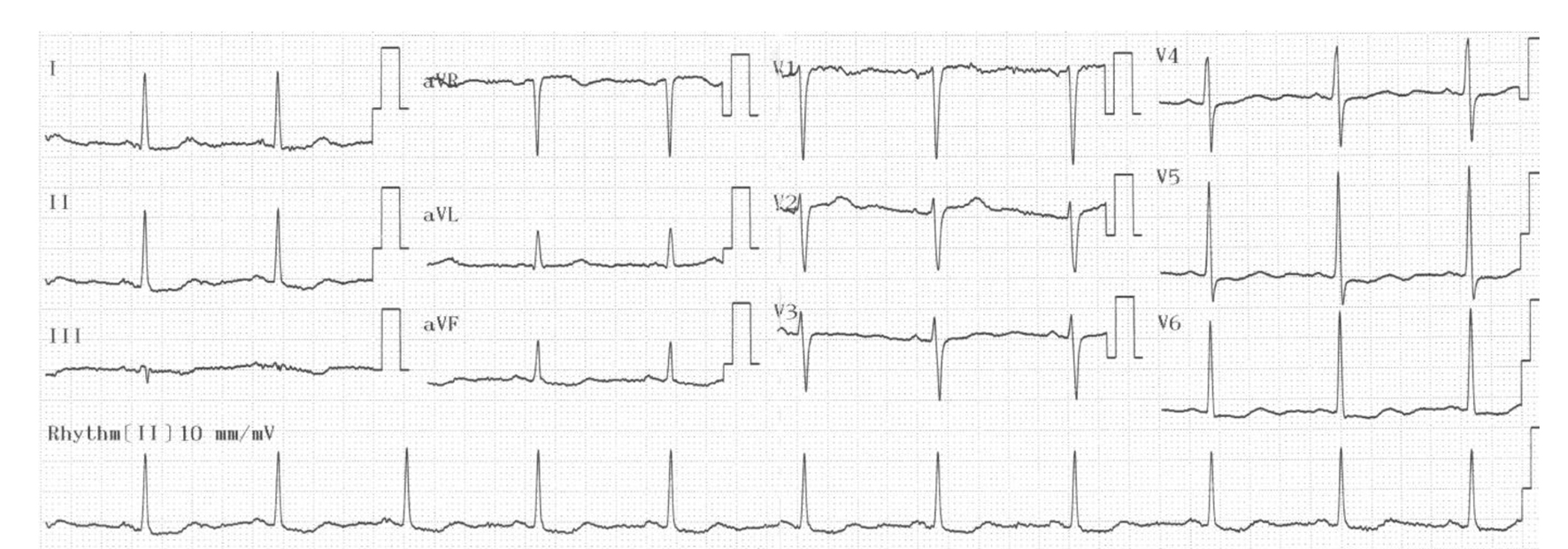
Figure 1. Baseline ECG showing a sinus rhythm along with ST depression on inferolateral derivations without evidence of conduction disorder.
| Cardiology Research, ISSN 1923-2829 print, 1923-2837 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, Cardiol Res and Elmer Press Inc |
| Journal website https://www.cardiologyres.org |
Case Report
Volume 8, Number 3, June 2017, pages 123-127
Ticagrelor-Associated Conduction Disorder: A Case Report and Review of the Literature
Figures

Table
| Author | Age/sex | Time from ticagrelor intake to onset of cardiac arrhythmia or related symptoms | Symptoms | ECG | The underlying disease | Treatment | Pre-existing conduction disease and/or AV blocking agent |
|---|---|---|---|---|---|---|---|
| ACS: acute coronary syndrome; AVB: atrioventricular block; ECG: electrocardiography; LAD: left anterior descending artery; LBBB: left bundle branch block; LCx: left circumflex artery; M: male; NA: not applicable; NSTEMI: non-ST-elevation myocardial infarction; RBBB: right bundle branch block; RCA: right coronary artery; STEMI: ST-elevation myocardial infarction. | |||||||
| Nicol et al [5] | 39/M | 1 h | No | Ventricular pause | STEMI - LAD | Follow-up | No/atenolol |
| Goldberg et al [6] | 52/M | 4 h | Syncope | Short episodes of AVB, and ventricular pause | NSTEMI - LMCA to LCx | Hemodynamic support and temporary pacemaker | RBBB/bisoprolol |
| Goldberg et al [7] | 71/M | 3 h | Syncope | AVB, deep bradicardia, ventricular pause | STEMI - LAD | Hemodynamic support and temporary pacemaker | LBBB/bisoprolol |
| Baker et al [8] | 56/M | 1 h | Lightheadedness, diaphoresis and nausea | 1 h later: borderline first-degree AVB, 3 h later: sinus bradycardia followed by sinus arrest, and complete AVB | NSTEMI - LAD | Temporary pacemaker | No/no |
| Ozturk et al [9] | 62/M | 7 h | No | Mobitz tip-2 AVB | STEMI - RCA | Follow-up | First degree AVB/metoprolol |
| Unlu et al [10] | NA/NA | 4 h | NA | Mobitz tip-2 AVB | ACS - LCx | Permanent pacemaker | First-degree AVB/metoprolol |
| Sharma et al [11] | 55/M | 2 months | Fatigue and intermittent dizziness | Mobitz tip-2 AVB | ACS - LCx | Follow-up | Moderately first-degree AVB - RBBB/metoprolol |
| Zhang et al [12] | 74/M | 6 h | Palpitation | Atrial fibrillation | ACS - LAD | Follow-up | RBBB/bisoprolol |
| Serafino et al [13] | 51/M | 2 days after ticagrelor; few hours after ivabradine | NA | Severe sinus bradicardia and arrest | STEMI - LAD | Hemodynamic support and follow-up | NA/carvediolol and ivabradine |