| Cardiology Research, ISSN 1923-2829 print, 1923-2837 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, Cardiol Res and Elmer Press Inc |
| Journal website http://www.cardiologyres.org |
Case Report
Volume 6, Number 2, April 2015, pages 263-265
Myriad Cardiac Manifestation of Hyperhomocysteinemia
Jai Babua, b, Prashanth Kumar Malkiwodeyara, Shivashankara Tarikerea, Nanjappa Manjunath Cholenahallia
aDepartment of Cardiology, SJICS&R, Bangalore, India
bCorresponding Author: Jai Babu, Department of Cardiology, SJICS&R, 7, CM-206, 7th C Main, Ist Block Kalyan Nagar, Bangalore, 43, India
Manuscript accepted for publication April 15, 2015
Short title: Myriad Cardiac Manifestation
doi: http://dx.doi.org/10.14740/cr395w
| Abstract | ▴Top |
Homocysteine has been recognized as a risk factor for various cardiovascular manifestations including thrombosis of arterial and venous system, spontaneous dissection involving various vessels in the body including coronaries and aneurysms. Here we report a young gentleman who was diagnosed as stroke in young and found to have dilated cardiomyopathy, with left ventricular dysfunction and hyperhomocysteinemia. Now the patient was presenting with unstable angina and found to have layered left ventricular thrombus on echocardiography and spontaneous coronary artery dissection on angiography. Our patient is being followed up on optimal medical management, as he is asymptomatic with medications.
Keywords: Hyperhomocysteinemia; Layered left ventricular thrombus; Spontaneous dissection of coronary arteries
| Introduction | ▴Top |
Homocysteine has been recognized as a risk factor for various cardiac diseases including thrombosis of arterial and venous system, spontaneous dissection involving various vessels in the body including coronaries, aneurysms, and peripheral artery disease [1]. Here we report a 38-year-old gentleman who was diagnosed as stroke in young and to have dilated cardiomyopathy, with left ventricular dysfunction and peripheral artery disease and hyperhomocysteinemia. Now the patient was presenting with unstable angina and found to have layered left ventricular thrombus on echocardiography and spontaneous coronary artery dissection on angiography.
| Case Report | ▴Top |
A 38-year-old gentleman was diagnosed as stroke in young; cardiac evaluation revealed dilated cardiomyopathy with biventricular dysfunction in the past. Serum homocysteine was elevated and was diagnosed to have hyperhomocysteinemia.
This time he presented with unstable angina, NYHA class III symptoms; patient was non-compliant with medications prescribed earlier. Echocardiography revealed dilated chambers, with layered left ventricular thrombus, and biventricular dysfunction with left ventricular ejection fraction of 22% (Fig. 1).
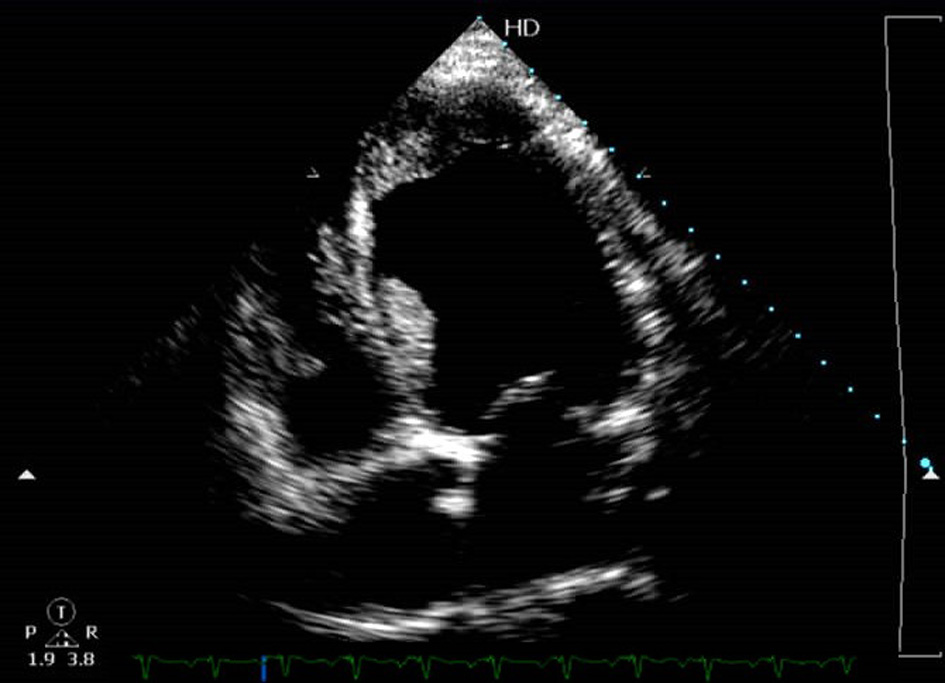 Click for large image | Figure 1. Echocardiography (apical four-chamber view) showing dilated chambers, with layered left ventricular thrombus. |
Coronary angiography showed spontaneous dissection in proximal left anterior descending artery and distal left circumflex artery (Fig. 2). Patient is being followed up on optimal medical management and regular follow-up.
