P valuea |
|---|---|---|---|
| aCox regression for mortality. NSAIDs: non-steroidal anti-inflammatory drugs; SBP: systolic blood pressure; COPD: chronic obstructive pulmonary disease; HR: hazard ratio; CI: confidence interval. | |||
| NSAIDs, absent vs. present | 1.536 | 4.646 (1.725 - 12.510) | 0.002 |
| SBP, <100 mm Hg vs. ≥ 100 mm Hg | 1.675 | 5.341 (2.204 - 12.942) | < 0.001 |
| COPD, absent vs. present | 1.349 | 3.855 (1.417 - 10.489) | 0.008 |
| n (%), mean ± SD, non-NSAIDs (n = 179) | n (%), mean ± SD, NSAIDs (n = 14) | P value | |
|---|---|---|---|
| NSAIDs: non-steroidal anti-inflammatory drugs; SD: standard deviation; SBP: systolic blood pressure; DBP: diastolic blood pressure; eGFR: estimated glomerular filtration rate; Alb: albumin; PPIs: proton pump inhibitors. | |||
| Age (years) | 80.5 ± 7.5 | 83.8 ± 7.1 | 0.112 |
| Sex (male) | 103 (57.5%) | 6 (42.9%) | 0.286 |
| Number of medications at admission | 6.9 ± 4.0 | 9.6 ± 4.1 | 0.013 |
| SBP (mm Hg) at admission | 138.4 ± 31.8 | 139.7 ± 39.1 | 0.881 |
| DBP (mm Hg) at admission | 76.8 ± 22.0 | 81.2 ± 23.7 | 0.497 |
| eGFR (mL/min/1.73 m2) | 42.2 ± 21.6 | 43.6 ± 17.3 | 0.800 |
| Alb (g/dL) | 3.5 ± 0.5 | 3.3 ± 0.4 | 0.207 |
| PPIs, present | 79 (44.1%) | 8 (57.1%) | 0.346 |
| All-cause mortality | 25 (14.0%) | 5 (35.7%) | 0.031 |