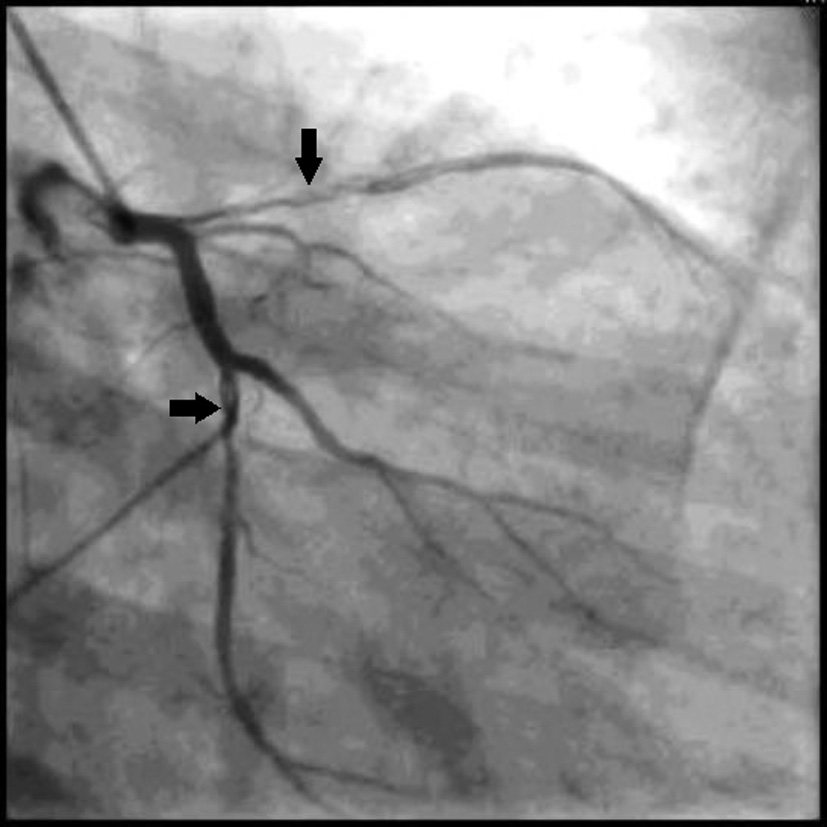 Click for large image | Figure 2. Coronary angiography showing spontaneous dissection in proximal left anterior descending artery and distal left circumflex artery. |
| Discussion | ▴Top |
Hyperhomocysteinemia incidence is estimated to be 5-7% in general population; it is a known risk factor for various vascular disorders which include coronary artery disease, venous and arterial thrombosis, peripheral vascular disease, and cerebrovascular disease [1, 2]. Hyperhomocysteinemia is associated with raised serum levels of homocysteine in general with concentrations more than 14 μmol/L but with no elimination of homocysteine in the urine [3]. Homocysteine is reflected to be noxious to vascular endothelium, leads on to arterial intimal thickening and fibrous rich plaques in smooth muscle cells and collagen relatively than typical fatty plaques noted in atherosclerosis. Further homocysteine promotes endothelial injury, postulated to be facilitated by pro-inflammatory changes, oxidative stress, and endoplasmic reticulum stress, which accordingly lead to endothelial cell injury and dysfunction [4]. Further hyperhomocysteinemia increases thrombotic tendency leading on to further endothelial cell injury, resulting in the early infarctions and death associated with this condition [4].
Hyperhomocysteinemia is associated with arterial and venous thrombus formation. Left ventricular thrombus formation can be seen to be independently associated with hyperhomocysteinemia and left ventricular dysfunction [5]. Hyperhomocysteinemia can even present as left atrial thrombus in sinus rhythm, pedunculated left ventricular mass in different case reports reported in literature [6, 7]. Our patient had layered left ventricular thrombus on echocardiography, which has not been reported in literature to our knowledge. Although biventricular dysfunction with reduced ejection fraction may be an antecedent factor in the cause of thrombus formation, homocysteinemia cannot be ruled out as one of the causative factors in this case.
There have been numerous causes associated with spontaneous coronary artery dissection like atherosclerotic plaque, peripartum period, connective tissue disorders (Marfan’s syndrome), vasculitis, after intense exertion, blunt chest trauma, cocaine abuse, hyperhomocysteinemia and idiopathic [8-12]. Hyperhomocysteinemia is related to spontaneous dissection involving aorta (aortic aneurysm), coronary, intra- and extracranial arteries and peripheral arteries [9, 13-16].
Spontaneous coronary artery dissection in coronary arteries is most frequently located in the left anterior descending coronary artery (45-75%), followed by the right coronary artery (20-33%), left circumflex coronary artery (4-19%) and left main coronary artery involved in < 1%. Left coronary artery dissections are more common in women and right coronary artery dissections occur more frequently in men [9, 10, 17]. Spontaneous coronary artery dissection can present as acute coronary syndrome, unstable angina, non-ST elevation myocardial infarction, ST-elevation myocardial infarction, or chronic stable angina [18], and can even present as refractory congestive heart failure with attempt to bridge to cardiac transplantation [19, 20].
In our case, patient had spontaneous dissection in proximal left anterior descending artery and distal left circumflex artery. This was unique case report in that both spontaneous dissections of coronary arteries present at the time of clinical presentation with unstable angina.
Recognized guidelines are not present to the treatment of patients with spontaneous coronary artery dissection at present. Treatment options include optimal medical management and revascularization with CABG or PCI. Medical management includes antiplatelets, anticoagulation, nitrates, and beta-blockers [21, 22]. Revascularization is contemplated with ongoing ischemia and is frequently treated with percutaneous intervention or surgery and is individualized [9].
Our patient is being followed up on optimal medical management, as he is asymptomatic with medications. He may be considered for myocardial perfusion imaging for inducible ischemia in future for possible coronary revascularization.
Sources of Support
Nil.
Conflict of Interest
Nil.
| References | ▴Top |
- Welch GN, Loscalzo J. Homocysteine and atherothrombosis. N Engl J Med. 1998;338(15):1042-1050.
doi pubmed - Boushey CJ, Beresford SA, Omenn GS, Motulsky AG. A quantitative assessment of plasma homocysteine as a risk factor for vascular disease. Probable benefits of increasing folic acid intakes. JAMA. 1995;274(13):1049-1057.
doi pubmed - Hackam DG, Peterson JC, Spence JD. What level of plasma homocyst(e)ine should be treated? Effects of vitamin therapy on progression of carotid atherosclerosis in patients with homocyst(e)ine levels above and below 14 micromol/L. Am J Hypertens. 2000;13(1 Pt 1):105-110.
doi - Lawrence de Koning AB, Werstuck GH, Zhou J, Austin RC. Hyperhomocysteinemia and its role in the development of atherosclerosis. Clin Biochem. 2003;36(6):431-441.
doi - Orhan AL, Okuyan E, Okcun B, Nurkalem Z, Sayar N, Soylu O, Uslu N, et al. Plasma homocysteine level and left ventricular thrombus formation in acute anterior myocardial infarction patients following thrombolytic therapy with t-PA. Thromb Res. 2009;124(1):65-69.
doi pubmed - Cattaneo P, Mariscalco G, Blanzola C, Chelazzi P, Faeli M, Sala A. [Left ventricular thrombus in a patient with antiphospholipid antibody syndrome and hyperhomocysteinemia]. Ital Heart J Suppl. 2003;4(1):54-57.
pubmed - Cupini LM, De Simone R. Hyperhomocysteinemia and left atrial thrombus in a stroke patient with sinus rhythm. Stroke. 2003;34(9):e143-145; author reply e143-145.
- DeMaio SJ, Jr., Kinsella SH, Silverman ME. Clinical course and long-term prognosis of spontaneous coronary artery dissection. Am J Cardiol. 1989;64(8):471-474.
doi - Hering D, Piper C, Hohmann C, Schultheiss HP, Horstkotte D. [Prospective study of the incidence, pathogenesis and therapy of spontaneous, by coronary angiography diagnosed coronary artery dissection]. Z Kardiol. 1998;87(12):961-970.
doi pubmed - Almeda FQ, Barkatullah S, Kavinsky CJ. Spontaneous coronary artery dissection. Clin Cardiol. 2004;27(7):377-380.
doi pubmed - Steinhauer JR, Caulfield JB. Spontaneous coronary artery dissection associated with cocaine use: a case report and brief review. Cardiovasc Pathol. 2001;10(3):141-145.
doi - Kearney P, Singh H, Hutter J, Khan S, Lee G, Lucey J. Spontaneous coronary artery dissection: a report of three cases and review of the literature. Postgrad Med J. 1993;69(818):940-945.
doi pubmed - Khandanpour N, Loke YK, Meyer FJ, Jennings B, Armon MP. Homocysteine and peripheral arterial disease: systematic review and meta-analysis. Eur J Vasc Endovasc Surg. 2009;38(3):316-322.
doi pubmed - Pezzini A, Del Zotto E, Archetti S, Negrini R, Bani P, Albertini A, Grassi M, et al. Plasma homocysteine concentration, C677T MTHFR genotype, and 844ins68bp CBS genotype in young adults with spontaneous cervical artery dissection and atherothrombotic stroke. Stroke. 2002;33(3):664-669.
doi pubmed - Duncan IC, Terblanche JM. Spontaneous isolated posterior communicating artery dissection in a young adult with hyperhomocysteinemia. AJNR Am J Neuroradiol. 2005;26(8):2030-2032.
pubmed - Narayanan N, Tyagi N, Shah A, Pagni S, Tyagi SC. Hyperhomocysteinemia during aortic aneurysm, a plausible role of epigenetics. Int J Physiol Pathophysiol Pharmacol. 2013;5(1):32-42.
pubmed - Auer J, Punzengruber C, Berent R, Weber T, Lamm G, Hartl P, Eber B. Spontaneous coronary artery dissection involving the left main stem: assessment by intravascular ultrasound. Heart. 2004;90(7):e39.
doi pubmed - Kamran M, Guptan A, Bogal M. Spontaneous coronary artery dissection: case series and review. J Invasive Cardiol. 2008;20(10):553-559.
pubmed - Conraads VM, Vorlat A, Colpaert CG, Rodrigus IE, De Paep RJ, Moulijn AC, Vrints CJ. Spontaneous dissection of three major coronary arteries subsequent to cystic medial necrosis. Chest. 1999;116(5):1473-1475.
doi pubmed - Ferrari E, Tozzi P, von Segesser LK. Spontaneous coronary artery dissection in a young woman: from emergency coronary artery bypass grafting to heart transplantation. Eur J Cardiothorac Surg. 2005;28(2):349-351.
doi pubmed - Zampieri P, Aggio S, Roncon L, Rinuncini M, Canova C, Zanazzi G, Fiorencis R, et al. Follow up after spontaneous coronary artery dissection: a report of five cases. Heart. 1996;75(2):206-209.
doi pubmed - Sarmento-Leite R, Machado PR, Garcia SL. Spontaneous coronary artery dissection: stent it or wait for healing? Heart. 2003;89(2):164.
doi pubmed
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cardiology Research is published by Elmer Press Inc.











